Abstract
Objectives
The purpose of this study was to evaluate the diagnostic accuracy of third-generation dual-source dual-energy CT (DECT) color-coded collagen reconstructions for the assessment of the cruciate ligaments compared to standard grayscale image reconstruction.
Methods
Patients who underwent third-generation dual-source DECT followed by either 3-T MRI or arthroscopy of the knee joint within 14 days between January 2016 and December 2021 were included in this retrospective study. Five radiologists independently evaluated conventional grayscale DECT for the presence of injury to the cruciate ligaments; after 4 weeks, readers re-evaluated the examinations using grayscale images and color-coded collagen reconstructions. A reference standard for MRI was provided by a consensus reading of two experienced readers and arthroscopy. Sensitivity and specificity were the primary metrics of diagnostic performance.
Results
Eighty-five patients (mean age, 44 years ± 16; 50 male) with injury to the ACL or PCL (n = 31) were ultimately included. Color-coded collagen reconstructions significantly increased overall sensitivity (94/105 [90%] vs. 67/105 [64%]), specificity (248/320 [78%] vs. 215/320 [67%]), PPV (94/166 [57%] vs. 67/162 [39%]), NPV (248/259 [96%] vs. 215/253 [85%]), and accuracy (342/425 [81%] vs. 282/425 [66%]) for the detection of injury to the anterior cruciate ligament (all parameters, p < .001). For injury to the posterior cruciate ligament, diagnostic accuracy increased for complete tears (p < .001). Color-coded collagen reconstructions achieved superior diagnostic confidence, image quality, and noise scores compared to grayscale CT (all parameters, p < .001) and showed good agreement with MRI examinations.
Conclusions
DECT-derived color-coded collagen reconstructions yield substantially higher diagnostic accuracy and confidence for assessing the integrity of the cruciate ligaments compared to standard grayscale CT in patients with acute trauma.
Key Points
• Color-coded collagen reconstructions derived from dual-energy CT yield substantially higher diagnostic accuracy and confidence for the assessment of the cruciate ligaments compared to standard grayscale CT in patients with acute trauma.
• Color-coded collagen reconstructions demonstrate good agreement with MRI for the assessment cruciate ligament injury.
• Dual-energy CT may serve as a readily available screening approach for patients with acute trauma to the knee when injury to the cruciate ligaments is suspected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cruciate ligaments are major stabilizers of the knee joint. They prevent excessive anterior and posterior translation and restrain tibial rotation, varus stress, and valgus stress [1]. Injury to the anterior cruciate ligament (ACL) is common, with reported incidences of up to 1147 per 100,000 in the general population, and higher incidences among athletes [2, 3]. Isolated injury to the posterior cruciate ligament (PCL) is relatively rare [4].
Cruciate ligament injury can be managed surgically and nonoperatively. In younger patients and athletes, surgical reconstruction of injured cruciate ligaments is generally performed to enable continued high levels of physical activity. Early reconstruction of the ACL reduces the risk of subsequent injury to other soft tissue structures of the knee and improves long-term knee motion compared to delayed reconstruction [5,6,7,8]. Furthermore, early ACL reconstruction reduces the time before patients can return to full physical activity, which reduces associated socioeconomic burdens [9].
MRI is the reference standard for imaging of the cruciate ligaments [10]. However, availability of MRI is usually limited during on-call times, which can delay adequate treatment and recovery. Furthermore, MRI is not available for certain patients due to contraindications. CT is readily available to assess musculoskeletal trauma and usually performed in case of complex injuries to the knee or when conventional radiographs do not demonstrate pathology but injury to the knee joint is suspected. In this context, single-energy CT has been shown to provide insufficient soft-tissue contrast and resolution for assessing injury to the cruciate ligaments [11].
Material differentiation and collagen mapping in dual-energy CT (DECT) increase the quality of soft tissue visualization and provide novel information for different musculoskeletal applications compared to conventional single-energy CT [12,13,14,15,16,17,18]. Increased diagnostic value of second-generation dual-source grayscale DECT over conventional single-energy CT for assessing the cruciate ligaments has been demonstrated in initial pilot studies that used a simplified approach, with restrictions to complete tears of the cruciate ligaments and an emphasis on monochromatic images [19, 20]. With the advent of third-generation dual-source DECT, increased spatial resolution and advancements in material differentiation have further improved the possibilities for the assessment of soft tissue structures [21, 22]. In this context, a novel postprocessing algorithm visualizing collagenous structures by application of dedicated material decomposition has been developed [17]. In contrast to most DECT applications, this algorithm does not identify collagen based on the atomic number of contained hydrogen, carbon, nitrogen, and oxygen, but rather on the characteristic attenuation of the densely packed hydroxylysine and hydroxyproline in the collagen side chains, which can be decomposed against water and soft tissue [23, 24]. However, this algorithm has not yet been investigated for evaluation of the cruciate ligaments. Therefore, the purpose of this study was to evaluate the diagnostic accuracy and reader confidence of third-generation dual-source DECT color-coded collagen reconstructions for assessing the cruciate ligaments compared to standard grayscale CT.
Materials and methods
The institutional review board approved this retrospective study. The requirement to obtain written informed consent was waived. C.B. and I.Y. received speaking fees from Siemens Healthineers. The other authors have no conflict of interest to disclose.
Patient selection
One hundred consecutive patients over the age of 18 years with acute injury (within 3 days of trauma) to the knee who had undergone non-contrast third-generation dual-source DECT between January 2016 and December 2021, followed by supplementary MRI and/or arthroscopic inspection of the knee joint within 14 days, were considered for study inclusion. Exclusion criteria were suspected or known malignancy, inflammatory conditions, and inadequate imaging quality due to metallic implants.
CT protocol
CT studies were performed on a third-generation dual-source CT system in dual-energy mode (SOMATOM Force; Siemens Healthineers). Both X-ray tubes operated at different kilovoltage settings (tube A: 90 kVp, 180 mAs; tube B: Sn150 kVp [0.64-mm tin filter], 180 mAs). All examinations were performed without the administration of a contrast agent. Three image sets were acquired in each CT examination: 90 kVp, Sn150 kVp, and weighted average (ratio, 0.5:0.5) to resemble single-energy 120 kVp images. Image series (axial, coronal, and sagittal: section thickness 1 mm, increment 0.75 mm) were reconstructed with dedicated dual-energy bone (Br69f) and soft-tissue kernels (Br40). The image series were automatically transferred to the picture archiving and communication system (PACS; GE Healthcare).
CT postprocessing
Color-coded collagen reconstruction was performed on a Siemens syngo.via VB50 (Siemens Healthineers) using an experimental, not publicly available algorithm with the following default settings:
-
Application profile = Knee; Settings = Collagen; Public Layout = Fat Map; Width = 63; Level = − 32.
For image analysis, axial, coronal, and sagittal color-coded reconstructions (section thickness 1 mm, increment 0.75 mm) were sent to the PACS (GE Healthcare). Reconstruction time was measured from launching Siemens syngo.via until image export to the PACS system was initiated.
MRI protocol
MRI was performed on a 3-Tesla system (PrismaFit, Siemens Healthineers). Examinations included non-contrast T1-weighted turbo spin-echo sequences with and without fat suppression and proton density-weighted sequences with and without fat suppression, all in the transversal, sagittal, and coronal planes (ST: 3 mm). Pulse sequence parameters (echo time, repetition time, flip angle), FOV, and acquisition matrix were adapted for every examination.
Image analysis
Image evaluation was performed with a conventional PACS workstation (Centricity 7.0; GE Healthcare).
Two board-certified radiologists (K.E. and T.J.V.) with 17 and 35 years of experience in musculoskeletal imaging independently performed a reading of all MRI series to provide an independent reference standard. In case of disagreement (n = 2), a third board-certified radiologist (T.G.) with 11 years in musculoskeletal imaging was consulted. ACL and PCL were evaluated separately (1 = rupture certainly absent, 2 = total rupture, 3 = partial rupture, 4 = avulsion).
A consecutive reading of all CT images was independently performed by five radiologists (3 board-certified radiologists (C.B., I.Y., and S.M.)) and two radiologists in training (L.G., V.K.) with 1 to 7 years of experience in musculoskeletal imaging. These readers were blinded to clinical data, imaging results, and follow-up examinations. Two protocols were provided for the assessment of the cruciate ligaments: protocol 1 = standard grayscale images in axial, coronal, and sagittal plane; and protocol 2 = standard grayscale images and color-coded collagen reconstructions in axial, coronal, and sagittal plane as described above. Preset window settings could be freely modified. To reduce observer recall bias, a time interval of 4 weeks was kept between readout sessions and all images were presented in random order for both readouts. Readers reviewed both protocols for the presence of injury to the ACL and PCL (1 = rupture certainly absent, 2 = total rupture, 3 = partial rupture, 4 = avulsion).
Furthermore, readers rated their overall diagnostic confidence in the assessment of cruciate ligament injury as well as the image quality (including soft-tissue contrast, resolution, and artifacts) and image noise (ranging from 1 = poor to 5 = excellent) for each imaging protocol and patient.
Arthroscopy
Arthroscopy was performed by two board-certified orthopedic surgeons (V.H. and K.Z.) with 8 and 17 years of experience.
Statistical analysis
Statistical analysis was performed with dedicated commercial software (Prism 9 for macOS, version 9.0.1, GraphPad Software LLC; MedCalc for Windows, Version 20.022, MedCalc). Differences in baseline characteristics were assessed using t-tests, if applicable, or Chi-squared tests. Inter-reader agreement was evaluated by computing weighted Fleiss’ κ. Agreement between MRI and both imaging protocols was evaluated by computing Cohens’ κ.
Imaging findings were analyzed individually for each type of injury to the cruciate ligament, as mentioned above. Furthermore, analysis was performed after lesions were dichotomized (0 = injury absent, 1 = injury present). Findings were compiled in cross-tables, and diagnostic accuracy parameters (sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and area under the curve (AUC)) for the detection of injury to the cruciate ligaments were calculated. Receiver operator characteristic (ROC) curve comparison was used to determine the incremental diagnostic value of color-coding over grayscale imaging. Statistical significance was given if p < 0.05.
Results
Of 100 patients considered for study inclusion, 15 patients were excluded due to suspected or known malignancy (n = 4), inflammatory conditions (n = 3), and inadequate imaging quality due to metallic implants (n = 8) (Fig. 1). Therefore, a total of 85 patients who had undergone non-contrast third-generation dual-source DECT of the knee joint followed by MRI (n = 78) or arthroscopic inspection (n = 34) were finally included in this study (50 male and 35 female, mean age, 44 ± 16 years; range, 14–89 years; Table 1). Seven patients did not undergo MRI prior to arthroscopy. Both MRI and arthroscopic inspection were available as a reference standard in 27 patients. In two of these patients, arthroscopy revealed partial rupture of the ACL that were missed in MRI. No lesions of the PCL were missed in MRI. Together, the reference standards revealed an injury to the ACL in 21 patients (24.7%; complete tear = 11; partial tear = 4; avulsion fracture = 6) and the PCL in 10 patients (12.9%; complete tear = 1; partial tear = 0; avulsion fracture = 9). One patient had injury to the ACL and PCL. Using only MRI as the reference standard revealed injury to the ACL in 19 patients (complete tear = 11; partial tear = 2; avulsion = 6) and to the PCL in 10 patients (complete tear = 1; avulsion fracture = 9). No statistical significance was observed between the demographics of patients with injury to the cruciate ligaments and patients without injury. Patient characteristics are summarized in Table 1. The mean interval between dual-energy CT and MRI or arthroscopic inspection was 6 days (range, 0–13 days). Color-coded image reconstruction took on average 3 min (range, 1–5 min). An example case without injury to the cruciate ligaments is given in Fig. 2.
Standard sagittal unenhanced grayscale CT (A, D), color-coded collagen reconstructions (B, E), and unenhanced proton density-weighted MRI series with fat saturation (C, F) of a 28-year-old patient with acute knee pain following a bicycle accident demonstrate intact anterior (arrows) and posterior cruciate ligaments (arrowheads). The collagen signal is visualized blue by using default postprocessing settings
Diagnostic accuracy of ACL injury
Protocol 2 including color-coded collagen reconstructions of the ACL showed higher overall sensitivity (94/105 [90%] vs. 67/105 [64%]), specificity (248/320 [78%] vs. 215/320 [67%]), PPV (94/166 [57%] vs. 67/162 [39%]), NPV (248/259 [96%] vs. 215/253 [85%]), accuracy (342/425 [81%] vs. 282/425 [66%]), and AUC (0.84 vs 0.66) for the detection of injury to the ACL compared to protocol 1 comprising standard grayscale CT images alone (all comparisons, ΔAUC = 0.18, p < 0.001, Table 2). Inter-reader agreement was excellent for both protocols (κ = 0.84 for protocol 1 and κ = 0.85 for protocol 2), but only moderate between protocol 1 and protocol 2 (κ = 0.52). Notably, increases in AUC between protocol 1 and protocol 2 were highest for complete ACL tears (0.85 vs. 0.52, ΔAUC = 0.33, p < 0.001) and partial ACL tears (0.75 vs. 0.53, ΔAUC = 0.22, p = 0.02), whereas no significant difference was observed for avulsions of the ACL (0.68 vs. 0.63, ΔAUC = 0.05, p = 0.14). Diagnostic accuracy parameters did not change significantly when arthroscopy was excluded as a reference standard. Agreement between MRI and protocol 2, including color-coded collagen reconstructions, was higher compared to agreement between MRI and protocol 1 for all injuries (Table 3). Example cases demonstrating improvement in the detection of complete and partial ACL tears by color-coded collagen reconstructions are illustrated in Figs. 3 and 4.
Standard sagittal unenhanced grayscale CT (A, B), color-coded collagen reconstructions (C), and proton density-weighted unenhanced MRI series with fat saturation (D) of a complete tear (arrows) of the anterior cruciate ligament (ACL) in the cranial part in a 31-year-old professional kickboxer who repeatedly twisted her knee during kickboxing and presented to the emergency department with knee pain on Friday night immediately after training. Standard grayscale CT images showed no presence of fracture. However, a subtle inhomogeneity of the ACL in the cranial aspect (arrowhead) was noted. Color-coded collagen maps showed a distinct lack of collagen signal in this area (arrow) indicating a complete tear of the ACL. Subsequently, the additionally performed MRI confirmed the diagnosis, which was treated the next morning by arthroscopic repair. Abbreviations: ACL, anterior cruciate ligament
Standard sagittal unenhanced grayscale CT, color-coded collagen reconstructions, and arthroscopy images of a partial tear of the anterior cruciate ligament (ACL) in a 23-year-old patient who twisted his knee playing football. The ACL was considered as completely intact by the radiologists in this study using the standard grayscale CT (A). However, color-coded collagen reconstruction maps showed reduced and thinned blue collagen signal close to the tibial insertion (arrow) in terms of a partial tear (B), which was confirmed by the subsequently performed arthroscopy (arrow) (C). Abbreviations: ACL, anterior cruciate ligament
Comparing all CT readers, the least experienced radiologists showed a greater improvement in diagnostic accuracy for the detection of ACL injury compared to more experienced readers with higher overall sensitivity (20/21 [95%] vs. 12/21 [57%]), specificity (52/64 [81%] vs. 41/64 [64%]), PPV (20/34 [63%] vs. 12/35 [34%]), NPV (52/51 [98%] vs. 41/50 [82%]), and accuracy (72/85 [85%] vs. 53/85 [62%], all comparisons, p < 0.001) (Supplementary Table 1).
Diagnostic accuracy of PCL injury
Protocol 2, which included color-coded collagen reconstructions of the PCL, showed no significant difference for the detection of injury to the PCL compared to protocol 1 in overall sensitivity (42/50 [84%] vs. 44/50 [88%]), specificity (355/375 [95%] vs. 303/375 [81%]), PPV (42/62 [68%] vs. 44/116 [38%]), NPV (355/363 [98%] vs. 303/309 [98%]), accuracy (397/425 [93%] vs. 347/425 [82%]), and AUC (0.89 vs 0.84) (all comparisons, ΔAUC = 0.05, p = 0.20, Table 2). Inter-reader agreement was excellent for both protocols (κ = 0.87 for protocol 1 and κ = 0.90 for protocol 2), as well as between protocols (κ = 0.80). Notably, AUC increased significantly between protocol 1 and protocol 2 for complete PCL tears (0.80 vs 0.49, ΔAUC = 0.21, p = 0.02), but not for avulsions (ΔAUC = 0.01, p = 0.81, Table 2). Diagnostic accuracy parameters did not change significantly when arthroscopy was excluded as a reference standard. Agreement between MRI and protocol 2, including color-coded collagen reconstructions, was higher compared to agreement between MRI and protocol 1 for all injuries (Table 3). No partial PCL tears were observed in our study. An example case demonstrating improvement in the detection of PCL injury by color-coded collagen reconstruction is illustrated in Figs. 5 and 6.
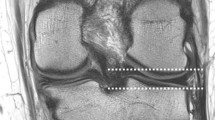
Standard unenhanced grayscale CT, color-coded collagen reconstructions, and unenhanced proton density-weighted MRI series with fat saturation of a 58-year-old patient show a tibial avulsion fracture of the posterior cruciate ligament (PCL) (A–C, arrows) following a dashboard injury. Color-coded collagen reconstructions and the MRI series demonstrate unambiguously a retained integrity of the thickened PCL (arrowheads), while there is some inhomogeneity of the PCL on standard grayscale CT series which led to a decreased readers’ diagnostic confidence when using protocol 1 compared to protocol 2 in this case. Abbreviations: PCL, posterior cruciate ligament
ROC curve analysis shows incremental value of protocol 2, including color-coded collagen reconstructions and grayscale CT (solid line) over protocol 1, comprising only standard grayscale CT (dotted line) for the depiction of all lesions (A, E), complete (B, F) and partial tears (C) of the cruciate ligaments. No incremental value was observed for avulsion fractures of the cruciate ligaments (D, G). Abbreviations: ROC, receiver-operating characteristic; ACL, anterior cruciate ligament; PCL, posterior cruciate ligament
Diagnostic accuracy between different reference standards
The prevalence of injury to the cruciate ligaments was significantly increased in patients that received arthroscopy. In line, diagnostic accuracy was significantly higher when arthroscopy was available as the reference standard compared to MRI as reference standard (p < 0.001) (Supplementary Table 2).
Diagnostic confidence, image quality, and image noise
The availability of color-coded collagen reconstructions increased the diagnostic confidence of all readers for the detection of injuries to the ACL (4.1 ± 0.6 vs. 2.7 ± 0.7, p < 0.001) and PCL (4.4 ± 0.7 vs. 3.0 ± 0.8, p < 0.001). Inter-reader agreement was moderate for protocol 1 (κ = 0.58 for ACL, κ = 0.52 for PCL) and good for protocol 2 (κ = 0.63 for ACL, κ = 0.65 for PCL). No significant differences were observed regarding the diagnostic confidence between less and more experienced readers (Table 4).
The image quality was rated with a mean score of 2.8 ± 0.7 for grayscale images and 4.0 ± 0.6 for color-coded collagen reconstructions, indicating that readers perceived image quality as superior in color-coded images (p < 0.001). Inter-reader agreement was comparable between grayscale and color-coded images (κ = 0.63 for grayscale, κ = 0.65 for color-coding).
Image noise was perceived lower in color-coded images compared to grayscale images (3.8 ± 0.7 vs. 2.4 ± 0.8, p < 0.001), and inter-reader agreement was similarly high (κ = 0.65 for grayscale, κ = 0.72 for color-coding).
Discussion
A novel third-generation dual-source DECT postprocessing algorithm based on dedicated material decomposition facilitates color-coded collagen reconstructions of the cruciate ligaments. Our results show that these provide substantially higher overall diagnostic accuracy for the evaluation of complete and partial tears of the ACL compared to standard grayscale CT (AUC 0.85 vs. 0.52 and 0.75 vs. 0.53, respectively, all comparisons p < 0.001), and that ligamentous integrity of the cruciate ligaments can be accurately assessed in avulsion fractures.
Previous research demonstrated insufficient soft tissue contrast of conventional multi-detector CT (MDCT) for the assessment of the cruciate ligaments [11]. For second-generation dual-source DECT grayscale images, Peltola et al and Glazebrook et al showed an increased sensitivity (79% and 86%, respectively) for the detection of complete ACL tears [19, 20]. There are, however, significant methodical shortcomings in both studies, with a highly selected study population comprising fewer than 30 participants per study (18 patients, Peltola et al; 27 patients, Glazebrook et al) and the exclusion of patients with partial tears of the cruciate ligaments. In addition, both studies used an insufficient reference standard obtained without control imaging or blinding of the control readings, and dedicated analysis of color-coded collagen reconstructions was omitted or did not demonstrate incremental diagnostic value over grayscale CT [19, 20]. Since then, multiple studies have demonstrated improved material decomposition of third-generation dual-source DECT over second-generation dual-source DECT, which can be attributed to improved spectral separation by extending the disparate tube voltages up to 90 kV and tin-filtrated Sn150 kV, improvements in iterative image reconstruction, and advances in detector technology. Ultimately, these allow for a more detailed color-coded depiction of ligaments and tendons, which has been difficult to achieve before [21,22,23,24,25,26,27]. However, no studies have yet evaluated the potential of third-generation dual-source DECT and collagen mapping to improve the assessment of the cruciate ligaments. In our study, the diagnostic accuracy for the detection of injury to the ACL using grayscale images was significantly lower compared to Peltola et al and Glazebrook et al with a sensitivity of 64%, possibly due to a more heterogenous study population that comprised patients with complete tears, partial tears, and avulsion fractures. Furthermore, a more precise classification of the lesions was required from readers in our study, which remains challenging even in MRI. Notably, the availability of color-coded collagen reconstructions derived from a novel postprocessing algorithm based on dedicated material decomposition significantly increased the sensitivity of readouts to 90%, despite the heterogeneity of our study population and the more complex requirements for lesion classification. We observed no increase in diagnostic accuracy using color-coded collagen reconstructions for the identification of avulsion fractures of the cruciate ligaments. This result was expected, as grayscale images in a dedicated bone kernel were included in both protocols. Nonetheless, color-coded reconstructions facilitate assessing the integrity of the cruciate ligaments in avulsion fractures, as demonstrated by increased diagnostic accuracy and confidence of reporting radiologists for protocol 2 over protocol 1. The incremental diagnostic value of CT-based assessment of the cruciate ligaments using color-coded collagen reconstructions and the high agreement between color-coded reconstructions and MRI highlight the potential of DECT as an alternative imaging approach for patients with contraindications to MRI and in circumstances where MRI is not available. Additional applications of third-generation dual-source DECT, such as the depiction of bone marrow edema to identify acute fractures, further emphasize this role [16, 22, 26]. Reconstruction of color-coded collagen images from dual-energy CT took 3 min on average and is therefore applicable in daily clinical practice. In contrast to MRI, CT scans are readily available during on-call times, which can accelerate the diagnosis and treatment of acute ACL tears. By reducing the time of immobilization and the risk of subsequent injury to other soft tissue structures of the knee, accelerated treatment can improve patient outcomes and reduce the socioeconomic burden on health care systems and working environments [5,6,7].
This retrospective study has certain limitations we would like to address. First, because patients with fractures or a high probability of damage to the internal structures of the knee did not routinely receive MRI before surgical inspection, we used a mixed reference standard comprising MRI and/or arthroscopic inspection. Nevertheless, MRI represents the current imaging gold standard for cruciate ligament assessment besides arthroscopy; thus, we decided to include each patient undergoing at least one of both reference standards. Interestingly, the diagnostic accuracy was significantly increased when arthroscopy was available as a reference standard. We believe that this is not a technical issue but rather attributable to the fact that the prevalence of ligamentous injury was significantly higher in patients where arthroscopy was performed, and that the sustained injuries of these patients were more severe and readily picked up in imaging. This is underlined by the fact that the use of MRI as a single reference standard did not lead to a reduction of diagnostic accuracy. Nonetheless, further studies with larger patient’s cohorts should be performed to gain more insights into this finding. Second, we evaluated the incremental diagnostic value of third-generation dual-source DECT-derived color-coded collagen reconstructions over third-generation dual-source DECT grayscale images. Due to improved material differentiation, soft-tissue contrast has also improved significantly for standard grayscale images. Therefore, the incremental diagnostic value of collagen reconstructions over single-energy CT or previous generations of dual-source DECT could be underestimated from the results of this study. Last, the color-coded collagen reconstruction algorithm used in our study is vendor-specific; and therefore, the results of our study cannot be generalized, although all major vendors offer dual-energy CT.
In conclusion, our study shows that third-generation dual-source DECT color-coded collagen reconstructions substantially improve diagnostic accuracy for the detection of acute complete and partial tears of the cruciate ligaments of the knee compared to standard grayscale images, with inexperienced readers benefiting the most. Color-coded reconstructions demonstrate good agreement with MRI and achieve superior diagnostic confidence, image quality, and noise scores compared to grayscale CT for all readers. Therefore, we believe this algorithm may become a viable alternative for assessing the cruciate ligaments when MRI is unavailable, but dual-energy CT can be performed.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- AUC:
-
Area under the curve
- DECT:
-
Dual-energy computed tomography
- FOV:
-
Field of view
- MDCT:
-
Multidetector computed tomography
- NPV:
-
Negative predictive value
- PCL:
-
Posterior cruciate ligament
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operator characteristic
- SD:
-
Standard deviation
References
Markolf KL, Mensch JS, Amstutz HC (1976) Stiffness and laxity of the knee–the contributions of the supporting structures. A quantitative in vitro study. J Bone Joint Surg Am 58:583–594
Gianotti SM, Marshall SW, Hume PA et al (2009) Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport 12:622–627. https://doi.org/10.1016/j.jsams.2008.07.005
Agel J, Rockwood T, Klossner D (2016) Collegiate ACL injury rates across 15 sports: National Collegiate Athletic Association Injury Surveillance System data update (2004–2005 Through 2012–2013). Clin J Sport Med 26:518–523. https://doi.org/10.1097/JSM.0000000000000290
Fanelli GC, Edson CJ (1995) Posterior cruciate ligament injuries in trauma patients: part II. Arthroscopy: J Arthrosc Relat Surg 11:526–529. https://doi.org/10.1016/0749-8063(95)90127-2
Sri-Ram K, Salmon LJ, Pinczewski LA et al (2013) The incidence of secondary pathology after anterior cruciate ligament rupture in 5086 patients requiring ligament reconstruction. Bone Joint J 95-B:59–64. https://doi.org/10.1302/0301-620X.95B1.29636
Prodromidis AD, Drosatou C, Thivaios GC et al (2021) Timing of anterior cruciate ligament reconstruction and relationship with meniscal tears: a systematic review and meta-analysis. Am J Sports Med 49:2551–2562. https://doi.org/10.1177/0363546520964486
Bergerson E, Persson K, Svantesson E et al (2022) Superior outcome of early ACL reconstruction versus initial non-reconstructive treatment with late crossover to surgery: a study from the Swedish National Knee Ligament Registry. Am J Sports Med 50:896–903. https://doi.org/10.1177/03635465211069995
Ajrawat P, Dwyer T, Whelan D et al (2021) A comparison of quadriceps tendon autograft with bone-patellar tendon-bone autograft and hamstring tendon autograft for primary anterior cruciate ligament reconstruction: a systematic review and quantitative synthesis. Clin J Sport Med 31:392–399. https://doi.org/10.1097/JSM.0000000000000765
Mather RC, Hettrich CM, Dunn WR et al (2014) Cost-effectiveness analysis of early reconstruction versus rehabilitation and delayed reconstruction for anterior cruciate ligament tears. Am J Sports Med 42:1583–1591. https://doi.org/10.1177/0363546514530866
Spindler KP, Wright RW (2008) Anterior cruciate ligament tear. N Engl J Med 359:2135–2142. https://doi.org/10.1056/NEJMcp0804745
Mustonen AOT, Koivikko MP, Haapamaki VV et al (2007) Multidetector computed tomography in acute knee injuries: assessment of cruciate ligaments with magnetic resonance imaging correlation. Acta Radiol 48:104–111. https://doi.org/10.1080/02841850601045138
Vetter JR, Perman WH, Kalender WA et al (1986) Evaluation of a prototype dual-energy computed tomographic apparatus. II. Determination of vertebral bone mineral content. Med Phys 13:340–343. https://doi.org/10.1118/1.595951
Wesarg S, Kirschner M, Becker M et al (2012) Dual-energy CT-based assessment of the trabecular bone in vertebrae. Methods Inf Med 51:398–405. https://doi.org/10.3414/ME11-02-0034
Booz C, Nöske J, Martin SS et al (2019) Virtual noncalcium dual-energy CT: detection of lumbar disk herniation in comparison with standard gray-scale CT. Radiology 290:446–455. https://doi.org/10.1148/radiol.2018181286
Gruenewald LD, Koch V, Martin SS et al (2021) Diagnostic accuracy of quantitative dual-energy CT-based volumetric bone mineral density assessment for the prediction of osteoporosis-associated fractures. Eur Radiol. https://doi.org/10.1007/s00330-021-08323-9
Booz C, Nöske J, Albrecht MH et al (2020) Diagnostic accuracy of color-coded virtual noncalcium dual-energy CT for the assessment of bone marrow edema in sacral insufficiency fracture in comparison to MRI. Eur J Radiol 129:109046. https://doi.org/10.1016/j.ejrad.2020.109046
Gruenewald LD, Leitner DH, Koch V et al (2023) Diagnostic value of DECT-based collagen mapping for assessing the distal tibiofibular syndesmosis in patients with acute trauma. Diagnostics 13:533. https://doi.org/10.3390/diagnostics13030533
Gruenewald LD, Koch V, Yel I et al (2022) Association of phantomless dual-energy CT-based volumetric bone mineral density with the prevalence of acute insufficiency fractures of the spine. Acad Radiol. https://doi.org/10.1016/j.acra.2022.11.020
Peltola EK, Koskinen SK (2015) Dual-energy computed tomography of cruciate ligament injuries in acute knee trauma. Skeletal Radiol 44:1295–1301. https://doi.org/10.1007/s00256-015-2173-x
Glazebrook KN, Brewerton LJ, Leng S et al (2014) Case–control study to estimate the performance of dual-energy computed tomography for anterior cruciate ligament tears in patients with history of knee trauma. Skeletal Radiol 43:297–305. https://doi.org/10.1007/s00256-013-1784-3
Booz C, Yel I, Martin SS et al (2021) Incremental diagnostic value of virtual noncalcium dual-energy computed tomography for the depiction of cervical disk herniation compared with standard gray-scale computed tomography. Invest Radiol 56:207–214. https://doi.org/10.1097/RLI.0000000000000734
Koch V, Müller FC, Gosvig K et al (2021) Incremental diagnostic value of color-coded virtual non-calcium dual-energy CT for the assessment of traumatic bone marrow edema of the scaphoid. Eur Radiol 31:4428–4437. https://doi.org/10.1007/s00330-020-07541-x
Johnson TRC, Krauß B, Sedlmair M et al (2007) Material differentiation by dual energy CT: initial experience. Eur Radiol 17:1510–1517. https://doi.org/10.1007/s00330-006-0517-6
Mallinson PI, Coupal TM, McLaughlin PD et al (2016) Dual-energy CT for the musculoskeletal system. Radiology 281:690–707. https://doi.org/10.1148/radiol.2016151109
Artzner C, Grozinger G, Kolb M et al (2022) Effect of acquisition techniques, latest kernels, and advanced monoenergetic post-processing for stent visualization with third-generation dual-source CT. Diagn Interv Radiol 28:364–369. https://doi.org/10.5152/dir.2022.21107
Booz C, Nöske J, Lenga L et al (2020) Color-coded virtual non-calcium dual-energy CT for the depiction of bone marrow edema in patients with acute knee trauma: a multireader diagnostic accuracy study. Eur Radiol 30:141–150. https://doi.org/10.1007/s00330-019-06304-7
Petritsch B, Kosmala A, Weng AM et al (2017) Vertebral compression fractures: third-generation dual-energy CT for detection of bone marrow edema at visual and quantitative analyses. Radiology 284:161–168. https://doi.org/10.1148/radiol.2017162165
Acknowledgements
We thank Neelam Lingwal for statistical advice and Karim Zayed for support in image retrieval.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Dr. Thomas J. Vogl.
Conflict of interest
Thomas J. Vogl is an Honorary Editor of European Radiology. They have not taken part in the review or selection process of this article.
I.Y. and C.B. received speaking fees from Siemens Healthineers. The other authors have no conflict of interest to disclose.
Statistics and biometry
Neelam Lingwal of the Institute for Biostatistics of the Goethe Universität Frankfurt kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
330_2023_9558_MOESM1_ESM.pdf
Supplementary file1 (PDF 209 kb) Supplementary Table 1 Individual readings of diagnostic accuracy for the ACL and PCL. Abbreviations: ACL: anterior cruciate ligament, PCL: posterior cruciate ligament, PPV: positive predictive value, NPV: negative predictive value, AUC: area under the curve. Numbers in square brackets are confidence intervals. Diagnostic accuracy of protocol 1 (standard grayscale CT) and protocol 2 (standard grayscale CT + color-coded collagen reconstructions) with MRI or arthroscopic inspection as the standard of reference. Supplementary Table 2 Diagnostic accuracy of color-coded collagen reconstructions for the ACL and PCL for arthroscopic inspection as reference standard. Abbreviations: ACL: anterior cruciate ligament, PCL: posterior cruciate ligament, PPV: positive predictive value, NPV: negative predictive value, AUC: area under the curve. Numbers in square brackets are confidence intervals. Diagnostic accuracy of protocol 2 (standard grayscale CT + color-coded collagen reconstructions) for arthroscopy as the reference standard. Prevalence of injury to the cruciate ligaments was higher in the group of patients with arthroscopic as the reference standard. Notably, for these patients the diagnostic accuracy was significantly increased compared to MRI, possibly due to more severe lesions that were easier to pick up in color-coded reconstructions.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gruenewald, L.D., Koch, V., Martin, S.S. et al. Diagnostic value of DECT-based colored collagen maps for the assessment of cruciate ligaments in patients with acute trauma. Eur Radiol 33, 6339–6350 (2023). https://doi.org/10.1007/s00330-023-09558-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09558-4