Abstract
Objective
To accurately estimate liver PDFF from chemical shift-encoded (CSE) MRI using a deep learning (DL)-based Multi-Decoder Water-Fat separation Network (MDWF-Net), that operates over complex-valued CSE-MR images with only 3 echoes.
Methods
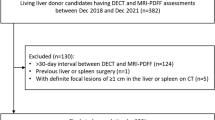
The proposed MDWF-Net and a U-Net model were independently trained using the first 3 echoes of MRI data from 134 subjects, acquired with conventional 6-echoes abdomen protocol at 1.5 T. Resulting models were then evaluated using unseen CSE-MR images obtained from 14 subjects that were acquired with a 3-echoes CSE-MR pulse sequence with a shorter duration compared to the standard protocol. Resulting PDFF maps were qualitatively assessed by two radiologists, and quantitatively assessed at two corresponding liver ROIs, using Bland Altman and regression analysis for mean values, and ANOVA testing for standard deviation (STD) (significance level: .05). A 6-echo graph cut was considered ground truth.
Results
Assessment of radiologists demonstrated that, unlike U-Net, MDWF-Net had a similar quality to the ground truth, despite it considered half of the information. Regarding PDFF mean values at ROIs, MDWF-Net showed a better agreement with ground truth (regression slope = 0.94, R2 = 0.97) than U-Net (regression slope = 0.86, R2 = 0.93). Moreover, ANOVA post hoc analysis of STDs showed a statistical difference between graph cuts and U-Net (p < .05), unlike MDWF-Net (p = .53).
Conclusion
MDWF-Net showed a liver PDFF accuracy comparable to the reference graph cut method, using only 3 echoes and thus allowing a reduction in the acquisition times.
Clinical relevance statement
We have prospectively validated that the use of a multi-decoder convolutional neural network to estimate liver proton density fat fraction allows a significant reduction in MR scan time by reducing the number of echoes required by 50%.
Key Points
• Novel water-fat separation neural network allows for liver PDFF estimation by using multi-echo MR images with a reduced number of echoes.
• Prospective single-center validation demonstrated that echo reduction leads to a significant shortening of the scan time, compared to standard 6-echo acquisition.
• Qualitative and quantitative performance of the proposed method showed no significant differences in PDFF estimation with respect to the reference technique.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a spectrum of disorders, that range from simple steatosis to non-alcoholic steatohepatitis and cirrhosis [1]. NAFLD is directly related to the hepatic fat content [1, 2] and, despite biopsy being the reference method to estimate liver fat, non-invasive modalities based on chemical shift-encoded (CSE) MRI have been increasingly used. This procedure allows the estimation of proton density fat fraction (PDFF), which has already been validated against pathology to determine the presence and grading of hepatic steatosis in patients with NAFLD [1].
To accurately estimate PDFF, the standardized techniques must address a water-fat separation problem considering the effect of a set of confounders, such as R2* (= 1/T2*) signal decay ratio, off-resonance field map (Δf), and multi-peak fat spectrum, as they have non-linear effects over the signal that complicate its separation [3,4,5].
Several water-fat separation algorithms that deal with these confounding factors have already been proposed [3, 6,7,8]. A graph cut–based method, that consists of a VARPRO formulation and an iterative Graph-Cut algorithm of considerable robustness and accuracy, is usually considered the gold standard [8, 9]. However, the required CSE-MR images, which are acquired using a multiple gradient echo pulse sequence, are usually obtained with 6 echoes, as this is the minimum recommended number in literature to achieve an improved R2* estimation [10]. Therefore, scan times could be significantly long and several patient breath holdings could be necessary during the procedure. Moreover, The graph cut method requires large computational resources and calculation time.
Recently, several deep learning (DL)–based methods have been proposed to address the water-fat separation problem [11,12,13,14,15]. To our knowledge, all these works have proposed convolutional neural networks (CNNs) with different configurations, although most of them [11, 12, 15] have implemented a U-Net architecture [16]. However, only one of them has included the estimation of R2* and Δf maps to discard them as confounding factors [15]. Moreover, only a couple of these works have performed an assessment using images with a reduced number of echoes [11, 12], which could suggest a possible reduction in the acquisition times. Nevertheless, the validation of reducing the number of echoes has not been thoroughly done, as the performance was not assessed using acquisitions of a shorter duration than the original protocol.
To achieve an effective shortening of the scan time, the repetition time (TR) of the pulse sequence must be optimized to maximize the acquired number of slices per breath-hold. Shortening of TR is known to generate a T1-weighting in the resulting MR signal and, as consequence, a positive PDFF bias. To avoid this bias, low flip angles are preferred at the cost of a drop in the signal intensity [17].
Recent DL applications for signal processing have implemented multi-task U-Net-based architectures to jointly perform more than one estimation from a single input [18, 19]. This configuration, which is a U-Net with multiple decoders, allows a more dedicated estimation of outputs with significantly different attributes (i.e., sharpness of structures, noise, etc.) without the need of developing two separate models for each task.
In this work, we propose a multi-task U-Net-based architecture, denoted as a multi-decoder water-fat separation neural network (MDWF-Net), to jointly estimate water-only and fat-only images, in addition to R2* and Δf maps. This multi-task approach allows for improving the estimation of water-fat images, which enables a reduction of the necessary echoes to achieve an accurate PDFF quantification. The main goal of this work was to achieve a liver PDFF estimation with an accuracy comparable to the reference 6-echo graph cut technique, using 3-echo images.
Materials and methods
The data for this study was acquired in a single center, with a 1.5-T MR scanner (Achieva, Philips Healthcare), and was HIPAA compliant.
Retrospective data
We first considered a set of previously collected CSE-MR abdomen images, which were obtained between 2017 and 2020. Data was obtained from 134 volunteers, each of them with a number of slices between 18 and 24, according to the whole liver coverage. Both healthy and fatty-liver subjects were considered. For non-healthy subjects, the inclusion criterion was suspicion of hepatic steatosis preliminarily evaluated by ultrasound. Additionally, fatty-liver subjects were considered only after discarding confounding conditions (i.e., history of other chronic liver diseases, significant alcohol consumption, and drug therapy).
These CSE-MR images were acquired with a standard 6-echo T1w-GRE protocol. During acquisition, patients were asked for breath-holding (10–13 breath-holds of approximately 10 s each), and complex-valued data was stored. The most relevant pulse sequence parameters were the following: TR = 30 [ms], TE1/ΔTE = 1.3/2.1 [ms], voxel-size = 0.89 × 0.89 × 10 [mm3], flip-angle = 10°. The remaining parameters are summarized in Table 1.
Prospectively acquired images
We scanned a second subset of healthy subjects (between 2021 and 2022) using the standard 6-echoes protocol and a 3-echoes acquisition. The 3-echoes pulse sequence considered the same echo times of the first 3 echoes of standard protocol, except for TR, which was optimized at each scan to maximize the number of acquired slices per breath-hold, leading to a reduction of the nominal scan time from 120 to 54 s. Pulse sequence parameters of the 3-echoes protocol are also summarized in Table 1.
Reference water-fat separation method
The voxel-wise physical model that describes the complex signal at the n-th echo (In) for a T1w-GRE sequence is:
where j is the imaginary unit, ρw and ρf are the water and fat signals, R2* is the transverse relaxation, Δf is the off-resonance field map, TEn is the n-th echo time, P is the number of fat spectral peaks, and fF,p are the frequencies of the fat spectral peaks, with their respective relative amplitudes αp (with Σαp = 1), which are known a priori [20]. Then, PDFF is calculated as:
Reference results of ρw, ρf, R2*, and Δf were obtained using the graph cut algorithm [8] implemented in the International Society of Magnetic Resonance in Medicine (ISMRM) water-fat Toolbox[21].
Multi-decoder water-fat separation network
MDWF-Net is a CNN [22, 23] capable of calculating water-fat images, R2* and ∆f after receiving multi-echo GRE acquisitions as input. The architecture of MDWF-Net is based on multi-task U-Net, which has been previously proposed in the literature for signal processing tasks [18, 19]. This configuration consists of an encoder-decoder structure that translates the input to a reduced-dimensions latent space of features, from which water-fat images, R2* and ∆f are separately decodified (Fig. 1).
A Architecture of MDWF-Net. An encoder structure (light blue) extract features from the multi-echo acquisitions, converging to the reduced-dimensions latent space (blue). From this latent space, three decoders translate these extracted features into water-fat images (green), R2* map (orange), and off-resonance field map (pink). B A similar U-Net architecture, with a single decoder to obtain the four outputs from the latent space
The encoder was comprised of 4 consecutive Conv2D blocks, which were composed of two bidimensional convolution operators (with N = 72, 144, 288, 576 convolutional filters) each followed by ReLU activation function and Batch Normalization. The resulting Conv2D blocks features were downsampled using 2D max pooling, to finally obtain the latent space, which consisted of 1152 features of 12 × 12 dimensions. In the decoders, latent space features were upsampled using transposed bidimensional convolutions and then concatenated with the equally shaped encoder features. The concatenated features were then processed through the same Conv2D blocks used in the encoder. For Δf decoder, the first upsampling from the latent space was followed by the application of a self-attention block [24,25,26] that enabled the learning of spatial relationships between non-neighboring pixels. This additional self-attention block was expected to improve the suppression of swapping artifacts. Therefore, we expected MDWF-Net to overperform the already studied U-Net [11, 12, 15] (Fig. 1B), as it gives a more dedicated approach to the specific features of each output.
The input for MDWF-Net was arrays composed of multiple echoes of a single rescaled 2D slice of the abdomen. All CSE-MR images were rescaled to 192 × 192 by k-space subsampling, and each array channel contained the real and imaginary components of each echo. Therefore, for 3-echoes acquisitions, the input array dimensions were 192 × 192 × 6. On the other hand, MDWF-Net returned three outputs: a 2-channels array with the magnitude water-fat images, and two single-channel arrays with the R2* and the Δf maps, respectively.
Experiments
Previously acquired data were considered for training (N = 2479 slices) and validation during training (N = 384), while prospective data were reserved for testing. As previous data included 6-echoes images, and it would have been non-viable to re-scan each of the previously acquired volunteers using the 3-echo protocol, only the first 3 echoes were considered during training.
All samples were labeled with graph cut results obtained from 6-echo images. Both MR images and labels were masked using thresholding over the mean of all-echoes magnitude images for noisy background removal. To set the R2* and Δf values in the range of [0,1], we normalized the reference variables by 200 [s−1] and 400 [Hz], respectively.
The training process elapsed 120 epochs, considering a batch size of 32 and an initial learning rate of 5 × 10–4 with a cosine decay. The considered loss function was the mean-absolute-error (MAE) to reference results. We also trained a U-Net (similar implementation of [12]) under the same conditions and hyperparameters configuration, which computed a 4-channel output, each of them corresponding to ρw, ρf, R2*, and Δf. Similar to MDWF-Net, U-Net weights were randomly initialized and posteriorly fitted considering the same training samples.
The pre-processing of the data (DICOM reading, rescaling, and graph cut estimations) was performed in MATLAB (MathWorks), and DL-based models were implemented using the TensorFlow framework [27]. Further details about the training process can be found in the Supplementary Material.
Subjective analysis
PDFF maps were visually rated blinded and independently by two experienced radiologists (C.B., J.U., with 10 and 3 years of experience in Body MR, respectively), for a qualitative comparison with the reference method. Complete multi-slice abdomen PDFF maps, provided in DICOM format, were assessed in terms of overall image quality, perceived SNR, and artifacts using a 5-point Likert scale (Table 2).
Quantitative and statistical analysis
To quantitatively assess PDFF estimation performance, we located two specific regions of interest (ROI) of ~ 2 cm2 in the liver parenchyma, at the right posterior and left hepatic lobes (RHL and LHL, respectively) at the level of the portal bifurcation (Fig. 2A). ROIs were drawn with the assistance of evaluating radiologists, avoiding large vessels, liver lesions, and artifacts, at the same position in the liver. Once the location of each ROI was determined, all of them were co-localized on the maps obtained with each method.
Posteriorly, to assess the bias and blurring of each method, we computed the mean and standard deviation (STD) of PDFF at each ROI. For assessing agreement with ground truth (6-echoes graph cuts), we performed least squares (LS) regression correlation and Bland Altman analysis for mean PDFF values. Additionally, an ANOVA post hoc test was performed to assess differences between PDFF STD values. For this statistical analysis, both ROIs were analyzed together, due to the reduced number of samples. A significance level of 0.05 was considered, and all statistical tests were performed in R (R Development Core Team; https://www.R-project.org). Assessment of R2* maps can be found in the Supplementary Material.
A repository with all the used codes is available at https://github.com/jpmeneses/MDWF-Net.
Results
Demographics of the considered subjects
Previously acquired 134 subjects showed the following demographics: mean age, 32.5 ± 18.1 years old; inter-quartile range, 36 years old; 99 women. This first database covered a wide range of body mass index (30.0 ± 5.0 kg/m2) and distribution of ground-truth PDFF values at RHL and LHL (Fig. 2B).
Additionally, after discarding a single subject due to the presence of several liver cysts, we scanned 13 subjects (mean age, 34.4 ± 13.8 years old; inter-quartile range, 11 years old; 5 women) with both original and 3-echoes protocol (N = 290). Although the mean body mass index was lower than the training dataset (25.4 ± 2.2 kg/m2), we observed three volunteers whose reference liver PDFF was over 20%.
A detailed description of the demographics of both datasets is shown in Table 3.
Computation times
Both CNNs were trained using a Quadro RTX 8000 graphics processing unit (GPU) and tested in a smaller GPU (GeForce GTX 1050) to consider more accessible hardware conditions. Both training processes elapsed ~ 5 h. Once they were trained, mean computation times were 0.07 [s/slice] for U-Net, and 0.13 [s/slice] for VET-Net, compared to 15.58 [s/slice] for 6-echo graph cuts.
Qualitative analysis
In Fig. 3, we displayed the outputs (ρw, ρf, R2*, Δf) for representative slices of testing subjects that were obtained with the graph cuts (using CSE-MR images obtained with the original protocol), and DL-based methods (using 3-echoes images). Figure 3A showed a specific case in which some swapping artifacts were observed in the left anterior part of the liver. In Fig. 3B, we displayed a case in which the TR of the 3-echo pulse sequence was shorter (13.3 ms) than in the original protocol (30.0 ms).
Assessment of radiologists indicated that MDWF-Net and U-Net achieved PDFF maps of similar quality to graph cuts, according to overall IQ scores (U-Net: 3.44 ± 0.80, MDWF-Net: 3.54 ± 0.86, graph cuts: 3.55 ± 0.98). In terms of SNR, both CNNs also achieved similar performance to 6-echo graph cuts (U-Net: 3.27 ± 0.99, MDWF-Net: 3.32 ± 0.76, graph cuts: 3.30 ± 0.88). Moreover, MDWF-Net achieved slightly higher mean artifact reduction scores than 6-echo graph cuts (U-Net: 3.68 ± 0.61; MDWF-Net: 3.66 ± 0.61; graph cuts: 3.56 ± 0.66). All mean PDFF scores are summarized in Table 4.
The distribution of PDFF overall IQ scores showed that almost half of the PDFF maps obtained with MDWF-Net were graded with overall IQ scores ≥ 4, unlike U-Net, for which more than half of the samples had a score of 3 (Fig. 4).
ROI analysis and statistical tests
Least squares regression correlation analysis of mean PDFF values at ROIs indicated that MDWF-Net showed a better agreement with respect to 6-echo graph cuts (regression slope: 0.94, R2: 0.97) than U-Net (regression slope: 0.86, R2: 0.93) (Fig. 5). Similarly, Bland Altman analysis showed that MDWF-Net presented a lower bias and narrower LoA (bias: 0.24%; LoA: − 2.36%,2.84%) than U-Net (bias: − 0.27%; LoA: − 4.20%,3.66%).
In the specific case of a short TR subject (same as Fig. 3B), MDWF-Net showed a positive bias of 1.53% and 1.13% in RHL and LHL, while U-Net displayed a bias of 2.00% and 0.94%, respectively.
To assess the blurring of PDFF estimations, the ANOVA post hoc test considering PDFF-STD values at each ROI suggested that there was a significant difference between U-Net and ground-truth (p = 0.0250), unlike MDWF-Net, which has no significative difference with respect to the reference (p = 0.5323) (Fig. 6).
Discussion
In this study, we compared the performance of two DL-based methods, our proposed MDWF-Net and a U-Net, an architecture whose performance in MR water-fat separation had been already studied in the literature. For a fair comparison, both CNNs were trained under the same conditions (equal training datasets, same hyperparameters).
Visual assessment of the CNNs outputs showed that, unlike U-Net, MDWF-Net could alleviate some swapping artifacts observed in Fig. 3A. However, we also noticed that both DL-based R2* maps were more blurred than the reference, which was evident in the vascular liver structures. This was expectable, as for most water-fat separation techniques, R2* is the most affected variable when the number of echoes is reduced, and usually up to 12 echoes are suggested for a reliable R2* estimation [10]. In Fig. 3B, we observed that there was no T1-weighting effect when the TR of 3-echo pulse sequence was shorter (13.3 ms) than in the original protocol (30.0 ms).
The reader should notice that we did not quantitatively assess overall maps, such as the ones displayed in Fig. 3, because reference and MDWF-Net results originated from MR images acquired with different protocols and in different instances, which may produce different features (structures, field inhomogeneities, motion, etc.). Therefore, we used a hold-out validation scheme and not a k-fold cross-validation as usually performed in these studies. To quantitatively assess differences, MAE between MDWF-Net and U-Net results, which were obtained from the same 3-echo protocol, was included in Supplementary Material.
Evaluation of radiologists showed that both MDWF-Net and U-Net slightly overperformed the reference method in terms of artifact reduction and perceived SNR scores. Similarly, MDWF-Net showed a visual quality comparable to graph cuts, as demonstrated by the mean overall scores, although our proposed method used less information.
The quantitative assessment showed that MDWF-Net overperformed U-Net in PDFF estimation, as showed by the higher correlation with respect to 6-echo graph cut estimations. MDWF-Net also achieved a reduced bias and a narrower LoA than U-Net. Moreover, and in agreement with radiologists’ assessment, MDWF-Net reduced blurring artifacts compared to U-Net, as demonstrated by the ANOVA post hoc analysis. This behavior was expectable, as loss in texture details has been previously reported for U-Net [14].
We believe that the improved PDFF estimation of MDWF-Net was a consequence of multi-task architecture, in which the encoder weights (used to compute the shared encoder features) were adjusted considering the decoder weights of each output. As each output, water/fat images, R2*, Δf, has a different range and meaning, the use of separated decoders in MDWF-Net improved PDFF estimation compared to U-Net, due to an improved estimation of R2* and Δf effects.
Additionally, we observed that a reduced TR in 3-echo protocol did not significantly affect MDWF-Net performance, probably due to the use of small flip angles [17]. Nevertheless, a limitation of this study was the reduced number of subjects acquired with a shorter TR than the standard protocol. Future work will thoroughly assess T1-weighting bias in a larger group of subjects with few echoes, short TR, and variable flip angles.
Although a quantitative comparison of R2* and Δf between both CNNs was included in Supplementary Material, further validation is part of our future work, as both values could have clinical value. While R2* is potentially useful to diagnose hepatic iron overload [28], Δf maps are used to estimate quantitative susceptibility mapping (QSM) [29, 30]. Nevertheless, this latter application would be necessary to use 3D CSE-MR images.
Incoming work will be focused on adequately assessing the robustness of the proposed method, which is a relevant aspect of translation to clinical practice. MDWF-Net needs to be validated using CSE-MR images of phantoms and subjects acquired using scanners from different vendors.
Conclusion
MDWF-Net enables a highly accurate estimation of liver PDFF, with a performance comparable to graph cuts, using half of the data necessary for the latter technique. This induces a significant shortening of the acquisition time, and therefore a reduction of the breath-holds necessary during the procedure. The favorable assessment of expert radiologists and the absence of statistically significant differences in gold standards demonstrated that the proposed method is a reliable liver fat quantification tool for clinical use.
Abbreviations
- CNN:
-
Convolutional neural network
- CSE:
-
Chemical shift-encoded
- DL:
-
Deep learning
- GRE:
-
Gradient-echo
- LHL:
-
Left hepatic lobe
- MAE:
-
Mean-absolute-error
- MDWF-Net:
-
Multi-decoder water-fat separation network
- NAFLD:
-
Non-alcoholic fatty liver disease
- PDFF:
-
Proton density fat fraction
- RHL:
-
Right hepatic lobe
- TR:
-
Repetition time
References
Idilman IS, Aniktar H, Idilman R et al (2013) Hepatic steatosis: quantification by proton density fat fraction with MR imaging versus liver biopsy. Radiology 267:767–775. https://doi.org/10.1148/radiol.13121360
Starekova J, Reeder SB (2020) Liver fat quantification: where do we stand? Abdom Radiol (NY) 45:3386–3399. https://doi.org/10.1007/s00261-020-02783-1
Reeder SB, Wen Z, Yu H et al (2004) Multicoil dixon chemical species separation with an iterative least-squares estimation method. Magn Reson Med 51:35–45. https://doi.org/10.1002/mrm.10675
Reeder SB, Cruite I, Hamilton G, Sirlin CB (2011) Quantitative assessment of liver fat with magnetic resonance imaging and spectroscopy. J Magn Reson Imaging 34:729–749. https://doi.org/10.1002/jmri.22580
Colgan TJ, Zhao R, Roberts NT et al (2021) Limits of fat quantification in the presence of iron overload. J Magn Reson Imaging 54:1166–1174. https://doi.org/10.1002/jmri.27611
Yu H, Shimakawa A, McKenzie CA et al (2008) Multiecho water-fat separation and simultaneous R*2 estimation with multifrequency fat spectrum modeling. Magn Reson Med 60:1122–1134. https://doi.org/10.1002/mrm.21737
Jaubert O, Arrieta C, Cruz G, et al (2020) Multi-parametric liver tissue characterization using MR fingerprinting: simultaneous T1, T2, T2* and fat fraction mapping. Magn Reson Med mrm.28311. https://doi.org/10.1002/mrm.28311
Hernando D, Kellman P, Haldar JP, Liang ZP (2010) Robust water/fat separation in the presence of large field inhomogeneities using a graph cut algorithm. Magn Reson Med 63:79–90. https://doi.org/10.1002/mrm.22177
Hernando D, Liang ZP, Kellman P (2010) Chemical shift-based water/fat separation: a comparison of signal models. Magn Reson Med 64:811–822. https://doi.org/10.1002/mrm.22455
Yu H, McKenzie CA, Shimakawa A et al (2007) Multiecho reconstruction for simultaneous water-fat decomposition and T2* estimation. J Magn Reson Imaging 26:1153–1161. https://doi.org/10.1002/jmri.21090
Andersson J, Ahlström H, Kullberg J (2019) Separation of water and fat signal in whole-body gradient echo scans using convolutional neural networks. Magn Reson Med 82:1177–1186. https://doi.org/10.1002/mrm.27786
Goldfarb JW, Craft J, Cao JJ (2019) Water–fat separation and parameter mapping in cardiac MRI via deep learning with a convolutional neural network. J Magn Reson Imaging 50:655–665. https://doi.org/10.1002/jmri.26658
Cho JJ, Park HW (2019) Robust water–fat separation for multi-echo gradient-recalled echo sequence using convolutional neural network. Magn Reson Med 82:476–484. https://doi.org/10.1002/mrm.27697
Liu K, Li X, Li Z, et al (2020) Robust water–fat separation based on deep learning model exploring multi-echo nature of mGRE. Magn Reson Med 1–14. https://doi.org/10.1002/mrm.28586
Jafari R, Spincemaille P, Zhang J et al (2021) Deep neural network for water/fat separation: supervised training, unsupervised training, and no training. Magn Reson Med. https://doi.org/10.1002/mrm.28546
Ronneberger O, Fischer P, Brox T (2015) U-net: convolutional networks for biomedical image segmentation. Lect Notes Computer Sci (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics) 9351:234–241. https://doi.org/10.1007/978-3-319-24574-4_28
Peterson P, Svensson J, Månsson S (2014) Relaxation effects in MRI-based quantification of fat content and fatty acid composition. Magn Reson Med 72:1320–1329. https://doi.org/10.1002/mrm.25048
Jha A, Kumar A, Pande S et al (2020) MT-UNET: a novel U-Net based multi-task architecture for visual scene understanding. 2020 IEEE International Conference on Image Processing (ICIP) 2191–2195. https://doi.org/10.1109/ICIP40778.2020.9190695
Lee GW, Kim HK (2020) Multi-task learning U-Net for single-channel speech enhancement and mask-based voice activity detection. Appl Sci (Switzerland) 10:. https://doi.org/10.3390/app10093230
Hamilton G, Yokoo T, Bydder M et al (2011) In vivo characterization of the liver fat 1H MR spectrum. NMR Biomed 24:784–790. https://doi.org/10.1002/nbm.1622
Hu HH, Börnert P, Hernando D et al (2012) ISMRM workshop on fat-water separation: insights, applications and progress in MRI. Magn Reson Med 68:378–388. https://doi.org/10.1002/mrm.24369
Shin HC, Roth HR, Gao M et al (2016) Deep convolutional neural networks for computer-aided detection: CNN architectures, dataset characteristics and transfer learning. IEEE Trans Med Imaging 35:1285–1298. https://doi.org/10.1109/TMI.2016.2528162
Albawi S, Mohammed TA, Al-Zawi S (2018) Understanding of a convolutional neural network. Proceedings of 2017 International Conference on Engineering and Technology, ICET 2017 2018-Janua:1–6. https://doi.org/10.1109/ICEngTechnol.2017.8308186
Vaswani A, Shazeer N, Parmar N et al (2017) Attention is all you need. Advances in Neural Information Processing Systems 30:5999–6009
Zhang H, Goodfellow I, Metaxas D, Odena A (2019) Self-attention generative adversarial networks. Proceedings of the 36th International Conference on Machine Learning 97:7354–7363
Ramachandran P, Bello I, Parmar N et al (2019) Stand-alone self-attention in vision models. Advances in Neural Information Processing Systems 32
Abadi M, Barham P, Chen J et al (2016) TensorFlow: a system for large-scale machine learning. Proceedings of the 12th USENIX Symposium on Operating Systems Design and Implementation 16:265–283
Wood JC, Enriquez C, Ghugre N et al (2005) MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood 106:1460–1465. https://doi.org/10.1182/blood-2004-10-3982
Jafari R, Sheth S, Spincemaille P et al (2019) Rapid automated liver quantitative susceptibility mapping. J Magn Reson Imaging 50:725–732. https://doi.org/10.1002/jmri.26632
Lin H, Wei H, He N et al (2018) Quantitative susceptibility mapping in combination with water-fat separation for simultaneous liver iron and fat fraction quantification. Eur Radiol. https://doi.org/10.1007/s00330-017-5263-4
Acknowledgements
This work was funded by ANID – Millennium Science Initiative Program – ICN2021_004, and also received the Chilean government through the Fondo Nacional de Desarrollo Científico y Tecnológico (FONDECYT 1191145 to MA). J.P.M. was funded by the National Agency for Research and Development (ANID) / Scholarship Program / DOCTORADO BECAS CHILE/2020 – 21210665. C.A. was partially funded by ANID FONDECYT Postdoctorado 2019 #3190763. C.T. was funded by Fondecyt 1231535, Anillo PIA ACT192064. S.U. was funded by Fondecyt 1181057.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions This work was funded by ANID – Millennium Science Initiative Program – ICN2021_004, and also received the Chilean government through the Fondo Nacional de Desarrollo Científico y Tecnológico (FONDECYT 1191145 to MA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Sergio Uribe.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained from the Scientific Ethical Committee of the Pontifical Catholic University of Chile.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in Verdejo et al, Similar Metabolic Health in Overweight/Obese Individuals with Contrasting Metabolic Flexibility to an Oral Glucose Tolerance Test (Frontiers in Nutrition, 2021).
In this prior study, that included J.E.G. as co-author, there were reported on 22 subjects of the current work. The prior report compared metabolic health in individuals with contrasting metabolic flexibility to an oral glucose tolerance test. The current study considered the MR data acquired in this previous work for monitoring abdominal fat.
Methodology
• Retrospective
• Observational study
• Performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meneses, J.P., Arrieta, C., della Maggiora, G. et al. Liver PDFF estimation using a multi-decoder water-fat separation neural network with a reduced number of echoes. Eur Radiol 33, 6557–6568 (2023). https://doi.org/10.1007/s00330-023-09576-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09576-2