Abstract
Objectives
Coronary artery calcium (CAC) scores derived from computed tomography (CT) scans are used for cardiovascular risk stratification. Artificial intelligence (AI) can assist in CAC quantification and potentially reduce the time required for human analysis. This study aimed to develop and evaluate a fully automated model that identifies and quantifies CAC.
Methods
Fully convolutional neural networks for automated CAC scoring were developed and trained on 2439 cardiac CT scans and validated using 771 scans. The model was tested on an independent set of 1849 cardiac CT scans. Agatston CAC scores were further categorised into five risk categories (0, 1–10, 11–100, 101–400, and > 400). Automated scores were compared to the manual reference standard (level 3 expert readers).
Results
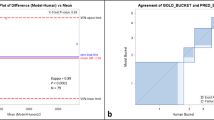
Of 1849 scans used for model testing (mean age 55.7 ± 10.5 years, 49% males), the automated model detected the presence of CAC in 867 (47%) scans compared with 815 (44%) by human readers (p = 0.09). CAC scores from the model correlated very strongly with the manual score (Spearman’s r = 0.90, 95% confidence interval [CI] 0.89–0.91, p < 0.001 and intraclass correlation coefficient = 0.98, 95% CI 0.98–0.99, p < 0.001). The model classified 1646 (89%) into the same risk category as human observers. The Bland–Altman analysis demonstrated little difference (1.69, 95% limits of agreement: −41.22, 44.60) and there was almost excellent agreement (Cohen’s κ = 0.90, 95% CI 0.88–0.91, p < 0.001). Model analysis time was 13.1 ± 3.2 s/scan.
Conclusions
This artificial intelligence–based fully automated CAC scoring model shows high accuracy and low analysis times. Its potential to optimise clinical workflow efficiency and patient outcomes requires evaluation.
Key Points
• Coronary artery calcium (CAC) scores are traditionally assessed using cardiac computed tomography and require manual input by human operators to identify calcified lesions.
• A novel artificial intelligence (AI)–based model for fully automated CAC scoring was developed and tested on an independent dataset of computed tomography scans, showing very high levels of correlation and agreement with manual measurements as a reference standard.
• AI has the potential to assist in the identification and quantification of CAC, thereby reducing the time required for human analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is a leading cause of death and disability worldwide, which imposes a substantial burden on healthcare expenditure [1]. Early identification of asymptomatic individuals at high cardiovascular risk is important for optimising the use of preventive pharmacotherapies, such as statins. The coronary artery calcium (CAC) score is a surrogate measure of atherosclerotic plaque burden within the coronary arteries that has been shown to predict CAD events [2, 3]. CAC is traditionally assessed non-invasively using electrocardiogram-gated computed tomography (CT) imaging of the heart, without the need for intravenous contrast [3]. Uptake in clinical practice is likely to increase, as guidelines now recommend CAC scoring for reclassifying cardiovascular risk in intermediate or borderline risk individuals, which thereby assists in decision-making around preventive therapies [4,5,6].
CAC is currently assessed manually by radiographers using CT image axial slices and then quantified using commercially available semi-automatic software. The radiographer must select high-density voxels, defined as > 130 Hounsfield units (HU), which are identified semi-automatically and then segmented according to their location in the coronary arteries.[3] Importantly, the radiographer must inspect the location of high-density voxels to exclude non-coronary calcification. CAC is usually quantified using the Agatston method, which considers calcified plaque area and maximal density of individual calcified lesions, but not location and distributional pattern [7, 8]. The Agatston score can be categorised into cardiovascular risk categories based on the score: 0 (no CAC), 1–10 (minimal CAC), 11–100 (mild CAC), 101–400 (moderate CAC), and > 400 (severe CAC) [3, 9]. CAC scoring, albeit straightforward, adds to costs and can be time-consuming and impractical for large-scale studies.
Automated models for CAC assessment using cardiac CT have been reported, including rule-based, machine learning, and deep learning approaches [10,11,12,13,14,15,16,17,18,19,20]. A challenge for fully automated scoring methods is the ability to discriminate between true CAC and calcification in surrounding structures, such as that of the mitral annulus, heart valves, and the aorta. Despite promising results, these automated methods have not yet been adopted into routine clinical practice as more evidence is necessary and generalisability needs to be demonstrated. Fully automated identification and quantification of CAC that requires very little or no human analysis can potentially decrease the workload of human operators, be more time-efficient, reduce costs, and play a role in large-scale screening strategies or epidemiological studies [21,22,23]. This study aims to develop and evaluate a novel artificial intelligence (AI)–based fully automated model that identifies and quantifies CAC using cardiac CT.
Material and methods
All CT scans used for training, validation, and testing of the automated CAC scoring model (DeepC Architecture, Salix, Artrya Ltd.) were retrospectively obtained. This study was approved by the local research ethics committee (Bellberry Human Research Ethics Committee: 2020-06-533) and was conducted in accordance with the Declaration of Helsinki.
Model development
A three-dimensional (3D) fully convolutional neural network (CNN) was developed to classify high-density voxels (defined as >130 HU) in the non-contrast CT volume as shown in Fig. 1. This custom CNN is a 13-layer model consisting of 3D convolution layers. The CNN field of view comprises an area of 33 mm in the z direction and 60.5 mm in the axial plane, which provides the spatial context the CNN uses to predict the classification of lesions identified. A separate U-NET-based CNN was developed to identify the ascending and descending aorta from the CT axial slices. The output of the aortic segmentation was used as an additional input channel to the CAC scoring CNN. A second two-dimensional CNN, with a similar design to the aortic segmentation model, was used to segment the cardiac area of interest from the scan. The use of these segmentation models was incorporated to reduce false positives by eliminating areas of the scan with non-coronary calcifications.
Architecture diagram for the automated CAC scoring algorithm. Abbreviations: CAC coronary artery calcium, CNN convolutional neural networks, CT computed tomography. Figure legend: As a pre-processing step, two-dimensional (2D) convolutional neural networks (CNN) are used to segment the ascending and descending aorta, and heart area. The 2D CNNs process the computed tomography (CT) scan slice by slice in the axial direction to generate a three-dimensional (3D) segmentation. The DeepC 3D CNN combines six input channels, each representing a 3D sub-volume. Of these six input channels, two are used for the aorta and heart segmentation, and a further three to provide spatial context relative to the centre of the scan in the x, y, and z directions. The final channel represents the Hounsfield unit (HU) subvolume. The extended input channels enable the CNN to classify specific HU patterns based on where they occur spatially in the scan. The 3D CNN then labels each coronary artery and an Agatston CAC score is calculated
A unique aspect of the model is the use of additional input channels to the CNN to provide spatial location information relative to a spatial reference point in the scan. As the CNN only has access to a subset of the CT volume when inferencing (i.e., the field of view as described previously), the additional spatial location data can be used to distinguish between similar spatial patterns occurring in different locations of the volume. This further assists in reducing false positives by differentiating coronary from non-coronary calcifications. For example, calcifications of the left anterior descending artery only occur near the anterior interventricular groove and the CNN leverages the information embedded in the spatial channels to incorporate this into the analysis. An ADAMAX optimiser was used along with a cross-entropy loss function against the categorical vessel classes.
Validation and testing
Non-contrast prospective electrocardiogram-gated CT scan data from individuals aged ≥ 18 years who underwent assessment of CAC for investigation of CAD, where an Agatston CAC score was reported by level 3 expert readers, was included. Manual CAC scores were considered as ground truth. Scans were assessed for exclusion criteria a priori by the study investigators, and excluded scans were not included in the analyses. Exclusion criteria included high levels of noise, presence of multiple non-contrast series, missing data, and scans in individuals with coronary artery stents, coronary artery bypass grafts, prosthetic heart valves, permanent cardiac pacemakers, or other metal artefacts. In the dataset, multiple non-contrast CT series in an individual may have been present in cases where there was noise or acquisition issues. As such, these scans were excluded to reduce the potential for bias. The level of noise was determined by the signal-to-noise ratio in the descending aorta and the number of lesions (> 130 HU). The cut-off for excluding a scan due to noise was defined a priori through internal analyses as a signal-to-noise ratio of 1.7 with a maximum lesion number of 9000, such that no more than 5% of scans would be excluded.
For training and validation of the automated model, consecutive non-contrast-enhanced cardiac CT scans that were performed routinely for clinical purposes were retrospectively obtained from two separate institutions. The 3D CNN was trained on (1) 2251 Siemens Healthcare SOMATOM Force scans acquired from Envision Medical Imaging (Perth, Australia), with a validation set consisting of 735 scans that were randomly selected; and (2) 143 Philips Healthcare Brilliance 64 and 45 Toshiba Medical Systems Aquilion ONE scans acquired from University of Edinburgh (Edinburgh, Scotland), with a validation set consisting of 20 Philips Healthcare and 16 Toshiba Medical Systems scans.
The aorta model was trained using data from three separate CT scanners: Siemens Healthcare SOMATOM Force, Toshiba Medical Systems Aquilion ONE, and Philips Healthcare Brilliance 64. In total, 54 studies were used in the training set with seven studies in the validation set and 12 studies in the test set, all of which were randomly selected. A Dice score of 0.94 was achieved on the test set. A larger training set was used to develop the heart model with 94 studies in the training set across the three scanners, seven studies in the validation set, and 10 studies in the test set. The Dice score for the heart model was 0.86.
Following this, 2000 cardiac CT scans performed for clinical indications between December 2014 and May 2021 at the University of Ottawa Heart Institute (Ottawa, Canada) were retrospectively obtained. These CT images were acquired with standardised vendor-specific sequential scanning protocols, a tube voltage of 120 kVp and slice thickness of 2.5 mm (GE Healthcare) or 3 mm (Siemens Healthcare). After applying exclusion criteria, the automated CAC scoring model was tested on this independent dataset using images from the non-contrast series and CAC scores were computed for each scan. The graphic processing unit used was EVGA GeForce RTX3090 FTW3 ULTRA 24G (NVIDIA).
Statistical analysis
Statistical analyses were performed using Python (Python Software Foundation). Data are presented as mean and standard deviation or count and percent. The total CAC score per individual was computed using the Agatston method and was further categorised according to the following five cardiovascular risk categories based on the score: 0, 1–10, 11–100, 101–400, and > 400.[3, 9] Automated CAC scores were compared to the manual and prospectively derived Agatston CAC scores as per the scan report (manual reference standard). Differences between proportions were compared using Pearson’s chi-square test. Correlation and agreement between methods were assessed using Spearman’s rank correlation coefficient (⍴), two-way intraclass correlation coefficient (ICC), Bland-Altman plots with mean difference and 95% limits of agreement, and Cohen’s linearly weighted kappa coefficient (κ). A two-tailed p value of < 0.05 was used to define statistical significance.
Results
Of the 2000 independent cardiac CT scans obtained, 151 were excluded and the remaining 1849 (92.5%) were used for testing the model as shown in Fig. 2. Of these 1849 scans, 965 (52.2%) were Siemens Healthcare Definition Flash and 884 (47.8%) were GE Healthcare Lightspeed VCT 64 slice scans. The mean age was 55.7 ± 10.5 years and 915 (49.5%) were males. The mean total analysis time per scan was 13.1 ± 3.2 s for the model, with variations in time due to the number of slices per CT scan required to analyse.
Coronary artery calcifications were reported in 815 (44.1%) individuals with the reference standard and in 867 (46.9%, p = 0.09) individuals using the automated model. Examples of calcifications detected are shown in Fig. 3. Of the 1034 (55.9%) individuals with a zero CAC score with the reference standard, 92 (8.9%) had a positive score using the automated model (Table 1) and the reasons for this are detailed in Supplemental Table 1. Of the 815 (44.1%) individuals with a positive CAC score with the reference standard, 40 (4.9%) had a score of zero using the automated model (reasons detailed in Supplemental Table 1). A CAC score of > 100 Agatston units was reported in 274 (14.8%) individuals with the reference standard, of which 256 (93.4%) had a score of > 100 using the automated model. For CAC score > 100, the positive predictive value was 95.2% and negative predictive value was 98.9%. Of the 1575 (85.2%) individuals with a CAC score ≤ 100 Agatston units, 13 (0.8%) had a score > 100 using the automated model.
Example cases of calcifications detected. Figure legend: Successful detection of coronary artery calcification is seen in the (A) left main coronary artery, (B) left anterior descending coronary artery, (C) left circumflex coronary artery, and (D) right coronary artery. Successful detection of calcification that would not contribute to the calcium score is seen in the (E) aortic root and (F) mitral annulus.
The CAC score results from the automated model correlated very strongly (Spearman’s r = 0.90, 95% confidence interval [CI] 0.89–0.91, p < 0.001; and ICC = 0.98, 95% CI 0.98–0.99, p < 0.001) with the reference standard (Fig. 4). Bland–Altman analysis showed little difference in CAC scores between the reference standard and those predicted by the automated model, with a mean difference of 1.69 (95% limits of agreement: −41.22, 44.60) (Fig. 5). Overall, the fully automated model classified 1646 individuals (89.0%) into the same CAC score risk category as a reference standard. Of the 203 individuals that were reclassified, 171 (84.2%) were reclassified to the next risk category. When CAC score risk categories between the two methods were compared using Cohen’s kappa statistic (Table 1), there was almost excellent agreement (κ = 0.90, 95% CI 0.88–0.91, p < 0.001).
Discussion
This paper presents a novel AI-based fully automated model that was developed to identify and quantify total per-patient CAC using non-contrast electrocardiogram-gated cardiac CT. The model demonstrated very high levels of correlation and agreement when compared with CAC scores obtained with the manual reference standard. Notably, the high accuracy of the model was maintained across the spectrum of cardiovascular risk categorisation and across different scanners. In addition, the model was able to compute the CAC score quickly, with a low analysis time per CT scan. These results lay the foundation for the translation of AI-based CAC scoring techniques in clinical practice.
The number of studies evaluating automated CAC scoring models is limited and comparison of studies is difficult due to differences in study design, methods, and CT datasets used. The present study is an extension of other similar studies with results that are in line with that of other cardiac CT studies evaluating automated methods, with high correlation and kappa coefficients of approximately 0.90 when compared to a human reference standard [12, 15, 16, 18,19,20]. Automated CAC scoring has also been the subject of notable publications over the past two years, including another multi-centre and multi-vendor study by Eng et al which included non-electrocardiogram gated CT scans [21, 23, 24]. AI models can also have a role in identifying and quantifying CAC in low-dose non-electrocardiogram-gated CT scans that include the heart, but which are performed for non-cardiac reasons such as lung cancer screening, thereby allowing opportunistic cardiovascular risk assessment [15, 16, 23,24,25]. However, given the reduced fidelity of non-gated chest CT, automated CAC score accuracies remain low (kappa coefficient in the range of 0.6 to 0.7) [20, 25].
A major challenge for automated CAC scoring methods is the ability to discriminate between true CAC and non-coronary calcification or noise without the need for human input. Some automated algorithms reported in the literature have relied on information from coronary computed tomography angiography (CCTA) slices to better define coronary artery anatomy, and therefore improve this discrimination [13, 26, 27]. However, CT images for quantifying CAC are not always acquired in conjunction with CCTA, which requires intravenous contrast. The focus of the present study is to achieve fast and accurate results exclusively on non-contrast electrocardiogram-gated cardiac CT scans. With this in mind, the present study developed an AI-based model using multiple CNNs designed to integrate 3D spatial location information, such that the position of the coronary arteries and aorta can be estimated, and lesions can be segmented without the need for contrast. The incorporation of a separate aortic segmentation model and a cardiac segmentation model may also help to reduce false positives by differentiating coronary from non-coronary calcifications. The model was also able to compute a CAC score in the order of seconds, which is substantially faster than manual methods and is an important prerequisite for implementing AI software [15, 17, 18, 20].
Another difference in the present study design is the use of five categories for the CAC score [3, 9]. Some studies using cardiac CT have assessed the ability of automated models to differentiate individuals into three or four CAC score risk categories [10, 19, 21, 26]. The inclusion of categories for CAC scores of 1–10 and 11–100 rather than one category for 1–100 assesses the added ability to identify individuals with minimal coronary artery plaque. Furthermore, individuals with a CAC score of zero have a very low 10-year cardiovascular risk and identifying these individuals can reduce the use of unnecessary preventative pharmacotherapies. [9] The automated model classified 9% of individuals with a reported CAC score of zero as having a positive score, and the reasons for this included detection of non-coronary calcification, noise, ground truth in question, and artefacts. On the other hand, only 5% of individuals with a reported positive CAC score were classified as having a score of zero using the automated model for similar reasons as above. Similar reasons have also been noted in previous AI studies in CAC scoring, thus highlighting an ongoing challenge [12, 28]. The majority of miscategorisation was between the 0 and 1–10 CAC score categories. From a clinical perspective, there are currently no recommendations for the use of a CAC score between 1 and 10 Agatston units to guide decision-making around preventive pharmacotherapies and thus the clinical impact of miscategorisation at this very low range of CAC score is reduced.
Although the CAC score is a continuous variable, guidelines recommend a CAC score of ≥ 100 Agatston units as a threshold for initiating statins [4,5,6]. The automated model accurately identified a CAC score >100 Agatston units in 95% of individuals compared with manual human assessment. On the other hand, < 1% of individuals with a CAC score ≤ 100 Agatston units had a score > 100 using the automated model. Although the model achieved respectable diagnostic performance, visual feedback can be provided to display regions contributing to the score and allow human operators to make modifications if required. Although not utilised in the present study, ambiguity detectors can be embedded to prompt feedback by human operators in cases of lesion uncertainty, which can resolve false positive or negative results and thus minimise the misclassification of CAC score categories [10, 12].
The use of AI in cardiovascular imaging has developed rapidly over the past decade [22, 23]. Fully automated models can minimise the physical and repetitive task of performing CAC identification, quantitation, and segmentation by reducing the need for human analysis. Re-direction of the human operator’s role to other tasks instead can further reduce costs associated with CAC scoring, thus making it more widely available. This is important as demand for CAC scoring is likely to increase substantially in the future due to guidelines now recommending its use as an additional non-invasive tool for cardiovascular risk-stratification [4,5,6]. Furthermore, automated models can be applied to large populations for screening or research purposes due to their ability to quantify CAC in seconds and because AI can potentially overcome measurement errors by human observers due to its high repeatability [21, 23]. Once fully validated, AI models for CAC scoring could also be used to train physicians in interpreting and reporting CAC scores.
The large number of CT scans used for training, validation, and testing of the automated CAC scoring model is a key strength of the present study. In addition, CT images in the dataset were acquired from several different scanners, reflecting the variability of real-world practice. Although CT scanners made by different vendors might produce different CAC scores, testing the automated model on a variety of CT images from different vendors or scanner types improves its applicability and generalisability to different practices [29]. A limitation of this study is that over half of the scans in the testing dataset had a zero CAC score. Although this is consistent with other studies and reflects the clinical practice and real-world populations, such a dataset would result in some cases where the model incorrectly reports a positive CAC score (particularly in the 1–10 CAC score category) [17]. Thus, the reported results could have been even better if not for this limitation. The accuracy of the model may therefore be reduced at very low levels of CAC and future iterations of the model will seek to refine this aspect. Furthermore, the model was not developed to quantify CAC per individual coronary artery, which may improve cardiovascular risk-stratification, but is not yet routinely performed for this purpose [8]. Scans with metal artefacts and high levels of noise were excluded as this can influence the CAC score, thus limiting the applicability of the automated model to such cases.
In conclusion, the presented fully automated AI-based CAC scoring model for cardiac CT is novel and rapid and shows high accuracy when compared to current manual CAC scoring methods. Future studies should evaluate its potential impact on clinical practice and workflow for cardiac CT reporting clinicians, as well as evaluate the association between automated CAC scores and patient outcomes.
Abbreviations
- AI :
-
Artificial intelligence
- CAC :
-
Coronary artery calcium
- CAD :
-
Coronary artery disease
- CCTA :
-
Coronary computed tomography angiography
- CNN :
-
Convolutional neural network
- CT:
-
Computed tomography
- HU :
-
Hounsfield units
- ICC :
-
Intraclass correlation coefficient
References
Khan MA, Hashim MJ, Mustafa H et al (2020) Global epidemiology of ischemic heart disease: results from the global burden of disease study. Cureus 12:e9349
McClelland RL, Jorgensen NW, Budoff M et al (2015) 10-year coronary heart disease risk prediction using coronary artery calcium and traditional risk factors: derivation in the MESA (Multi-Ethnic Study of Atherosclerosis) with validation in the HNR (Heinz Nixdorf Recall) study and the DHS (Dallas Heart Study). J Am Coll Cardiol 66:1643–1653
Hecht HS (2015) Coronary artery calcium scanning: past, present, and future. JACC Cardiovasc Imaging 8:579–596
Visseren FLJ, Mach F, Smulders YM et al (2021) 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 42:3227–3337
Arnett DK, Blumenthal RS, Albert MA et al (2019) 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140:e596–e646
Jennings GL, Audehm R, Bishop W et al (2021) National Heart Foundation of Australia: position statement on coronary artery calcium scoring for the primary prevention of cardiovascular disease in Australia. Med J Aust 214:434–439
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
Blaha MJ, Budoff MJ, Tota-Maharaj R et al (2016) Improving the CAC score by addition of regional measures of calcium distribution: multi-ethnic study of atherosclerosis. JACC Cardiovasc Imaging 9:1407–1416
Budoff MJ, Shaw LJ, Liu ST et al (2007) Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol 49:1860–1870
Isgum I, Rutten A, Prokop M, van Ginneken B (2007) Detection of coronary calcifications from computed tomography scans for automated risk assessment of coronary artery disease. Med Phys 34:1450–1461
Shahzad R, van Walsum T, Schaap M et al (2013) Vessel specific coronary artery calcium scoring: an automatic system. Acad Radiol 20:1–9
Wolterink JM, Leiner T, Takx RA, Viergever MA, Isgum I (2015) Automatic coronary calcium scoring in non-contrast-enhanced ECG-triggered cardiac CT with ambiguity detection. IEEE Trans Med Imaging 34:1867–1878
Yang G, Chen Y, Ning X, Sun Q, Shu H, Coatrieux JL (2016) Automatic coronary calcium scoring using noncontrast and contrast CT images. Med Phys 43:2174
Wolterink JM, Leiner T, de Vos BD, van Hamersvelt RW, Viergever MA, Išgum I (2016) Automatic coronary artery calcium scoring in cardiac CT angiography using paired convolutional neural networks. Med Image Anal 34:123–136
de Vos BD, Wolterink JM, Leiner T, de Jong PA, Lessmann N, Isgum I (2019) Direct automatic coronary calcium scoring in cardiac and chest CT. IEEE Trans Med Imaging 38:2127–2138
van Velzen SGM, Lessmann N, Velthuis BK et al (2020) Deep learning for automatic calcium scoring in CT: validation using multiple cardiac CT and chest CT protocols. Radiology 295:66–79
Martin SS, van Assen M, Rapaka S et al (2020) Evaluation of a deep learning-based automated CT coronary artery calcium scoring algorithm. JACC Cardiovasc Imaging 13:524–526
Sandstedt M, Henriksson L, Janzon M et al (2020) Evaluation of an AI-based, automatic coronary artery calcium scoring software. Eur Radiol 30:1671–1678
Wang W, Wang H, Chen Q et al (2020) Coronary artery calcium score quantification using a deep-learning algorithm. Clin Radiol 75:237.e211-237.e216
Eng D, Chute C, Khandwala N et al (2021) Automated coronary calcium scoring using deep learning with multicenter external validation. NPJ Digit Med 4:88
Vonder M, Zheng S, Dorrius MD et al (2022) Deep learning for automatic calcium scoring in population-based cardiovascular screening. JACC Cardiovasc Imaging 15:366–367
Dey D, Slomka PJ, Leeson P et al (2019) Artificial intelligence in cardiovascular imaging: JACC state-of-the-art review. J Am Coll Cardiol 73:1317–1335
Lee H, Martin S, Burt JR et al (2020) Machine learning and coronary artery calcium scoring. Curr Cardiol Rep 22:90
Xu J, Liu J, Guo N et al (2021) Performance of artificial intelligence-based coronary artery calcium scoring in non-gated chest CT. Eur J Radiol 145:110034
Zeleznik R, Foldyna B, Eslami P et al (2021) Deep convolutional neural networks to predict cardiovascular risk from computed tomography. Nat Commun 12:715
Wolterink JM, Leiner T, de Vos BD et al (2016) An evaluation of automatic coronary artery calcium scoring methods with cardiac CT using the orCaScore framework. Med Phys 43:2361
Eilot D, Goldenberg R (2014) Fully automatic model-based calcium segmentation and scoring in coronary CT angiography. Int J Comput Assist Radiol Surg 9:595–608
Lessmann N, van Ginneken B, Zreik M et al (2018) Automatic calcium scoring in low-dose chest CT using deep neural networks with dilated convolutions. IEEE Trans Med Imaging 37:615–625
Willemink MJ, Vliegenthart R, Takx RA et al (2014) Coronary artery calcification scoring with state-of-the-art CT scanners from different vendors has substantial effect on risk classification. Radiology 273:695–702
Funding
Open Access funding enabled and organised by CAUL and its Member Institutions. MCW (FS/ICRF/20/26002) is supported by the British Heart Foundation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof Girish Dwivedi.
Conflict of interest
The authors of this manuscript declare the following conflicts of interest:
The methods for the analysis of automated calcium scoring described in this report are subject to patent application (WO2021168517A1) (JF, JJ, GD, AI)
GD, ARI, JF, JJ – Equity; Artrya Ltd.
JF, SW, JJ – Employees of Artrya Ltd.
MCW - Speaker bureau for Canon Medical Systems.
GD – Speaker bureau for Janssen, Amgen, Pfizer, AstraZeneca
ARI – Speaker bureau from Boston Scientific, Abbott Medical, Janssen
Statistics and biometry
One of the authors has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained by the Bellberry Limited 2020-06-533.
Methodology
• Retrospective
• Observational
• Multicentre
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 21 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ihdayhid, A.R., Lan, N.S.R., Williams, M. et al. Evaluation of an artificial intelligence coronary artery calcium scoring model from computed tomography. Eur Radiol 33, 321–329 (2023). https://doi.org/10.1007/s00330-022-09028-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09028-3