Abstract
Metabolic bone disorders arise as primary diseases or may be secondary due to a multitude of organ malfunctions. Animal models are required to understand the molecular mechanisms responsible for the imbalances of bone metabolism in disturbed bone mineralization diseases. Here we present the isolation of mutant mouse models for metabolic bone diseases by phenotyping blood parameters that target bone turnover within the large-scale genome-wide Munich ENU Mutagenesis Project. A screening panel of three clinical parameters, also commonly used as biochemical markers in patients with metabolic bone diseases, was chosen. Total alkaline phosphatase activity and total calcium and inorganic phosphate levels in plasma samples of F1 offspring produced from ENU-mutagenized C3HeB/FeJ male mice were measured. Screening of 9,540 mice led to the identification of 257 phenodeviants of which 190 were tested by genetic confirmation crosses. Seventy-one new dominant mutant lines showing alterations of at least one of the biochemical parameters of interest were confirmed. Fifteen mutations among three genes (Phex, Casr, and Alpl) have been identified by positional-candidate gene approaches and one mutation of the Asgr1 gene, which was identified by next-generation sequencing. All new mutant mouse lines are offered as a resource for the scientific community.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metabolic bone diseases originate from endocrine dysfunctions as well as from heterogeneous determinants, including age, life style, and environmental influences. Bone turnover is physiologically regulated by hormones, cytokines, and growth factors and is under the control of numerous signaling pathways (Chavassieux et al. 2007). Metabolic diseases may have primary or secondary impact on bone mineralization. For investigating disease development and progression and to understand the underlying mechanisms, mice have been shown to serve successfully as model organisms (e.g., Abe et al. 2007; Kurima et al. 2002; Marklund et al. 2010; McGowan et al. 2008). Random N-ethyl-N-nitrosourea (ENU) mutagenesis is a promising approach to obtain mouse models for inherited human diseases (Hrabě de Angelis and Balling 1998). This has been shown in worldwide ENU mutagenesis programs, including bone metabolism, using dual-energy X-ray absorptiometry (DEXA), X-ray analysis, biochemical markers, or the SHIRPA protocol for the phenotyping of ENU mutagenesis-derived C3H/HeJ, BALB/cCRLAnn, and B57BL/6 J mice (Barbaric et al. 2008; Smits et al. 2010; Srivastava et al. 2003).
Within the large-scale Munich ENU mutagenesis screen more than 850 mutant mouse lines have been isolated, derived from a large-scale genome-wide screen (Hrabě de Angelis et al. 2000) or from an implemented modifier screen on Dll1 lacZ knockout mice (Rubio-Aliaga et al. 2007). Our Dysmorphology Screen is focusing on the isolation of new mouse models for hereditary metabolic bone diseases (Fuchs et al. 2006; Lisse et al. 2008).
In previous studies in mice the reliability of biochemical markers for skeletal disorders, including alkaline phosphatase (ALP), has been shown (Srivastava et al. 2001). Combined ALP, total calcium (Ca), and inorganic phosphate (Pi) measurements in serum or plasma are routinely performed in patients with metabolic bone diseases (Table 1).
Ca and Pi homeostasis is balanced by intestinal absorption, mobilization, or binding in bone and renal excretion. Ca levels directly and indirectly influence intestinal phosphate absorption. Much less is known about the influences on Pi homeostasis (Bergwitz and Jüppner 2010). A key role in maintaining phosphate homeostasis is the reabsorption of phosphate from urine into the renal proximal tubules. A previously identified phosphaturic factor, FGF23 (fibroblast growth factor 23), acts as an endocrine hormone on the regulation of Pi reabsorption in the kidney and on renal vitamin D metabolism (ADHR Consortium 2000; Strom and Jüppner 2008).
Here we describe the results of the Munich ENU Mutagenesis Project to obtain new mutant mouse models for impaired bone metabolism by phenotyping for alterations of at least one of the described plasma parameters as selection markers. We isolated 71 new murine models that may be of special value for the development of new therapeutic approaches since a high number of metabolic bone diseases in human patients are caused by point mutations (Marini et al. 2010; Simon-Bouy et al. 2008; Wenkert et al. 2011).
Material and methods
Mice
For this study we used C3HeB/FeJ (C3H) inbred mice purchased originally from the Jackson Laboratory (Bar Harbor, ME, USA) and bred in our animal facility. The mice were housed and handled according to the federal animal welfare guidelines and the state ethics committee approved all animal studies. The mice were kept in a 12/12-h dark–light cycle and provided standard chow ad libitum (TPT total pathogen-free chow #1314: calcium content 0.9 %, phosphate 0.7 %, vitamin D3 600 IE; Altromin, Lage, Germany) and water. Hygienic monitoring was performed following FELASA recommendations (Nicklas et al. 2002). Mutant mouse lines derived from our screen were given internal lab codes and were assigned with official gene symbols and names after the mutation was identified.
ENU mutagenesis
ENU mutagenesis treatment of inbred strain C3H males was as described previously (Aigner et al. 2011). Litters produced from the ENU-treated C3H males (G0) are designated F1 in the following, while offspring produced from confirmed mutant F1 animals are designated G2.
Generation of F1 mice and confirmation of phenotypes in a dominant breeding strategy
The F1 animals investigated for this study were derived from a total of 893 G0 males from 15 different ENU-treated groups. Blood samples of 9,540 F1 animals (4,606 females and 4,934 males) were screened for alterations of total ALP, Ca, and Pi blood plasma levels. F1 mice showing alterations of blood-based parameters were retested after 14 days. Breeding for confirmation of a dominant phenotype was performed as described previously (Aigner et al. 2007).
Blood measurements
Blood samples (250 μl) were obtained from 12-week-old nonfasted anesthetized mice by puncture of the retro-orbital sinus, as already described (Rathkolb et al. 2000). All samples were collected between 9:00 and 11:00 a.m. Plasma analysis of ALP, Ca, and Pi was done using an Olympus AU400 autoanalyzer (Olympus, Hamburg, Germany) and adapted test kits (Klempt et al. 2006). Descriptive data are expressed as mean ± standard deviation. PTH values were analyzed with a Mouse Intact PTH ELISA Kit (TECOmedical, Bünde, Germany).
DXA and X-ray measurement
DXA (pDEXA Sabre, Norland Medical Systems Inc., Basingstoke, Hampshire UK, distributed by Stratec Medizintechnik GmbH, Pforzheim, Germany) and X-ray (Faxitron, Hewlett Packard, Palo Alto, CA, USA) measurements were performed for in-depth analysis in selected mouse lines as described previously (Abe et al. 2006; Fuchs et al. 2011).
Genetic mapping
To map the mutations, ENU-derived mutant mice were outcrossed to wild-type C57BL/6 J (B6) mice, as described previously (Aigner et al. 2009). For linkage analysis, SNP (single-nucleotide polymorphism) genotyping by high-throughput MALDI-TOF (matrix-assisted laser desorption/ionization time-of-flight) technology supplied by Sequenom (San Diego, CA, USA) was performed with a panel containing 158 markers evenly distributed over the whole genome (Klaften and Hrabě de Angelis 2005). We developed the internal MyGenotype database for statistical SNP data analysis.
Mutation analysis
Casr, Phex, Alpl, and Asgr1 exons were amplified with intronic primers and directly sequenced using BigDye v3.1 cycle sequencing (Applied Biosystems, Life Technologies, Foster City, CA, USA). Casr consists of 7 exons (NM013803), Phex (NM011077) consists of 22 exons, and Alpl (NM007431) consists of 12 exons. All primer sequences are available upon request. The mutation of the BAP005 mutant line was detected by chromosome sorting (CHROMBIOS, Raubling, Germany) and whole-chromosome sequencing on a Genome Analyzer IIx (Illumina, San Diego, CA, USA). DNA extraction from sorted chromosomes 11 was performed overnight at 42 °C with 0.25 M EDTA, 10 % Na lauroyl sarcosine, and 50 μg proteinase K. Extracted DNA was precipitated and resuspended in TE buffer. Paired-end libraries were constructed with the Illumina paired-end DNA sample preparation kit according to the manufacturer’s protocols and as described previously (Eck et al. 2009). Alignment of the reads was performed with the BWA software, and subsequent analysis was performed with the SAMtools package. In total, ~82 million reads and ~157 million reads were generated for the mutant and control strain, respectively, of which 64 % mapped to the target chromosome 11 for the mutant strain, while 26 % of the control strain reads were on target. The identified nonsynonymous sequence variation in Asgr1 was confirmed in mutant mice by capillary sequencing.
Statistical analysis
Statistical analysis of parameters of F1 animals and sex- and age-matched wild-type C3H mice were performed using the software package JMP Release 5.1 (SAS Institute, Cary, NC, USA). The reference values were obtained from untreated age-matched C3H wild-type control groups (50 males and 50 females). Single F1 variants for ALP activity and Ca levels were defined by a Z score ≥3 or ≤–3 compared to the age-matched control groups. Mice showing hypophosphatemia were tested three times to confirm Pi changes. A Z score of ≤–2 was taken to select variants for hypophosphatemia. Statistical differences (P values) of the means of ALP, Ca, or Pi blood values between all tested affected mice and nonaffected littermates of a mutant line were assessed by one-way analysis of variance (ANOVA), t test (giving mean ± SD values), and the Mann-Whitney rank sum test (giving median values) using SigmaStat 3.5 (Systat Software Inc., Chicago, IL, USA).
Results
Overall results and statistics
In order to identify early stages of disturbed bone turnover, we investigated the diagnostic value of routine assays for ALP activity and Ca and Pi levels in the plasma of mice derived from ENU-treated males for its comparability to their use in human patients (Table 1). This table also shows other mouse lines obtained for selected metabolic bone diseases and the observed alterations of plasma parameters in these models. Since we were interested only in mouse lines showing alterations of the bone ALP (bALP) isoform of the measured total ALP enzyme, variants with additional alterations of ALAT (alanine-amino-transferase) and ASAT (aspartate-amino-transferase) levels were excluded from this study.
Two hundred fifty-seven phenodeviants (2.7 %, 87 females and 170 males) of 9,540 F1 animals showed alterations in at least one of the three parameters of interest (ALP, Ca, and Pi) in two repeated blood measurements. One hundred ninety of the 257 (74 %) phenodeviants were mated to wild-type C3H mice in confirmation crosses. In 71 of the mated 190 (37 %) (25 females and 46 males), the observed phenotype was genetically transmitted as a dominant trait (Table 2); however, six of these mutant lines were lost because no mutant male offspring was produced for sperm cryopreservation. For 110 of the mated 190 (58 %) phenodeviants, inheritance could not be confirmed because of sterility (n = 22/110, 20 %), the mice died due to unknown reasons (n = 15/110, 14 %), or the hypothesis of a dominant mutation was excluded (n = 73/110, 66 %). Confirmation crosses for the remaining 9 of the 190 phenodeviants are still underway. Sixty-seven of the 257 (26 %) phenodeviants were not mated due to space limitations; however, their sperm was frozen. Founder F1 mice with a similar phenotype and derived from the identical G0 male were expected to carry the identical mutation. Fifteen mutations have been identified resulting in new alleles of the Phex, Casr, and Alpl genes (Table 3).
New mouse lines carrying mutations of the Phex (phosphate-regulating gene with homologies to endopeptidases on the X-chromosome) gene
Affected animals of the BAP012 (Bone screen Alkaline Phosphatase No. 012) mutant line displayed a significant (P ≤ 0.001) decrease in plasma Pi levels. Female mutant mice (n = 42) exhibited a Pi value of 1.3 ± 0.2 mmol/l compared to female wild-type mice (2.0 ± 0.3 mmol/l, n = 11). Male mutant mice (n = 7) had a Pi value of 1.2 ± 0.1 mmol/l compared to 2.0 ± 0.3 mmol/l in male wild-type mice (n = 44). Mean ALP activity was significantly elevated (P ≤ 0.001) in female mutants (266.4 ± 35.3 U/l) compared to wild-type littermates (147.9 ± 17.9 U/l), and also in mutant male mice (370.9 ± 88.5 U/l) compared to their wild-type littermates (120 ± 8.5 U/l). In addition to these biochemical alterations, all mutants showed reduced body size, shortened hind limbs, and mild head-tossing behavior as described in other Phex mouse models (Lorenz-Depiereux et al. 2004; Moriyama et al. 2011). Genetic crosses revealed X-linked inheritance of the phenotype. Thus, mutant mice of both sexes were derived from mated mutant females, but from matings of male mutants only female mutants were born. Based on the phenotypic data, the causative mutation was hypothesized to be in the Phex gene. DNA sequence analysis of the Phex gene revealed a new hemizygous nonsense mutation in exon 2 (c.148A > T, p.Lys50X) (Fig. 1a). The mutation is located within the large extracellular domain of the protein close to the transmembrane domain. The Phex gene in mice is syntenic to the human PHEX gene, which is organized into 22 exons and encodes a type II transmembrane protein with homology to zinc metallopeptidases (HYP Consortium 1995). Inactivating mutations of the PHEX gene cause X-linked dominant hypophosphatemic rickets (XLHR), which has an incidence of 1:20,000 and is the most common familial form of hypophosphatemic rickets in humans (Burnett et al. 1964; Tenenhouse 1999).
a DNA sequence analysis of the Phex gene exon 2 revealed a hemizygous nonsense mutation (c.148A > T, p.Lys50X) in the DNA of a male C3Heb/FeJ-PhexBAP012 mutant mouse leading to a premature translation stop codon after 49 amino acids. b DNA sequence analysis of the Phex gene exon 22 revealed a hemizygous missense mutation (c.2197T > C, p.Cys733Arg) in the DNA of a male C3Heb/FeJ-PhexBAP024 mutant mouse. Variants are marked by an asterisk
Mice of the BAP024 mutant line express similar phenotypes, with gender influences on inheritance as the C3Heb/FeJ-PhexBAP012 mice. In BAP024 we found a new missense mutation in exon 22 of the Phex gene (c.2197T > C, p.Cys733Arg) (Fig. 1b), also located in the large extracellular catalytic domain of the protein. The cysteine at position 733 is highly conserved among other vertebrate species (Du et al. 1996). A cysteine-to-serine substitution at the corresponding position of the C3Heb/FeJ-PhexBAP024 mutation has been described recently in a patient with XLHR (Filisetti et al. 1999). No spontaneous Phex point mutations on the C3H strain have been isolated previously.
New mouse lines carrying mutations of the Casr (calcium-sensing receptor) gene
The BCH002 (Bone screen Calcium High No. 002) line showed a statistically significant increase of Ca levels in mutant animals compared to wild-type littermates (P ≤ 0.001). Female mutants’ Ca level was 2.9 ± 0.1 mmol/l (n = 23) compared to 2.43 ± 0.1 mmol/l for wild-type littermates (n = 19). The male mutant value was 2.87 ± 0.1 mmol/l (n = 20) compared to the wild-type littermates’ value of 2.41 ± 0.1 mmol/l (n = 20). Fifty-three percent of female and male mutant BCH002 mice had slightly reduced Pi levels. Histological analysis showed enlarged parathyroid glands in heterozygous mutant mice (Fig. 2a). A group of 11 female (6 mutants, 5 wild types) and 20 male mice (10 mutants, 10 wild types) was tested for PTH values, resulting in significantly raised median PTH values for mutant mice (P ≤ 0.001): female mutants, 214.9 pg/ml (25 % 203.3 pg/ml and 75 % 265.7 pg/ml), and wild types, 85.7 pg/ml (25 % 79.6 pg/ml and 75 % 113.1 pg/ml). Male mutants showed 235 pg/ml (25 % 191 pg/ml and 75 % 409.9 pg/ml) compared to wild types showing 102.7 pg/ml (25 % 78.8 pg/ml and 75 % 117.2 pg/ml). So far eight pups were derived from a first heterozygous intercross but no homozygous mutant was found. Mapping analysis of 40 mutant and 20 wild-type BCH002 animals derived from the dominant backcrosses to the B6 strain revealed linkage to chromosome 16 (Table 4), with the highest χ2 value at the marker rs4186801 (51.47 Mb, mouse genome Build 37.1, UCSC). In this region Casr was the most promising candidate gene for the observed phenotype. DNA sequence analysis of the Casr gene revealed a new heterozygous missense mutation (c.2579T > A, p. Ile859Asn) within the protein-coding region of exon 7 (Fig. 2b) of the gene that was not present in wild-type C3H and B6 mice. CASR belongs to the family of G-protein-coupled receptors (GPCRs) and is an integral membrane protein that senses changes in the extracellular calcium concentration to parathyroid cells.
a Representative pictures of the histological changes found in the mutant mouse line BCH002: 1, 2 (left) depict a H&E-stained section of normal thyroid gland (T) and parathyroid gland (P) in a control mouse. In 1 (low-magnification panel, 5×, scale bar = 100 μm), the normal gland appears as a small compact mass of dark cells. In 2 at higher magnification (20×, scale bar = 20 μm), two cell types interspersed with capillaries and sinusoids are identified: the chief cells, with a small basophilic cytoplasm, and the light cells, with abundant light cytoplasm. 3, 4 (right) show a H&E-stained section of the normal thyroid gland (T) and the enlarged parathyroid gland (P) with loose structure observed in heterozygous C3HeB/FeJ-CasrBCH002 mutant mice (3). At higher magnification in 4, an increase in the number of light cells is observed. b DNA sequence analysis of the Casr gene of C3HeB/FeJ-CasrBCH002 mice revealed a heterozygous mutation in exon 7 (c.2579T > A, p.Ile859Asn) that is marked by an asterisk
In addition, six new alleles of the Casr gene were isolated in other mouse lines (BCH003, BCH004, BCH007, BCH011, BCH013, and BCH014) (Table 3) creating an allelic series for functional analysis of the gene. Median PTH levels were significantly increased (P = 0.010) in first testings of BCH013 female mutants (n = 6), showing 175.2 pg/ml (25 % 143.21 pg/ml and 75 % 198.33 pg/ml) compared to wild types (n = 4) showing 50.061 pg/ml (25 % 48.805 pg/ml and 75 % 56.962 pg/ml). Male mutants (n = 10) displayed 100.984 ± 30.765 pg/ml and wild types (n = 9) 55.485 ± 14.734 pg/ml. For all other mouse lines with mutations of the Casr gene, PTH data are underway. The missense and nonsense mutations of these mouse lines were located in exons 3, 4, 5, and 7 of the Casr gene (Table 3).
New mouse lines carrying mutations of the Alpl (alkaline phosphatase, liver/bone/kidney) gene
In mutant mice of the BAP032 line, statistically significant (P < 0.001) low mean ALP activity was found in female mutants (47 ± 5.8 U/l, n = 9) compared to wild-type littermates (157.8 ± 7.9 U/l, n = 8), and in male mutants (38.4 ± 6.3 U/l, n = 12) compared to wild-type littermates (129.5 ± 10.1 U/l, n = 10) (Fig. 3a). Significantly reduced ALP activity suggested a mutation in the Alpl gene encoding the tissue nonspecific ALP (TNSALP). We sequenced this gene in BAP032 mice and revealed a new heterozygous missense mutation in exon 11 located within the protein-coding region of the Alpl gene on chromosome 4 (c.1217A > G, p.Asp406Gly) (Fig. 3b). This mutation was not found in wild-type C3H littermates or in wild-type B6 mice. We isolated five additional mouse lines carrying new alleles of the Alpl gene (Table 3). Four sequence variations were located in exons 7, 10, or 12 (BAP020, BAP023, BAP027, SAP007) and one affects the splice site in intron 9 (BAP026).
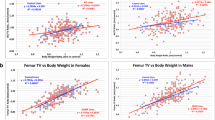
a C3HeB/FeJ-AlplBAP032 ALP blood activities (mean ± SD U/l) in female mutant (N = 8), female wild-type (N = 9), male mutant (N = 12), and male wild-type (N = 10) mice. Mean ± SD ALP activities were: female mutants 47 ± 5.8 U/l (P < 0.001); female wild-types 157.8 ± 7.9 U/l; male mutants 38.4 ± 6.3 U/l (P < 0.001); male wild-types 129.5 ± 10.1 U/l (t-test). b DNA sequence analysis of the Alpl gene exon 11 revealed a new heterozygous missense mutation (c.1217A > G, p.Asp406Gly). Variant is marked by an asterisk
Other mouse lines and mutations
Female and male mutant mice of the BAP005 line showed statistically significant (P ≤ 0.001) increased mean ALP activity. The value in female mutants (n = 25) was 233 ± 21 U/l compared to 136 ± 14 U/l in wild-type littermates (n = 32), and in male mutants (n = 39) ALP activity was 188 ± 19.81 U/l compared to 104.5 ± 10.43 U/l in their wild-type littermates (n = 36). The mouse line breeds homozygous offspring with very high ALP activities. Homozygous females derived from heterozygous intercrosses showed mean ALP activity of 587 ± 39 U/l (n = 12), and ALP activity in homozygous males was 482 ± 51 U/l (n = 21). SNP mapping revealed a region between the markers rs26982471 and rs27000576 (53.99–114.33 Mb, mouse genome Build 37.1, UCSC) on chromosome 11. Sorting of chromosome 11 and whole chromosome 11 sequencing on a GAIIx next-generation sequencing machine revealed a new missense mutation in the Asgr1 (asialoglykoprotein receptor 1) gene within the translated region (c.815A > G, p.Tyr272Cys). The mutation was sequenced in 16 BAP005 mutant mice, but neither in 4 wild-type littermates, nor in additional 4 wild-type mice from different inbred strains (BALB/c, DBA/2, FVB, SJL).
For eight additional mouse lines (BAP002, BAP003, BAP004, BAP014, BPL004, BPL006, BPL008, and TRE002) showing high ALP activity, low Pi, and high or low Ca values as a phenotype, genetic mapping has been finished (Table 3) and sequencing of candidate genes is in progress. For selected mouse lines we will include exome sequencing to find the causative mutation.
Discussion
In this study we described a large-scale ENU mutagenesis screen (Soewarto et al. 2009), with the main focus on malfunctioning bone turnover. In other projects murine models for disturbed bone metabolism were obtained by gene targeting (Daroszewska et al. 2011; Ducy et al. 1996; Forlino et al. 1999; Kato et al. 2002), transgene insertions (Imanishi et al. 2001; Rauch et al. 2010) or spontaneous mutations (Eicher et al. 1976; Marks and Lane 1976). Here, we isolated 71 new mouse models by screening for alterations of total ALP activity and total Ca and Pi values in plasma of 9,540 F1 mice. Our results demonstrate that malfunctions of bone metabolism in mice may be efficiently detected by the analysis of human standard clinical chemical parameters.
In this study the highest fraction of new mouse lines revealed alterations of total ALP activity (Table 3). Since these mouse lines discriminated in phenotype expression and occurrence of additional phenotypes, the phenotypes presumably depend on different molecular mechanisms. Total ALP was chosen as a parameter of interest since elevated ALP activity is the most frequently measured parameter for human Paget’s disease (Langston and Ralston 2004), X-linked hypophosphatemic rickets (XLHR) (Jonsson et al. 2003; Mäkitie et al. 2003), autosomal dominant hypophosphatemic rickets (ADHR) (Econs and McEnery 1997; Imel et al. 2007; Kruse et al. 2001), and type I osteoporosis (Avbersek-Luznik et al. 2007; Pedrazzoni et al. 1996).
Screening for alterations of total Ca and Pi values without changes of ALP activity resulted in 34 mutant lines with confirmation of the observed phenotype (Table 2). While the Ca parameter was easy to measure, Pi values were artificially elevated after plasma storage for longer than 1 day, freezing of the samples, or hemolysis. Metabolic bone diseases may be reflected in changes of more than one parameter, and very often two or three of the parameters of interest showed alterations in the same individual mouse line, as is commonly observed in human patients (Table 1).
In our screen we obtained new mouse models for hypophosphatemia, hyperparathyroidism, and hypophosphatasia. Despite the large number of existing mouse models for XLHR, there are still open questions on the mechanism of PHEX in renal phosphate wasting, abnormal vitamin D metabolism, and matrix mineralization (Addison et al. 2010; Brownstein et al. 2010). The C3HeB/FeJ-PhexBAP012 and C3HeB/FeJ-PhexBAP024 mutant lines represent two new mutant mouse lines with novel point mutations modeling XLHR in addition to previously published models (Carpinelli et al. 2002; Lorenz-Depiereux et al. 2004; Xiong et al. 2008).
New point mutations of the Casr gene were found in seven mouse lines. The large extracellular domain of the receptor contains clusters of amino acid residues, which may be involved in calcium binding (Brown et al. 1993). Exon 7 encodes the seven transmembrane domains and four intracellular loops of CASR (Chang et al. 2008). Human CASR mutations are known to be causative for primary hyperparathyroidism (HP) (Bilezikian et al. 2005) and familial benign hypocalciuric hypercalcemia (FHH) (Pollak et al. 1994). Approximately two thirds of FHH patients showed loss-of-function mutations involving the 3,234-bp coding region of the CASR gene (D’Souza-Li et al. 2002). Individuals with HP and FHH discriminate in creatinine clearance and serum magnesium values, both being higher in FHH (Marx et al. 1981). It has been demonstrated that individuals with FHH are heterozygous, and children within these families with severe neonatal primary hyperparathyroidism (NSHPT) are homozygous for CASR mutations (Janicic et al. 1995; Pollak et al. 1993). Mice with tissue-specific deletion of Casr in the parathyroid gland and bone exhibited profound bone defects (Chang et al. 2008). C3H;102CasrNuf/H mice carry an activating ENU-derived Casr point mutation that exhibits hypocalcemia, hyperphosphatemia, cataracts, and ectopic calcifications (Hough et al. 2004). We obtained the first presumed loss-of-function point mutation isolated in C3HeB/FeJ-CasrBCH002 mice that is supposed to model human FHH. Since the mouse line has been bred more than 15 generations and because we found six other independent Casr mutations for this phenotype, it is more than likely that the consistent phenotype is due to the isolated point mutation of the Casr gene. Heterozygous C3HeB/FeJ-CasrBCH002 mice exhibited high Ca and PTH values similar to targeted Black Swiss/129SvJ Casr +/− and Casr −/− mice (Ho et al. 1995), but, in addition, they showed enlarged parathyroid glands described only for Casr −/− mice. Further heterozygous intercrosses are required to find out if homozygous C3HeB/FeJ-CasrBCH002 mice are viable, which is not the case in Casr −/− mice. This would raise the opportunity to obtain a mouse model for NSHPT. More than 270 mutations have been described so far in the human CASR mutation database (www.casrdb.mcgill.ca; Nakajima et al. 2009), and interestingly most of the human mutations were found in exons 4 and 7. The mouse lines carrying Casr mutations obtained in our screen showed slight differences in the expression of the phenotype. Additional studies on phenotypical and histological traits will help to discriminate between the different effects of each point mutation on the severity of hyperparathyroidism and concomitantly to improve our understanding of CASR mutations in human patients.
Heterozygous C3HeB/FeJ-AlplBAP032 mice showed a statistically significant reduction of ALP activity in plasma without additional phenotypes, as observed in heterozygous Akp2 Hpp/+mice derived in an ENU mutagenesis screen on C3H/HeH background (Hough et al. 2007). In Akp2 Hpp/+ mice, an Alpl loss-of-function mutation led to the rare disease hypophosphatasia (HPP) which displays reduction of plasma ALP activities to about 50 % in Akp2 Hpp/+ and a stronger reduction in Akp2 Hpp/Hpp mice. Akp2 Hpp/+ mice were radiographically and histologically indistinguishable from wild-type mice at different time points, as were 16-week-old C3HeB/FeJ-AlplBAP032 mice in DEXA and X-ray analysis. Interestingly, we observed a stronger ALP reduction in heterozygous C3HeB/FeJ-AlplBAP032 mice than in Akp2 Hpp/+mice, with ALP activities in female and male mutant mice reduced to 29 % of that found in wild-type littermates. Severe HPP forms are characterized by hypomineralization, rickets, seizures, and nephrocalcinosis due to hypercalciuria (Beck et al. 2009). Alpl −/− mice showed a reduction in body size, no detectable ALP levels, and lethality prior to weaning, whereas Alpl +/− mice appeared healthy (Narisawa et al. 1997). The identical point mutation of C3HeB/FeJ-AlplBAP032 mice has also been described for a patient with HPP (Taillandier et al. 2000). Heterozygous C3HeB/FeJ-AlplBAP032 mice presumably model mild adult HPP. The mouse line was bred for more than ten generations, showing full penetrance of the phenotype in all litters. A multitude of diverse point mutations, deletions, and insertions of the human TNSALP gene causing HPP are listed in the hypophosphatasia database (www.sesep.uvsq.fr/03_hypo_mutations.php). The diversity of published human point mutations emphasizes the importance of mouse models for further investigations on physiological functions and cellular mechanisms of Alpl regions involved in collagen and Ca binding. Interestingly, we isolated in addition one silent mutation in the BAP020 mouse line (Table 4) showing the expected phenotype. No additional Alpl mutations were found in this mouse line. Alpl mRNA and translation of ALP were not analyzed so far.
Since only total ALP can be tested in mice so far, we probably will isolate mouse lines showing alterations other than the bone ALP isoform. High alterations of plasma ALP activities without any additional phenotypes, as observed in homozygous animals of the C3HeB/FeJ-Asgr1BAP005 line, have not been published in mice before. It has been described in patients with chronic liver disease that the adult intestinal ALP isoenzyme was increased due to the reduced efficiency or numbers of asialoglycoprotein receptors (Moss 1994). Thus, the mutation of the gene in BAP005 mice seems to cause alterations of the intestinal ALP isoform as a secondary effect. ASRG1 mutations may be responsible for high ALP activities of so far unknown reasons in humans without any skeletal disorders (Panteghini 1991) or may cause benign familial hyperphosphatasemia (Siraganian et al. 1989).
We have to consider bone as an active metabolic organ with a possible influence on metabolism in diseases of disturbed bone turnover (Ferron et al. 2010; Fulzele et al. 2010). For this reason, systematic analysis of all organ systems, as in the German Mouse Clinic (Gailus-Durner et al. 2005), might provide new insights into the actions in these pathways. Our mouse models will be archived by the European Mouse Mutant Archive (EMMA) and are available (www.emmanet.org) for the scientific community.
References
Abe K, Fuchs H, Lisse T, Hans W, de Angelis Hrabě (2006) New ENU-induced semidominant mutation, Ali18, causes inflammatory arthritis, dermatitis, and osteoporosis in the mouse. Mamm Genome 17:915–926
Abe K, Wechs S, Kalaydjiev S, Franz T, Busch DH (2007) Novel lymphocyte-independent mechanisms to initiate inflammatory arthritis via bone marrow derived cells of Ali18 mutant mice. Rheumatology 47(3):292–300
Addison WN, Masica DL, Gray JJ, McKee MD (2010) Phosphorylation-dependent inhibition of mineralization by osteopontin ASARM peptides is regulated by PHEX cleavage. J Bone Miner Res 25(4):695–705
ADHR Consortium (2000) Autosomal dominant hypophosphatemic rickets is associated with mutations in FGF23. Nat Genet 26(3):345–348
Aigner B, Rathkolb B, Mohr M, Klempt M, Hrabě de Angelis M et al (2007) Generation of ENU-induced mouse mutants with hypocholesterolemia: novel tools for dissecting plasma lipoprotein homeostasis. Lipids 42(8):731–737
Aigner B, Rathkolb B, Klaften M, Sedlmeier R, Klempt M et al (2009) Generation of N-ethyl-N-nitrosourea-induced mouse mutants with deviations in plasma enzyme activities as novel organ-specific disease models. Exp Physiol 94(4):412–421
Aigner B, Rathkolb B, Klempt M, Wagner S, Michel D et al (2011) Generation of N-ethyl-N-nitrosourea-induced mouse mutants with deviations in hematological parameters. Mamm Genome 22:495–505
Ashwell G, Morell AG (1974) The role of surface carbohydrates in the hepatic recognition and transport of circulating glycoproteins. Adv Enzymol Relat Areas Mol Biol 41:99–128
Avbersek-Luznik I, Gmeiner-Stopar T, Marc J (2007) Activity or mass concentration of bone-specific alkaline phosphatase as a marker of bone formation. Clin Chem Lab Med 45(8):1014–1018
Badadani M, Nalbandian A, Watts GD, Vesa J, Kitazawa M (2010) VCP associated inclusion body myopathy and Paget disease of bone knock-in mouse model exhibits tissue pathology typical of human disease. PLoS One 5(10):e13183
Barbaric I, Perry MJ, Dear TN, Rodrigues Da Costa A, Salopek D (2008) An ENU-induced mutation in the Ankrd11 gene results in an osteopenia-like phenotype in the mouse mutant Yoda. Physiol Genomics 32(3):311–321
Beck L, Karaplis AC, Amizuka N, Hewson AS, Ozawa H (1998) Targeted inactivation of Npt2 in mice leads to severe renal phosphate wasting, hypercalciuria, and skeletal abnormalities. Proc Natl Acad Sci USA 95(9):5372–5377
Beck C, Morbach H, Richl P, Stenzel M, Girschick HJ (2009) How can calcium pyrophosphate crystals induce inflammation in hypophosphatasia or chronic inflammatory joint diseases? Rheumatol Int 29(3):229–238
Bergwitz C, Jüppner H (2010) Regulation of phosphate homeostasis by PTH, vitamin D, and FGF23. Annu Rev Med 61:91–104
Bilezikian JP, Brandi ML, Rubin M, Silverberg SJ (2005) Primary hyperparathyroidism: new concepts in clinical, densitometric and biochemical features. J Int Med 257(1):6–17
Bonadio J, Saunders TL, Tsai E, Goldstein SA, Morris-Winmann J et al (1990) Transgenic mouse model of the mild dominant form of osteogenesis imperfecta. Proc Natl Acad Sci USA 87:7145–7149
Braga V, Gatti D, Rossini M, Colapietro F, Battaglia E (2004) Bone turnover markers in patients with osteogenesis imperfecta. Bone 34(6):1013–1016
Brown EM, Gamba G, Riccardi D, Lombardi M, Butters R et al (1993) Cloning and characterization of an extracellular Ca(2+)-sensing receptor from bovine parathyroid. Nature 366:575–580
Brownstein CA, Zhang J, Stillman A, Elis B, Troiano N et al (2010) Increased bone volume and correction of Hyp mouse hypophosphatemia in the Klotho/Hyp mouse. Endocrinology 151(2):492–501
Burnett CH, Dent CE, Harper C, Warland BJ (1964) Vitamin D-resistant rickets. Am J Med 36:222–232
Carpinelli MR, Wicks IP, Sims NA, O’Donnell K, Hanzinikolas K et al (2002) An ethyl-nitrosourea-induced point mutation in Phex causes exon skipping, X-linked hypophosphatemia, and rickets. Am J Pathol 161(5):1925–1933
Chang W, Tu C, Chen TH, Bikle D, Shoback D (2008) The extracellular calcium-sensing receptor (CaDR) is a critical modulator of skeletal development. Sci Signal 1(35):ra1
Chavassieux P, Seeman E, Delmas PD (2007) Insights into material and structural basis of bone fragility from diseases associated with fractures: how determinants of the biomechanical properties of bone are compromised by disease. Endocr Rev 28:151–164
Chipman SD, Sweet HO, McBride DJ Jr, Davisson MT, Marks SC Jr (1993) Defective pro alpha 2(I) collagen synthesis in a recessive mutation in mice: a model of human osteogenesis imperfecta. Proc Natl Acad Sci USA 90(5):1701–1705
Chodirker BN, Evans JA, Seargeant LE, Cheang MS, Greenberg CR (1990) Hyperphosphatemia in infantile hypophosphatasia: implications for carrier diagnosis and screening. Am J Hum Genet 46:280–285
Cundy T, Horne A, Bolland M, Gamble G, Davidson J (2007) Bone formation markers in adults with mild osteogenesis imperfecta. Clin Chem 53(6):1109–1114
D’Souza-Li, Yang B, Canaff L, Bai M, Hanley DA et al (2002) Identification and functional characterization of novel calcium-sensing receptor mutations in familial hypocalciuric hypercalcemia and autosomal dominant hypocalcemia. J Clin Endocrinol Metab 87:1309–1318
Daroszewska A, van’ t Hof RJ, Rojas JA, Layfield R, Landao-Basonga E et al (2011) A point mutation in the ubiquitin associated domain of SQSMT1 is sufficient to cause a Paget’s disease like disorder in mice. Hum Mol Genet 20(14):2734–2744
Delmas PD (1992) Clinical use of biochemical markers of bone remodeling in osteoporosis. Bone 13(Suppl 1):S17–S21
Du L, Desbarats M, Viel J, Glorieux FH, Cawthorn C et al (1996) cDNA cloning of the murine Phex gene implicated in X-linked hypophosphatemia and evidence for expression in bone. Genomics 36:22–28
Ducy P, Desbois C, Boyce B, Pinero G, Story B et al (1996) Increased bone formation in osteocalcin-deficient mice. Nature 382(6590):448–452
Eck SH, Benet-Pagès A, Flisikowski K, Meitinger T, Fries R et al (2009) Whole genome sequencing of a single Bos taurus animal for single nucleotide polymorphism discovery. Genome Biol 10(8):R82
Econs MJ, McEnery PT (1997) Autosomal dominant hypophosphatemic rickets/osteomalacia: clinical characterization of a novel renal phosphate-wasting disorder. J Clin Endocrinol Metab 82(2):674–681
Eicher EM, Southard JL (1972) Hypophosphatemia (Hyp); Chr 7 linkage. Mouse News Lett 47:36
Eicher EM, Southard JL, Scriver CR, Glorieux FH (1976) Hypophosphatemia: mouse model for human familial hypophosphatemic (vitamin D-resistant) rickets. Proc Natl Acad Sci USA 73:4667–4671
Farrow EG, Yu X, Summers LJ, Davis SI, Fleet JC et al (2011) Iron deficiency drives an autosomal dominant hypophosphatemic rickets (ADHR) phenotype in fibroblast growth factor-23 (Fgf23) knock-in mice. Proc Natl Acad Sci USA 108(46):E1146–E1155
Feng JQ, Huang H, Lu Y, Ye L, Xie Y et al (2003) The Dentin matrix protein 1 (Dmp1) is specifically expressed in mineralized, but not soft, tissues during development. J Dent Res 82(10):776–780
Feng JQ, Scott G, Guo D, Jiang B, Harris M et al (2008) Generation of a conditional null allele for Dmp1 in mouse. Genesis 46(2):87–91
Ferron M, Wei J, Yoshizawa T, Del Fattore A, DePinho RA et al (2010) Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Cell 142(2):296–308
Filisetti D, Ostermann G, von Bredow M, Strom T, Filler G et al (1999) Non-random distribution of mutations in the PHEX gene, and under-detected missense mutations at non-conserved residues. Eur J Hum Genet 7(5):615–619
Forlino A, Porter FD, Lee EJ, Westphal H, Marini JC (1999) Use of the Cre/lox recombination system to develop a non-lethal knock-in murine model for osteogenesis imperfecta with an α1(I)G349C substitution. J Biol Chem 274(53):37923–37931
Freeman DA (1988) Paget’s disease of bone. Am J Med Sci 295(2):144–158
Fuchs H, Lisse T, Abe K, Hrabě de Angelis M (2006) Screening for bone and cartilage phenotypes in mice. In: Hrabě de Angelis M, Chambon P, Brown S (eds) Phenotyping of the laboratory mouse. Wiley-VCH, Weinheim, pp 35–86
Fuchs H, Gailus-Durner V, Adler T, Aguilar-Pimentel A, Becker L et al (2011) Mouse phenotyping. Methods 53(2):120–135
Fulzele K, Riddle RC, DiGirolamo D, Cao X, Wan C et al (2010) Insulin receptor signaling in osteoblasts regulates postnatal bone acquisition and body composition. Cell 142(2):309–319
Gailus-Durner V, Fuchs H, Becker L, Bolle I, Brielmeier M et al (2005) Introducing the German mouse clinic: open access platform for standardized phenotyping. Nat Methods 2(6):403–404
Goseki-Sone M, Sogabe N, Fukushi-Irie M, Mizoi L, Orimo H et al (2005) Functional analysis of the single nucleotide polymorphism (787T > C) in the tissue-nonspecific alkaline phosphatase gene associated with BMD. J Bone Miner Res 20(5):773–782
Ho C, Conner DA, Pollak MR, Ladd DJ, Kifor O et al (1995) A mouse model of human familial hypocalciuric hypercalcemia and neonatal severe hyperparathyroidism. Nat Genet 11(4):389–394
Hough TA, Bogani D, Cheeseman MT, Favor J, Nesbit MA et al (2004) Activating calcium-sensing receptor mutation in the mouse is associated with cataracts and ectopic calcification. Proc Natl Acad Sci USA 101(37):13566–13571
Hough TA, Polewski M, Johnson K, Cheeseman M, Nolan PM et al (2007) Novel mouse model of autosomal semidominant adult hypophosphatasia has a splice site mutation in the tissue nonspecific alkaline phosphatase gene akp2. J Bone Miner Res 22(9):1397–1407
Hrabě de Angelis M, Balling R (1998) Lange scale ENU screens in the mouse: genetics meets genomics. Mutat Res 400(1–2):25–32
Hrabě de Angelis M, Flaswinkel H, Fuchs H, Rathkolb B, Soewarto D et al (2000) Genome-wide, large-scale production of mutant mice by ENU mutagenesis. Nat Genet 25(4):444–447
HYP Consortium (1995) A gene (PHEX) with homologies to endopeptidases is mutated in patients with X-linked hypophosphatemic rickets. Nat Genet 11(2):130–136
Imanishi Y, Hosokawa Y, Yoshimoto K, Schipani E, Mallya S et al (2001) Primary hyperparathyroidism caused by parathyroid-targeted overexpression of cyclin D1 in transgenic mice. J Clin Invest 107(9):1093–1102
Imel EA, Hui SL, Econs MJ (2007) FGF23 concentrations vary with disease status in autosomal dominant hypophosphatemic rickets. J Bone Miner Res 22(4):520–526
Janicic N, Pausova Z, Cole DEC, Hendy GN (1995) Insertion of an Alu sequence in the Ca(2+)-sensing receptor gene in familial hypocalciuric hypercalcemia and neonatal severe hyperparathyroidism. Am J Hum Genet 56(4):880–886
Jonsson KB, Zahradnik R, Larsson T, White KE, Sugimoto T et al (2003) Fibroblast growth factor 23 in oncogenic osteomalacia and X-linked hypophosphatemia. N Engl J Med 348(17):1656–1663
Kato M, Patel MS, Levasseur R, Lobov I, Chang BH et al (2002) Cbfa1-independent decrease in osteoblast proliferation, osteopenia, and persistent embryonic eye vascularization in mice deficient in Lrp5, a Wnt coreceptor. J Cell Biol 157(2):303–314
Klaften M, Hrabě de Angelis M (2005) ARTS: a web-based tool for the set-up of high-throughput genome-wide mapping panels for the SNP genotyping of mouse mutants. Nucleic Acids Res 33(Web Server Issue):W496–W500
Klempt M, Rathkolb B, Fuchs H, Hrabé de Angelis M, Wolf E (2006) Genotype-specific environmental impact on the variance of blood values in inbred and F1 hybrid mice. Mamm Genome 17(2):93–102
Kruse K, Woelfel D, Strom TM (2001) Loss of renal phosphate wasting in a child with autosomal dominant hypophosphatemic rickets caused by a FGF23 mutation. Horm Res 55(6):305–308
Kurima K, Peters LM, Yang Y, Riazuddin S, Ahmed ZM et al (2002) Dominant and recessive deafness caused by mutations of a novel gene, TMC1, required for cochlear hair-cell function. Nat Genet 30:277–284
Langston AL, Ralston SH (2004) Management of Paget’s disease of bone. Rheumatology 43(8):955–959
Lisse TS, Thiele F, Fuchs H, Hans W, Przemeck GK et al (2008) ER stress-mediated apoptosis in a new mouse model for osteogenesis imperfecta. PLoS Genet 4(2):e7
Liu X (1995) A targeted mutation at the known collagenase cleavage site in mouse type I collagen impairs tissue remodeling. J Cell Biol 130(1):227–237
Lomeli H, Ramos-Mejia V, Gertsenstein M, Lobe CG, Nagy A (2000) Targeted insertion of Cre recombinase into the TNAP gene: excision in primordial germ cells. Genesis 26(2):116–117
Lorenz-Depiereux B, Guido VE, Johnson KR, Zheng QY, Gagnon LH et al (2004) New intragenic deletions in the Phex gene clarify X-linked hypophosphatemia-related abnormalities in mice. Mamm Genome 15(3):151–161
Lorenz-Depiereux B, Bastepe M, Benet-Pagès A, Amyere M, Wagenstaller J et al (2006a) DMP1 mutations in autosomal recessive hypophosphatemia implicate a bone matrix protein in the regulation of phosphate homeostasis. Nat Genet 38(11):1248–1250
Lorenz-Depiereux B, Benet-Pagès A, Eckstein G, Tenenbaum-Rakover Y, Wagenstaller J et al (2006b) Hereditary hypophosphatemic rickets with hypercalciuria is caused by mutations in the sodium-phosphate cotransporter gene SLC34A3. Am J Hum Genet 78(2):193–201
Lorenz-Depiereux B, Schnabel D, Tiosano D, Häusler G, Strom TM (2010) Loss-of-function ENPP1 mutations cause both generalized arterial calcification of infancy and autosomal-recessive hypophosphatemic rickets. Am J Hum Genet 86(2):267–272
MacGregor GR, Zambrowicz BP, Soriano P (1995) Tissue non-specific alkaline phosphatase is expressed in both embryonic and extraembryonic lineages during mouse embryogenesis but is not required for migration of primordial germ cells. Development 121(5):1487–1496
Mäkitie O, Doria A, Kooh SW, Cole WG, Daneman A et al (2003) Early treatment improves growth and biochemical and radiographic outcome in X-linked hypophosphatemic rickets. J Clin Endocrinol Metab 88(8):3591–3597
Marini JC, Cabral WA, Barnes AM (2010) Null mutations in LEPRE1 and CRTAP cause severe recessive osteogenesis imperfect. Cell Tissue Res 339(1):59–70
Marklund U, Hansson E, Sundström E, Hrabě de Angelis M, Przemeck GKH et al (2010) Domain-specific control of neurogenesis achieved through patterned regulation of notch ligand expression. Development 137:437–445
Marks SC Jr, Lane PW (1976) Osteopetrosis, a new recessive skeletal mutation on chromosome 12 of the mouse. J Hered 67:11–18
Marx SJ, Attie MF, Levine MA, Spiegel AM, Downs RW Jr et al (1981) The hypocalciuric or benign variant of familial hypercalcemia: clinical and biochemical features in fifteen kindreds. Medicine 60(6):397–412
McGowan KA, Li JZ, Park CY, Beaudry V, Tabor HK et al (2008) Ribosomal mutations cause p53-mediated dark skin and pleiotropic effects. Nat Genet 40(8):963–970
Mejia-Gaviria N, Gil-Peña H, Coto E, Pérez-Menéndez TM, Santos F (2010) Genetic and clinical peculiarities in a new family with hereditary hypophosphatemic rickets with hypercalciuria: a case report. Orphanet J Rare Des 5:1–4
Moriyama K, Hanai A, Mekada K, Yoshiki A, Ogiwara K et al (2011) Kbus/Idr, a mutant mouse strain with skeletal abnormalities and hypophosphatemia: identification as an allele of ‘Hyp’. J Biomed Sci 18:60
Mornet E, Stura E, Lia-Baldini AS, Stigbrand T, Ménez A et al (2001) Structural evidence for a functional role of human tissue nonspecific alkaline phosphatase in bone mineralization. J Biol Chem 276(33):31171–31178
Moss DW (1994) Release of membrane-bound enzymes from cells and the generation of isoforms. Clin Chim Acta 226:131–142
Nakajima K, Yamazaki K, Kimura H, Takano K, Miyoshi H et al (2009) Novel gain of function mutations of the calcium-sensing receptor in two patients with PTH-deficient hypocalcemia. Intern Med 48(22):1951–1956
Narisawa S, Fröhlander N, Millan JL (1997) Inactivation of two mouse alkaline phosphatase genes and establishment of a model of infantile hypophosphatasia. Dev Dyn 208(3):432–446
Nicklas W, Baneux P, Boot R, Decelle T, Deeny AA et al (2002) Recommendations for the health monitoring of rodent and rabbit colonies in breeding and experimental units. Lab Anim 36(1):20–42
Panteghini M (1991) Benign inherited hyperphosphatemia of intestinal origin: report of two cases and a brief review of the literature. Clin Chem 37(8):1449–1452
Pedrazzoni M, Alfano FS, Girasole G, Giuliani N, Fantuzzi M et al (1996) Clinical observations with a new specific assay for bone alkaline phosphatase: a cross-sectional study in osteoporotic and pagetic subjects and a longitudinal evaluation of the response to ovariectomy, estrogens, and bisphosphonates. Calcif Tissue Int 59(5):334–338
Pollak MR, Brown EM, Chou YHW, Hebert SC, Marx SJ et al (1993) Mutations in the human Ca2+-sensing receptor gene cause familial hypocalciuric hypercalcemia and neonatal severe hyperparathyroidism. Cell 75:1297–1303
Pollak MR, Chou YHW, Marx SJ, Steinmann B, Cole DEC et al (1994) Familial hypocalciuric hypercalcemia and neonatal severe hyperparathyroidism. J Clin Invest 93(3):1108–1112
Rathkolb B, Decker T, Fuchs E, Soewarto D, Fella C et al (2000) The clinical-chemical screen in the Munich ENU mouse mutagenesis project: screening for clinically relevant phenotypes. Mamm Genome 11:543–546
Rauch DA, Hurchla MA, Harding JC, Deng H, Shea LK et al (2010) The ARF tumor suppressor regulates bone remodeling and osteosarcoma development in mice. PLoS One 5(12):e15755
Rubio-Aliaga I, Soewarto D, Wagner S, Klaften M, Fuchs H et al (2007) A genetic screen for modifiers of the delta-1-dependent notch signaling function in the mouse. Genetics 175(3):1451–1463
Segawa H, Onitsuka A, Kuwahata M, Hanabusa E, Furutani J et al (2009) Type IIc sodium-dependent phosphate transporter regulates calcium metabolism. J Am Soc Nephrol 20(1):104–113
Simon-Bouy B, Taillandier A, Fauvert D, Brun-Heath I, Serre JL et al (2008) Hypophosphatasia: molecular testing of 19 prenatal cases and discussion about genetic counseling. Prenat Diagn 28(11):993–998
Singer FR, Clemens TL, Eusebio RA, Bekker PJ (1998) Risedronate, a highly effective oral agent in the treatment of patients with severe Paget’s disease. J Clin Endocrinol Metab 83(6):1906–1910
Siraganian PA, Mulvihill JJ, Mulivor RA, Miller RW (1989) Benign familial hyperphosphatasemia. JAMA 261(9):1310–1312
Smits P, Bolton AD, Funari VM, Hong M, Boyden ED et al (2010) Lethal skeletal dysplasia in mice and humans lacking the golgin GMAP-210. N Engl J Med 362:206–216
Soewarto D, Fella C, Teubner A, Rathkolb B, Pargent W et al (2000) The large-scale Munich ENU-mouse-mutagenesis screen. Mamm Genome 11(7):507–510
Soewarto D, Klaften M, Rubio-Aliago I (2009) Features and strategies of ENU mouse mutagenesis. Curr Pharm Biotech 10:198–213
Srivastava AK, Bhattacharyya S, Li X, Mohan S, Baylink DJ (2001) Circadian and longitudinal variation of serum C-telopeptide, osteocalcin, and skeletal alkaline phosphatase in C3H/HeJ mice. Bone 29(4):361–367
Srivastava AK, Mohan S, Wergedahl JE, Baylink DJ (2003) A genomewide screening of N-ethyl-N-nitrosourea-mutagenized mice for musculoskeletal phenotypes. Bone 33:179–191
Strom TM, Jüppner H (2008) PHEX, FGF23, DMP1 and beyond. Curr Opin Nephrol Hypertens 17(4):357–362
Taillandier A, Cozien E, Muller F, Merrien F, Bonnin E et al (2000) Fifteen new mutations (-195C > T, L-12X, 298-2A > G, T117 N, A159T, R229S, 997+2T > A, E274X, A331T, H364R, D389G, 1256delC, R433H, N461I, C472S) in the tissue-nonspecific alkaline phosphatase (TNSALP) gene in patients with hypophosphatasia. Hum Mutat 15:292–293
Tenenhouse HS (1999) X-linked hypophosphataemia: a homologous disorder in humans and mice. Nephrol Dial Transpl 14:333–341
Tieder M, Modai D, Samuel R, Arie R, Halabe A et al (1985) Hereditary hypophosphatemic rickets with hypercalciuria. N Engl J Med 312(10):611–617
Tiosano D, Hochberg Z (2009) Hypophosphatemia: the common denominator of all rickets. J Bone Miner Metab 27(4):392–401
Wenkert D, McAlister WH, Coburn SP, Zerega JA, Ryan LM et al (2011) Hypophosphatasia: nonlethal disease despite skeletal presentation in utero (17 new cases and literature review). J Bone Miner Res 26(10):2389–2398
Whyte MP (2010) Physiological role of alkaline phosphatase explored in hypophosphatasia. Ann NY Acad Sci 1192(1):190–200
Xiong X, Qi X, Ge X, Gu P, Zhao J et al (2008) A novel Phex mutation with defective glycosylation causes hypophosphatemia and rickets in mice. J Biomed Sci 15(1):47–59
Acknowledgments
We thank Sandra Hoffmann, Andreas Mayer, Tommy Fuchs, Silvia Crowley, Annemieke Looienga, Elfi Holupirek, Jacqueline Mueller, Eleonore Samson, Sandy Lösecke, and Gerlinde Bergter for excellent technical assistance. We also thank Leticia Quintanella-Fendt for analysis of histologic images and Michael Roseman for scientific discussions. This work was supported by Nationales Genomforschungsnetz (NGFN 01GR0430), NGFNplus grants from the Bundesministerium für Bildung und Forschung (BMBF), (01GS0850 and 01GS0851), and BMBF OSTEOPATH grants (01EC1006B). The work was further supported by EU ANABONOS (LSH-2002-2.1.4-3) grants to MHdA.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
I. Rubio-Aliaga and W. Hans contributed equally to this study.
An erratum to this article is available at http://dx.doi.org/10.1007/s00335-014-9534-y.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Sabrautzki, S., Rubio-Aliaga, I., Hans, W. et al. New mouse models for metabolic bone diseases generated by genome-wide ENU mutagenesis. Mamm Genome 23, 416–430 (2012). https://doi.org/10.1007/s00335-012-9397-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00335-012-9397-z