Abstract
Background
Infections in kidney transplant recipients are particularly challenging owing to the immunosuppressive treatment, usually long history of chronic illness, comorbidities and prior exposures to antibiotics. Among the most common complications early after surgery are surgical site infections. The aim of this study was to identify risk factors and evaluate epidemiological data regarding surgical site infections. Moreover, we were able to compare the current results with historical data from our institution when different perioperative antibiotic prophylaxis was practiced.
Methods
We conducted a retrospective case–control study in a group of 254 deceased donor renal graft recipients transplanted in a single Central European institution. We evaluated epidemiological findings and resistance patterns of pathogens causing surgical site infections. We used multivariable logistic regression to determine risk factors for surgical site infections.
Results
We revealed no differences in baseline characteristics between patients with and without surgical site infections. Ten surgical site infections (3.9%) were diagnosed (six superficial incisional, two deep incisional, and two organ/space). Eight species (19 strains) were identified, most of which were multi-drug resistant (63%). The most common was extended-spectrum β-lactamase producing Klebsiella pneumoniae (26%). We showed that statistically significant differences were present between reoperated and non-reoperated patients (adjusted odds ratio: 6.963, 95% confidence interval 1.523–31.842, P = .012).
Conclusions
Reoperation is an individual risk factor for surgical site infection after kidney transplantation. According to our experience, cefazolin-based prophylaxis can be safe and is associated with relatively low prevalence of surgical site infections.
Similar content being viewed by others
Background
Surgical site infection is one of the most common nosocomial infections and a considerable cause of morbidity, prolonged hospitalization, and higher costs of medical care [1,2,3]. Solid organ transplant recipients are particularly susceptible to this complication mainly owing to their immunosuppressive treatment, usually long history of chronic illness, comorbidities and prior exposures to antibiotics.
Despite the progress in infection control practices and the development of perioperative antibiotic prophylaxis strategies, surgical site infections remain among the most challenging problems in the early period after kidney transplantation. Transplant teams may implement many preventive strategies at each stage of medical care to mitigate the risk of wound contamination, one of which is perioperative antibiotic prophylaxis [4, 5]. There is no single universal protocol and each transplant center should optimize their prophylaxis according to the local resistance patterns as well as the infection and colonization status of both the donor and recipient [6]. It is estimated that surgical site infections occur in 3% to 11% of renal graft recipients [4].
In this study, we aimed to retrospectively identify risk factors and epidemiological data associated with posttransplant surgical site infections. We also shared our single-center Central European country experience with a new perioperative antibiotic prophylaxis protocol that was modified after publishing our previous report [7].
Methods
Study design and eligibility criteria
As a continuation of our previous research, we maintained similar assumptions and research methods that we used before [7]. We conducted a retrospective case–control study in deceased donor renal graft recipients. We included adult patients transplanted or retransplanted between October 2015 and August 2018 in the Department of General and Transplantation Surgery at the Medical University of Warsaw, Poland. The exclusion criteria were: multi-organ transplantation, early (up to 7 days from the hospital admission) in-hospital death or graftectomy not related to surgical site infection, and the use of Bricker ileal conduit. The reporting of our study conforms to the STROBE statement [8].
Setting and data collection
All study participants were observed for at least 1 year after transplantation or until their death or graft loss. Medical records were analyzed to collect the following data: donors’ and recipients’ demographic data (age, sex, body mass, and height), comorbidities, and renal function. We identified the cause of donors’ death, time spent at the intensive care unit, the need to use catecholamines, presence of any type of infection (urine, blood, intubation tube, and preservation fluid cultures were collected). We retrieved data about the method of organ storage, cold and warm ischemic times, and the length of transplant procedure. Information regarding the studied patients included also: the use, modality, and dialysis vintage, past medical and transplant history, number of HLA mismatches with the received organ, details about immunosuppressive treatment, posttransplant renal function, and complications (surgical site and/or urinary tract infections, surgical procedures, delayed graft function, primary non-function, and episodes of biopsy-proven acute rejection).
Surgical site infection was determined in line with the Centers for Disease Control and Prevention definition [9]. It was stratified into superficial incisional, deep incisional, and organ/space infection [10]. Delayed graft function was defined as the need for dialysis within the first posttransplant week [11]. Primary graft non-function was diagnosed when persistent lack of transplanted kidney function was observed and the patient was dialysis-dependent immediately after surgery. Biopsy-proven acute rejection was identified and classified in compliance with the Banff 2017 criteria [12].
Analysis of microbiological results
Wound swabs were obtained when surgical site infection was suspected or when it was advised by a transplant nephrologist, including cases where graft preservation fluid cultures were positive. Isolates were identified and characterized using standard microbiological methods. Samples were cultured under aerobic and anaerobic conditions at 35–37 °C for 24–48 h with commercially available blood agar (Difco, Detroit, MI, USA) and MacConkey agar (bioMérieux, Marcy l'Etoile, France). Schaedler (bioMérieux) and liquid medium Schaedler (bioMerieux) were used for aerobic culture. Anaerobic strains were cultured in the anaerobic chamber. Sabouraud Agar (Difco) was used for the fungi culture. Biochemical characteristics of culture strains were evaluated using API and/or BioMerieux ID, according to manufacturer’s instructions. We investigated the antibiotic sensitivity of cultured strains using the ATB (bioMerieux) system according to recommendations of the Clinical and Laboratory Standards Institute (CLSI) [13] and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [14]. We also performed additional testing procedures for multi-drug resistant strains (classified in line with the 2019 CDC Antibiotic Resistance Threats Report) [15]. The strains’ antibiotic sensitivity analysis was carried out for microorganisms pathogenic to humans.
Organ preservation prior to transplant
Renal grafts were recovered in hospitals outside our transplantation center. Immediately after organ recovery and cooling to 4 °C, most kidneys were preserved by simple hypothermic storage in the University of Wisconsin solution and transported in a thermally stable container. Hypothermic machine perfusion was utilized when the following factors were present: poor in situ perfusion, use of kidney from an extended criteria donor, considerable risk of acute kidney injury, and anticipated cold ischemic time exceeding 24 h. The decision to use machine perfusion was limited by the availability of a disposable organ cassette and machine preservation fluid.
Perioperative antibiotic prophylaxis
Patients undergoing kidney transplantation received a standard perioperative antibiotic prophylaxis that was adapted in our center since October 2015. Each recipient was given a 2.0 g single-dose first generation cephalosporin (cefazolin) via an intravenous infusion 30 min before the first skin incision. Additionally, all patients received oral sulfamethoxazole–trimethoprim (480 mg daily starting on the 4th postoperative day) as a Pneumocystis pneumonia prophylaxis.
Transplant procedure
Kidneys were transplanted using the standard approach. Graft vessels were anastomosed end-to-side to external iliac vessels either on the left or right side. Lich-Gregoir technique was used for the ureterovesical anastomosis.
Immunosuppressive treatment
Standard immunosuppressive regimen consisted of calcineurin inhibitor (either tacrolimus or cyclosporine started at an oral dose of 0.2 mg/kg and 10 mg/kg, respectively), prednisolone (started simultaneously with the vascular anastomosis at intravenous dose of 250 mg or 500 mg, depending on the patient’s weight), and mycophenolate mofetil or sodium (1.0 g and 720 mg twice daily, respectively). Calcineurin inhibitors’ doses were halved on the second posttransplant day and the subsequent dosing was dependent on the regular blood concentration monitoring. Prednisone was continued at the dose of 125 mg every 12–24 h until the third postoperative day when its oral supplementation was started (at an initial dose of 20 mg/day that was gradually lowered to reach the dose of 10–15 mg/day on the 30th day after surgery). Patients with panel reactive antibody scores exceeding 20% and/or with at least four HLA mismatches were given an induction immunosuppression therapy with thymoglobuline or basiliximab.
Outcomes and study groups
We divided all patients into two groups: “SSI” with recipients who developed surgical site infection and “non-SSI” including those without that complication. Cases were defined as all patients with surgical site infections identified within the study period. Cases consisted of all remaining renal graft recipients who did not have surgical site infection within that time. No matching was planned for this study. Our main goal was to identify potential risk and/or protective factors for surgical site infection.
Statistical analysis
The assumption of normal distribution, evaluated with the Shapiro–Wilk test, was not fulfilled for any of the continuous variables. Thus their medians with ranges were reported. For categorical variables, frequencies and percentages were presented. Mann–Whitney U test was applied to compare continuous variables between the SSI and non-SSI groups. For categorical variables, differences between the groups were assessed with the Chi-square or Fisher’s exact tests, as appropriate. Multivariable logistic regression was used to identify the predictors of surgical site infections as well as to identify and adjust for potential confounding factors. Backward elimination with a P value criterion of .157 was used [16, 17]. Missing data were deleted pairwise. P < .05 was regarded as statistically significant. All analyses were performed in the R statistical environment, version 4.0.0 (R Core Team, 2020) [18].
Ethical approval was obtained from the Bioethics Committee at the Medical University of Warsaw (KB239/2013).
Results
Study participants
Between October 2015 and August 2018, 285 patients were transplanted in our unit. 31 of them were excluded due to multi-organ transplantation (8 patients), early in-hospital death or graftectomy not related to surgical site infection (4 cases), the use of Bricker ileal conduit (2 individuals), and other reasons (living donor transplants, loss to follow-up, and missing data). In result, 254 graft recipients were included in the final analysis.
The study population consisted of 87 women and 167 men. The median age of the participants was 50 (range, 18–78). They received renal grafts from deceased donors with the median age of 52 (range, 5–80). Five of them received their kidneys from a pediatric donor (age less than 18 years old). Only one patient was treated with cyclosporine while others received tacrolimus. The organs were stored in simple hypothermia in 219 cases and with the use of machine perfusion in 29 (in 6 individuals the storage modality was unknown or mixed). The donor- and recipient-related characteristics (demographics, comorbidities, past medical history, transplanted organ characteristics, renal function, and transplant procedure details with outcomes) are presented in Tables 1, 2, and 3.
Ten patients were diagnosed with surgical site infection and thus included in the SSI group. The non-SSI group consisted of 244 patients. The baseline characteristics between the two cohorts were compared and no statistically significant differences were noted apart from the size of each group (Tables 1, 2, and 3). Having met the predefined study requirements, we proceeded to the further analysis.
Primary outcome
Clinically- and laboratory-confirmed surgical site infections were observed in 10 patients (10/254, 3.9%). Six patients were diagnosed with superficial incisional (6/10, 60%), two with deep incisional (2/10, 20%), and two with organ/space infection (2/10, 20%). What we observed is that surgical site infections occurred mainly in patients with complications that often required reoperation before being diagnosed with surgical site infection (P = .002). Four patients were diagnosed with primary surgical site infection, three had an urinary complication, in two the pathogens were transferred with the transplanted organ, and one had an iatrogenic complication (colon perforation during the initial skin incision). We summarized the findings in those patients in Table 4.
Superficial incisional infections were treated with intravenous antibiotics, surgical debridement, and secondary wound closure was performed (except in one case when vacuum therapy with subsequent secondary wound sewing was implemented). Initially empirical antibiotic treatment was adjusted depending on the microbiological findings.
The two recipients with deep incisional infections were treated similarly but both underwent the vacuum therapy. One patient developed fascial disruption that was managed surgically.
Organ/space infections were all successfully treated with adequate antibiotics (carbapenem with vancomycin; linezolid was used only once), surgical (including fascial repair), and vacuum therapies. We identified major complications that are suspected to cause the infection in the two individuals: iatrogenic caecal perforation in one case and urinary anastomosis complication in the second (Table 4).
Surgical site infections—etiopathology
In Table 5, we present the list of pathogens detected by wound swabs collected from the SSI patients. Microbiological analyses revealed the presence of eight bacterial species (19 strains). The most common was extended-spectrum β-lactamase (ESBL) producing Klebsiella pneumoniae (five isolates, 26%). Ten out of 14 (71%) Gram negative pathogens were ESBL positive. 12 strains (12/19, 63%) were multi-drug resistant [15]. In two recipients surgical site infections were caused by bacteria transferred with the grafts (the same pathogen, Acinetobacter baumannii, was detected in the preservation fluid and wound swab specimens). One of them developed deep incision infection and required reoperation followed by vacuum therapy and antibiotics. The second had superficial infection cured successfully with conservative antibiotic treatment.
Transplant outcomes
There was no difference in the occurrence of delayed graft function, primary non-function, and creatinine serum levels between the analyzed groups after transplantation (Table 3). Appearance of hematoma in the operated area strongly correlated with the occurrence of surgical site infection (P = .012). Moreover, surgical site infections were more frequent if reoperation in the early posttransplant period was performed (P = .002).
Risk factors for surgical site infection
We performed a multivariable logistic regression analysis to identify the risk factors for surgical site infections (Table 6). It resulted in the inclusion of two exposures in the model: reoperation and presence of hematoma in the operated area. Although the two variables are correlated, χ2 (1, n = 198) = 13.217, P < .001, both could be included owing to the low value of variance inflation factor (VIF = 1.075). Additionally, BMI was included in that model as a known confounding factor. Therefore, we showed that there are statistically significant differences between reoperated and non-reoperated patients (adjusted odds ratio: 6.963, 95% confidence interval 1.523–31.842, P = .012).
Discussion
In this study, we summarized our experience with surgical site infections and perioperative antibiotic prophylaxis consisting of the first generation cephalosporin administered at a single dose 30 min prior to the initial skin incision. In the studied group of 254 deceased donor renal graft recipients, 10 (3.9%) developed surgical site infection. We calculated that reoperation adjusted for the presence of hematoma in the surgical site and BMI is a risk factor for this challenging complication (adjusted odds ratio: 6.963, 95% confidence interval 1.523–31.842, P = .012).
Surgical site infections occur in 3% to 11% of patients after kidney transplantation [3,4,5, 9, 19]. The prevalence of 3.9% in our transplant unit seems, therefore, to be relatively low. Even though the complication rarely leads to graft loss, it is proved to significantly increase morbidity and prolonged hospitalization time [20].
The identification of certain surgical site infection risk factors has been a significant problem for years as the conclusions vary in different publications. Most of them mention body mass index (BMI), immunosuppression regimen, older age, diabetes and accompanying heart diseases, cold ischemic time, duration of surgical procedure, and delayed graft function [20,21,22,23]. In this study, we aimed to verify those findings and identify potentially new predicting factors based on our experience.
While evaluating the impact of BMI on surgical site infections, we expected that patients with a higher BMI would acquire more episodes of surgical site infections. Obese patients are proved to have an increased prevalence of postoperative wound colonization, as demonstrated by multiple studies [24,25,26,27]. Some data on intraabdominal surgery show that especially the thicker subcutaneous fat tissue is related with higher wound morbidity [28]. In our study, we observed that the median BMI was higher in patients with surgical site infections compared to those without infection but the difference was not statistically significant (28.0 vs 25.0, U = 842.0, P = .096). However, BMI was indeed confirmed to be an important confounding factor that was included in our final logistic regression model.
Literature clearly confirms that patients with more intense immunosuppression are expected to acquire more surgical site infections [25]. In current study, each patient received the same, triple-drug immunosuppressive treatment, and almost 88% (224/254) of them did not receive antibody induction. As the protocol was universal, no differences could be found between the studied groups and we could not identify more intensive immunosuppression to be a predisposing risk factor for SSI. Similar conclusions can be drawn regarding patients’ age. However, reoperation was confirmed as a major risk factor for surgical site infection [25, 29]. It is most likely caused due to increased exposure of the surgical site on contamination [20]. In such circumstances, the immunocompromising influence of anti-rejection drugs worsens the outcomes [29]. We detected that the presence of a hematoma in the operated area also predisposes to the development of infection. This is not a frequent observation in the literature. In fact, the two variables (hematoma and reoperation) are correlated (not strongly, VIF = 1.075) as often they can cause one another. The multivariable logistic regression analysis confirmed that reoperation is an independent risk factor for surgical site infection. Therefore, we provided an odds ratio adjusted for the occurrence of hematoma in the surgical site and patient’s BMI. That leads us to the point, where in the future, this observation may be helpful in postoperative estimation of the risk of infection wound problems.
Evidence of the beneficial role of perioperative antibiotic prophylaxis in reducing postoperative surgical site infections in solid organ recipients is well-established [5, 7, 19]. Only a few reports question its efficacy [9, 30]. However, specific antibiotic regimens and durations vary widely across transplant centers and procedures, and the quality of the evidence supporting specific practices is quite poor [5, 31,32,33]. Currently, there are no strict formal recommendations on perioperative antibiotic prophylaxis administration in kidney recipients. According to the IDSA/ASHP/SIS/SHEA guidelines, each transplant center should customize their own protocol that corresponds with their unique microbiological setting (patients’ and donor’s colonization statuses, local resistance patterns, and presence of nosocomial pathogens) [5]. It should also be pointed out that such prophylaxis can lead to some problems including increased: financial costs, rates of Clostridioides difficile colonization and colitis, incidence of antimicrobial resistance, and other adverse events [34,35,36,37]. Thus, targeted antibiotics should be used in each case based on individual risk factors and local patterns of resistance [38,39,40]. Moreover, the spectrum of organisms involved in SSI in kidney recipients is more diverse than for the general population due to other important factors such as the underlying end‐stage organ failure, immunosuppression, prolonged hospitalization, organ transportation/preservation, and previous exposures to antibiotics in donors and recipients that could predispose to infections with multi-drug resistant organisms [15]. Therefore, the use of antibiotic prophylaxis should be optimized as to be truly effective yet still minimal as to restrain the spread of multi-drug resistant pathogens. As we modified our local protocol a few years earlier, we had a unique chance to compare our historical data with the current ones.
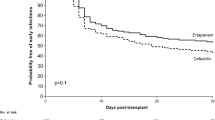
Before October 2015 our strategy was to administer 2.0 g of the third generation cephalosporin (ceftriaxone) in a single infusion 30 min prior to the first skin incision. We observed back then that surgical site infections occurred in 12 of 214 patients (5.6%) [7]. The historic incidence is slightly higher, although we think that the difference is not clinically significant. This finding is very satisfying as we started using an antibiotic with a narrower spectrum and achieved similar results. We hope that such an approach can at least minimally help to decrease the risk of development of new multi-drug resistant strains. Similar conclusions were demonstrated by other authors [4, 21]. Furthermore, other factors like: shortening surgical operative time, optimal sterile technique, proper perioperative management of patients’ comorbidities as well as good glucose and temperature regulation, are also assumed to be imperative to limit surgical site infections but those elements were outside the scope of our research [41,42,43,44,45].
Limitations
The main limitations of our study are the limited number of cases and the retrospective, non-randomized design carried out at a single Central European institution. The incompleteness of medical records resulted in the presence of some missing data. Therefore, we cannot exclude bias due to missing data. Another bias that might be present in such case–control study is caused by confounding [46]. We attempted to eliminate it by restriction (e.g., we excluded patients with Bricker ileal conduit due to significant deviation from a standard kidney transplant procedure that carries a higher risk for surgical site infection) and multivariable logistic regression (i.e., we calculated adjusted odds ratio).
Another limitation is related to the lack of definition of minimal clinically important difference (MCID) regarding the comparison of different perioperative antibiotic prophylaxis regimens. Such a concept would help transplant centers to confirm when a change in their perioperative antibiotic prophylaxis is reasonable. We were able to compare our current prophylaxis policy to the previous one concerning the prevalence of surgical site infection, although it was not the main scope of our study. We conclude that the decrease in prevalence of surgical site infection of 1.7% is not clinically relevant [47]. The difference is also not statistically significant (data not shown) which increases our confidence in that matter. However, if MCIDs were defined by transplant societies regarding the outcomes of perioperative antibiotic prophylaxis, it could possibly improve the process of choosing the most optimal regimen in each transplant center [48].
Conclusions
In conclusion, our study identifies reoperation as a strong risk factor for surgical site infection. Hematoma in the operated area also correlates with higher incidents of this complication. Our positive experience with single-dose cefazolin-based perioperative antibiotic prophylaxis shows that it can be a safe and effective method that in our unit is associated with relatively low prevalence of SSI (3.9%).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- ESBL:
-
Extended-spectrum β-lactamase
- HLA:
-
Human leukocyte antigen
- SSI:
-
Surgical site infection
- VIF:
-
Variance inflation factor
References
Magill SS, Hellinger W, Cohen J, Kay R, Bailey C, Boland B, et al. Prevalence of healthcare-associated infections in acute care hospitals in Jacksonville, Florida. Infect Control Hosp Epidemiol. 2012;33(3):283–91.
Awad SS. Adherence to surgical care improvement project measures and post-operative surgical site infections. Surg Infect Larchmt. 2012;13(4):234–7.
Anderson DJ, Podgorny K, Berríos-Torres S, Bratzler D, Dellinger EP, Greene L, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(Suppl 2):66–88.
Abbo LM, Grossi PA. Surgical site infections: guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13589.
Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health-Syst Pharm. 2013;70(3):195–283.
Malinis M, Boucher HW, on behalf of the AST Infectious Diseases Community of Practice. Screening of donor and candidate prior to solid organ transplantation—Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13548.
Ostaszewska A. Reoperation in early kidney post-transplant period as a strong risk factor of surgical site infection occurrence. Transplant Proc. 2019;51(8):2724–30.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
Mangram AJ, Horan T, Pearson M, Silver L, Jarvis W. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27(2):97–132, 133–4, 96.
Viehman JA, Clancy CJ, Clarke L, Shields RK, Silveira FP, Kwak EJ, et al. Surgical site infections after liver transplantation: emergence of multidrug-resistant bacteria and implications for prophylaxis and treatment strategies. Transplantation. 2016;100(10):2107–14.
Yarlagadda SG, Coca SG, Garg AX, Doshi M, Poggio E, Marcus RJ, et al. Marked variation in the definition and diagnosis of delayed graft function: a systematic review. Nephrol Dial Transplant. 2008;23(9):2995–3003.
Roufosse C, Simmonds N, Clahsen-van Groningen M, Haas M, Henriksen KJ, Horsfield C, et al. A 2018 reference guide to the Banff classification of renal allograft pathology. Transplantation. 2018;102(11):1795–814.
Melvin PW. M100 performance standards for antimicrobial susceptibility testing. 31st ed. 2021.
EUCAST. Clinical breakpoints and dosing of antibiotics. https://eucast.org/clinical_breakpoints/. Accessed 10 Apr 2021.
Centers for Disease Control and Prevention (U.S.). Antibiotic resistance threats in the United States, 2019. Centers for Disease Control and Prevention (U.S.); 2019. http://www.cdc.gov/DrugResistance/Biggest-Threats.html. Accessed 23 July 2021.
Heinze G, Dunkler D. Five myths about variable selection. Transpl Int. 2017;30(1):6–10.
Heinze G, Wallisch C, Dunkler D. Variable selection—a review and recommendations for the practicing statistician. Biom J. 2018;60(3):431–49.
R Core Team. R: a language and environment for statistical computing. 2020. https://www.R-project.org/.
Kirkland KB, Briggs J, Trivette S, Wilkinson W, Sexton D. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20(11):725–30.
Capocasale E, Vecchi E, Mazzoni M, Valle R, Pellegrino C, Ferretti S, et al. Surgical site and early urinary tract infections in 1000 kidney transplants with antimicrobial perioperative prophylaxis. Transplant Proc. 2014;46(10):3455–8.
Orlando G, Manzia T, Sorge R, Iaria G, Angelico R, Sforza D, et al. One-shot versus multidose perioperative antibiotic prophylaxis after kidney transplantation: a randomized, controlled clinical trial. Surgery. 2015;157(1):104–10.
Wszola M, Kwiatkowski A, Ostaszewska A, Górski Ł, Kuthan R, Sawicka-Grzelak A, et al. Surgical site infections after kidney transplantation—where do we stand now? Transplantation. 2013;95(6):878–82.
Pham PT, Danovitch GM, Pham PC. Kidney transplantation in the obese transplant candidates: to transplant or not to transplant? Semin Dial. 2013;26(5):568–77.
Lynch RJ, Ranney D, Shijie C, Lee D, Samala N, Englesbe M. Obesity, surgical site infection, and outcome following renal transplantation. Ann Surg. 2009;250(6):1014–20.
Humar A, Ramcharan T, Denny R, Gillingham K, Payne W, Matas A. Are wound complications after a kidney transplant more common with modern immunosuppression? Transplantation. 2001;72(12):1920–3.
Goel M, Flechner S, Zhou L, Mastroianni B, Savas K, Derweesh I, et al. The influence of various maintenance immunosuppressive drugs on lymphocele formation and treatment after kidney transplantation. J Urol. 2004;171(5):1788–92.
Zrim S, Furlong T, Grace B, Meade A. Body mass index and postoperative complications in kidney transplant recipients. Nephrol Carlton. 2012;17(6):582–7.
Fujii Y, Shimada K, Maru K, Ozawa J, Lu R. A method for direct measurement of the first-order mass moments of human body segments. Sens Basel. 2010;10(10):9155–62.
Menezes F, Wey S, Peres C, Medina-Pestana J, Camargo L. Risk factors for surgical site infection in kidney transplant recipients. Infect Control Hosp Epidemiol. 2008;29(8):771–3.
Ben-Ami R, Rodríguez-Baño J, Arslan H, Pitout J, Quentin C, Calbo E, et al. A multinational survey of risk factors for infection with extended-spectrum beta-lactamase-producing enterobacteriaceae in nonhospitalized patients. Clin Infect Dis. 2009;49(5):682–90.
Chadban SJ. KDIGO clinical practice guideline on the evaluation and management of candidates for kidney transplantation. Transplantation. 2020;104(4S1 Suppl 1):11–103.
Chadban SJ, Barraclough K, Campbell S, Clark C, Coates P, Cohney S, et al. KHA-CARI guideline: KHA-CARI adaptation of the KDIGO clinical practice guideline for the care of kidney transplant recipients. Nephrol Carlton. 2012;17(3):204–14.
Baker RJ, Mark P, Patel R, Stevens K, Palmer N. Renal association clinical practice guideline in post-operative care in the kidney transplant recipient. BMC Nephrol. 2017;18(1):174.
Kreisel D, Savel T, Silver A, Cunningham J. Surgical antibiotic prophylaxis and Clostridium difficile toxin positivity. Arch Surg. 1995;130(9):989–93.
Privitera G, Scarpellini P, Ortisi G, Nicastro G, Nicolin R, de Lalla F. Prospective study of Clostridium difficile intestinal colonization and disease following single-dose antibiotic prophylaxis in surgery. Antimicrob Agents Chemother. 1991;35(1):208–10.
Jobe BA, Grasley A, Deveney K, Deveney C, Sheppard B. Clostridium difficile colitis: an increasing hospital-acquired illness. Am J Surg. 1995;169(5):480–3.
Roberts NJ Jr, Douglas RG Jr. Gentamicin use and Pseudomonas and Serratia resistance: effect of a surgical prophylaxis regimen. Antimicrob Agents Chemother. 1978;13(2):214–20.
Safdar N, Maki DG. The commonality of risk factors for nosocomial colonization and infection with antimicrobial-resistant Staphylococcus aureus, enterococcus, gram-negative bacilli, Clostridium difficile, and Candida. Ann Intern Med. 2002;136(11):834–44.
Patel G, Huprikar S, Factor S, Jenkins S, Calfee D. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008;29(12):1099–106.
Linares L, Cervera C, Cofán F, Esforzado N, Terregrosa V, Oppenheimer F, et al. Epidemiology and outcomes of multiple antibiotic-resistant bacterial infection in renal transplantation. Transpl Proc. 2007;39(7):2222–4.
Cima R, Dankbar E, Lovely J, Pendlimari R, Aronhalt K, Nehring S, et al. Colorectal surgery surgical site infection reduction program: a national surgical quality improvement program-driven multidisciplinary single-institution experience. J Am Coll Surg. 2013;216(1):23–33.
Tang R, Chen H, Wang Y, Changchien C, Chen J, Hsu K, et al. Risk factors for surgical site infection after elective resection of the colon and rectum: a single-center prospective study of 2,809 consecutive patients. Ann Surg. 2001;234(2):181–9.
Darouiche RO, Wall M Jr, Itani K, Otterson M, Webb A, Carrick M, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
McConkey SJ, L’Ecuyer P, Murphy D, Leet T, Sundt T, Fraser V. Results of a comprehensive infection control program for reducing surgical-site infections in coronary artery bypass surgery: further data from the authors. Infect Control Hosp Epidemiol. 1999;20(12):791–2.
Park C, Hsu C, Neelakanta G, Nourmand H, Braunfeld M, Wray C, et al. Severe intraoperative hyperglycemia is independently associated with surgical site infection after liver transplantation. Transplantation. 2009;87(7):1031–6.
Schulz KF, Grimes DA. Case-control studies: research in reverse. Lancet Lond Engl. 2002;359(9304):431–4.
van Rijn MHC, Bech A, Bouyer J, van den Brand JAJG. Statistical significance versus clinical relevance. Nephrol Dial Transplant. 2017;32(suppl_2):ii6-12.
McGlothlin AE, Lewis RJ. Minimal clinically important difference: defining what really matters to patients. JAMA. 2014;312(13):1342–3.
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
AO and PD were responsible for study design, data collection, data interpretation, and manuscript preparation. MZ was involved in study design, data collection, statistical analysis, data interpretation, and manuscript preparation. EK participated in acquisition data. MW participated in study design and data interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
It is included as a part of the formal ethics approval. It was obtained from the Bioethics Committee at the Medical University of Warsaw (KB239/2013). The data used in this study was anonymized before its use. Administrative permissions to access the raw data used are included as a part of the formal ethics approval.
Consent for publications
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ostaszewska, A., Domagała, P., Zawistowski, M. et al. Single-center experience with perioperative antibiotic prophylaxis and surgical site infections in kidney transplant recipients. BMC Infect Dis 22, 199 (2022). https://doi.org/10.1186/s12879-022-07182-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07182-z