Abstract
Objectives
Different machine learning algorithms (MLAs) for automated segmentation of gliomas have been reported in the literature. Automated segmentation of different tumor characteristics can be of added value for the diagnostic work-up and treatment planning. The purpose of this study was to provide an overview and meta-analysis of different MLA methods.
Methods
A systematic literature review and meta-analysis was performed on the eligible studies describing the segmentation of gliomas. Meta-analysis of the performance was conducted on the reported dice similarity coefficient (DSC) score of both the aggregated results as two subgroups (i.e., high-grade and low-grade gliomas). This study was registered in PROSPERO prior to initiation (CRD42020191033).
Results
After the literature search (n = 734), 42 studies were included in the systematic literature review. Ten studies were eligible for inclusion in the meta-analysis. Overall, the MLAs from the included studies showed an overall DSC score of 0.84 (95% CI: 0.82–0.86). In addition, a DSC score of 0.83 (95% CI: 0.80–0.87) and 0.82 (95% CI: 0.78–0.87) was observed for the automated glioma segmentation of the high-grade and low-grade gliomas, respectively. However, heterogeneity was considerably high between included studies, and publication bias was observed.
Conclusion
MLAs facilitating automated segmentation of gliomas show good accuracy, which is promising for future implementation in neuroradiology. However, before actual implementation, a few hurdles are yet to be overcome. It is crucial that quality guidelines are followed when reporting on MLAs, which includes validation on an external test set.
Key Points
• MLAs from the included studies showed an overall DSC score of 0.84 (95% CI: 0.82–0.86), indicating a good performance.
• MLA performance was comparable when comparing the segmentation results of the high-grade gliomas and the low-grade gliomas.
• For future studies using MLAs, it is crucial that quality guidelines are followed when reporting on MLAs, which includes validation on an external test set.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
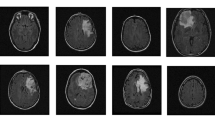
Gliomas are the most frequently occurring primary tumor of the brain [1]. Accurate segmentation of gliomas on clinical magnetic resonance imaging (MRI) scans plays an important role in the quantification and objectivation of diagnosis, treatment decision, and prognosis [2,3,4]. In current clinical practice, T1-weighted, post-contrast T1-weighted, T2-weighted, and T2-fluid attenuated inversion recovery (FLAIR) sequences are required to characterize the different components and to assess the infiltration of the surrounding brain parenchyma [5, 6]. Glioma segmentation requires the distinguishing of tumor tissue from healthy surrounding tissues by the radiologist [7] and the segmented region of interest or volume of interest can be used to compute feature-based radiomics and quantifiable measurements [8, 9]. However, segmentation is a time-consuming task with high inter-observer variability [10, 11]. Therefore, automatic segmentation methods have been searched for as these could facilitate consistent measures and simultaneously could reduce time spent on the task by radiologists in their daily practice. These developments have been powered by the organization of the annual multimodal Brain Tumor Segmentation (BraTS) challenge (http://braintumorsegmentation.org/). Within the BraTS challenges, the organization committee released multimodal scan volumes of a relatively large number of patients suffering from glioma after which different research groups aim to construct machine learning algorithms (MLAs) to automatically segment the gliomas. The BraTS data were accompanied by corresponding segmentations which served as the ground truth [11]. Recent developments in automatic segmentation by the use of MLAs helped to achieve higher precision [12]. Within the BraTS challenges, the MLAs which yielded the most accurate results included different 2D and 3D convolutional neural networks (CNNs) [13,14,15,16,17], including 3D U-Nets [18, 19].
Despite the large body of scientific literature covering this topic, a comprehensive overview and meta-analysis of the accuracy of MLAs in glioma segmentation is still lacking [20, 21]. Therefore, factors which enable the further development of MLAs for glioma segmentation remain partially elusive. The aim of the current study therefore was to provide a systematic review and meta-analysis of the accuracy of MLA-based glioma segmentation tools on multimodal MRI volumes. By providing this overview, the strengths and limitations of this field of research were highlighted and recommendations for future research were made.
Methods
The systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [22]. Prior to initiation of the research, the study protocol was registered in the international open-access Prospective Register of Systematic Reviews (PROSPERO) under number CRD42020191033.
Papers that developed or validated MLAs for the segmentation of gliomas were reviewed. Literature was searched for in MEDLINE (accessed through PubMed), Embase, and The Cochrane Library, between April 1, 2020, and June 19, 2020. No language restrictions were applied. The full search strings, including keywords and restrictions, are available in the Appendix. Studies describing MLA-based segmentation methodologies on MR images in glioma patients were included. Additional predefined inclusion criteria were as follows: (1) mean results were defined as dice similarity coefficient (DSC) score; (2) study results needed to be validated either internally and/or externally. Letters, preprints, scientific reports, and narrative reviews were included. Studies based on animals or non-human samples or that presented non-original data were excluded.
Two researchers screened the papers on title, abstract, and full-text independently. Discussions between both researchers were held to resolve all disagreements about non-consensus papers. The investigators independently extracted valuable data of the included papers using a predefined data extraction sheet after which the data was cross-checked. Data extracted from the included studies comprised the following: (a) first author and year of publication; (b) size of training set; (c) mean age of participants in the training set; (d) gender of participants in the training set; (e) size of internal test set; (f) whether there was an external validation; (g) study design, including the used MRI sequences and the segmentations which formed the ground truth; (h) architecture of the AI-algorithm(s); (i) target condition; (j) performance of the algorithm(s) in terms of DSC score, sensitivity, and specificity for both the training and the internal and/or external test sets. When studies performed external validation of the described AI-system(s), externally validated data were included in data extraction tables. Data from the internal validation were used when studies solely carried out the internal validation of the reported MLAs.
The quality of the included studies was not formally assessed, as a formal quality assessment is a well-known challenge in this area of research [23,24,25]. Nevertheless, Collins and Moons (2019) announced their initiative to develop a version of the transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) statement tailored to machine learning methods [26]. Pinto dos Santos suggested on the European Society of Radiology website various items to take into consideration when reviewing literature regarding machine learning [27]. These items were included in this review.
Statistical assessment
An independent statistician was consulted to discuss the statistical analyses and approaches with regard to the meta-analysis. To estimate the overall accuracy of the current MLAs, a random effects model meta-analysis was conducted. To be included in the meta-analysis, studies needed to have reported the outcome of interest (i.e., DSC score), in combination with a standard deviation (SD), standard error (SE), and/or the 95% confidence interval (95% CI). For studies reporting the SE and/or the 95% CI, the SD was statistically assessed [28]. Meta-analysis was performed on aggregated data of all studies providing suitable outcomes. Then, subgroup analyses were conducted on two separate target conditions, for studies describing the segmentation of either HGGs or LGGs.
Statistical analyses were carried out by use of IBM SPSS Statistics (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. IBM Corp.). Variables and outcomes of the statistical assessment were presented as mean with ± SD when normally distributed. When data were not normally distributed, they were presented as the median with range (minimum–maximum). Statistical tests were two-sided and significance was assumed when p < 0.05.
The DSC score represents an overlap index and is the most used metric in validating segmentation images. In addition to the direct comparison between automated and ground truth segmentations, the DSC score is a common measure of reproducibility [29, 30]. The DSC score ranges from 0.0 (no overlap) to 1.0 (complete overlap). In this meta-analysis, a DSC score of ≥ 0.8 was considered good overlap. A DSC score of ≤ 0.5 was considered poor.
The quantitative meta-analysis was partially carried out using OpenMeta[Analyst] software, which is the visual front-end for the R package (www.r-project.org; Metafor) [31]. Forest plots were created to depict the estimated DSC scores from the included studies, along with the overall DSC score performance. When the 95% CI of the different subgroup analyses overlapped, no further statistical analysis was carried out.
The heterogeneity of the included studies was tested with the Higgins I2-test. The Higgins I2-test quantifies inconsistency between included studies, where a value > 75% indicates considerable heterogeneity between groups. A low heterogeneity corresponds with a Higgins I2 between 0 and 40% [28]. Both the meta-analyses of the aggregated groups as the meta-analyses of the subgroups were performed using a random effects model, due to an observed high heterogeneity (Higgins I2 > 75%) between included studies [32].
To showcase possible publication bias, a funnel plot was created by means of Stata (StataCorp. 2019. Stata Statistical Software: Release 16.: StataCorp LLC.).
Results
Initially, 1094 publications were retrieved through database searching. An additional ten publications were identified through cross-referencing. After removing duplicates, the remaining 734 publications were screened. Based on the title and abstract, 509 papers were excluded. A total of 225 full-text articles were assessed for eligibility and 42 studies were included in the systematic review. Ten studies were eligible for inclusion for the meta-analysis as they provided sufficient quantitative data (e.g., only these studies provided the DSC score along with SD for the performance of the MLA) (Fig. 1). Publications describing the use of (automated) segmentations to apply MLAs to classify molecular characteristics of gliomas (n = 135) were excluded. Fourteen papers were excluded as they described the use of MLAs on gliomas to perform texture analyses. Eleven papers did not report the DSC score and another 11 studies showed unclarities in data reporting. Contacting the authors of these papers did not result in the acquisition of the needed data. Five studies did not report results of internal or external validation steps, whereas an additional three studies did not report data from the training-group. Three studies described separate combined features, instead of a coherent MLA methodology. One study was excluded due to the inclusion of other brain tumors next to gliomas (e.g., metastases) (Fig. 1).
Review of the included studies
Based on the full-text analysis, 42 segmentation studies [13, 17, 33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72] were included for the systematic review, from which the participant demographics and study characteristics are depicted in Table 1. The used MLAs are presented in Table 1 and comprised different types of CNNs [13, 17, 34, 35, 37,38,39,40,41,42,43, 45,46,47, 49,50,51,52,53, 55,56,57, 60, 61, 63,64,65, 67] and random forest model [68,69,70], multiple classifier system [33, 44], and an adaptive superpixel generation algorithm [60]. In addition, one study used semi-automatic constrained Markov random field pixel labeling [64], one study used an end-to-end adversarial neural network [71], and one study used a 3D supervoxel-based learning method [56].
Thirty-eight studies combined different combinations of MRI sequences for brain tumor segmentation (Table 1) [13, 17, 33,34,35,36,37,38,39,40,41,42, 44, 45, 47,48,49,50,51,52,53,54,55,56,57, 59,60,61,62,63,64,65,66,67,68,69,70,71,72]. Only 3 studies used one MRI sequence for the algorithm to segment [43, 46, 58]. One conference paper did not report on the used MRI sequences [56]. Four studies reported not to have used (any part of) the BraTS datasets [36, 46, 50, 51]. Two of these papers used original data [46, 51]. The other two papers used either data from the Cancer Imaging Archive (TCIA) [50] or a combination of TCIA data and original data [36].
In 36 studies, the ground truth (i.e., segmentations) was derived from the BraTS dataset [13, 17, 33,34,35,36, 38,39,40,41,42,43,44,45, 47,48,49, 52,53,54,55, 57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. In two of these studies, the researchers added segmentations of additional original data. Segmentations were manually annotated by two experienced professionals independently following the BraTS segmentation protocol[54, 64]. In one paper, only original data with corresponding segmentations were used. These segmentations were made independently by two experienced professionals following the BraTS segmentation protocol [51]. Three papers used segmentations which were obtained without adhering to the BraTS segmentation protocol [36, 46, 50]. In one conference paper, the segmentation methodology was not described [56]. Please note that the ground truth segmentations of BraTS 2015 were first produced by algorithms and then verified by annotators, whereas the ground truth of BraTS 2013 fused multiple manual annotations.
The performance of the MLAs, in terms of sensitivity, specificity, and DSC score, is displayed in Table 1. All studies used retrospectively collected data. Nine studies focused specifically on the segmentation of HGGs, whereas seven studies focused on the segmentation of LGGs. The remaining studies (n = 31) described the segmentation of gliomas in general without the subdivision of LGG and HGG. Five of the included studies [33, 35, 38, 62, 65] described segmentation of multiple target conditions (i.e., segmentation of both HGG and LGG). For these studies, the results of each different target are displayed in Table 1 as well. All of the included studies conducted some version of cross-validation on the MLAs; however, only four studies [35, 36, 51, 64] performed an external validation of performance.
Nine studies [33, 35, 36, 38, 51, 62, 64, 65, 72] described the segmentation of HGGs in particular, with four studies [35, 36, 51, 64] externally validating the performance of the reported MLAs. Performance evaluation of the included studies in terms of the validated DSC score ranged from 0.78 to 0.90. MLA sensitivity ranged from 84 to 85% (n = 3) [33, 51, 64]. Only one study [33] presented the specificity rate (i.e., 98%).
Seven studies [33, 35, 38, 46, 50, 62, 65] described the segmentation of LGGs. External validation of the MLA was performed by one study [35]. The validated DSC score for the included studies ranged from 0.68 to 0.85. Sensitivity was 89% (n = 2) [33, 46], whereas specificity was 98% (n = 1) [33].
Meta-analysis of the included studies
The aggregated meta-analysis comprised twelve MLAs, described in ten individual studies [33, 36, 44, 47, 51, 54, 58, 62, 66, 72], and showed an overall DSC score of 0.84 (95% CI: 0.82 – 0.86) (Fig. 2). Heterogeneity showed to be 80.4%, indicating that studies differed significantly (p < 0.001).
Forest plot of the included studies that assessed the accuracy of segmentation of glioma. Legend: DSC, dice similarity coefficient; CI, confidence interval. Forest plot shows that the performance of the MLAs to segment gliomas are centered around a DSC of 0.837 with a 95% CI ranging from 0.820 to 0.855
For the subgroup analysis of segmentation studies focusing on HGGs, the results are depicted in Fig. 3. Overall, DSC score for the five included studies [33, 36, 51, 62, 72] was 0.83 (95% CI: 0.80 – 0.87). The estimated I2 heterogeneity between groups showed to be 81.9% (p = 0.001). Two studies [33, 62] focusing on the segmentation of LGGs were included in another subgroup meta-analysis. Overall, the DSC score was found to be 0.82 (95% CI: 0.78–0.87) (Fig. 4). The estimated heterogeneity of included groups was 83.62% (p = 0.013). Hence, the heterogeneity was determined as high for both subgroup meta-analyses.
Forest plot of the included studies that assessed the accuracy of segmentation of high-grade glioma. Legend: DSC, dice similarity coefficient; CI, confidence interval. Forest plot shows that the performance of the MLAs to segment HGGs are centered around a DSC of 0.834 with a 95% CI ranging from 0.802 to 0.867
Forest plot of the included studies that assessed the accuracy of segmentation of low-grade glioma. Legend: DSC, dice similarity coefficient; CI, confidence interval. Forest plot shows that the performance of the MLAs to segment LGGs are centered around a DSC of 0.823 with a 95% CI ranging from 0.776 to 0.870
Publication bias
Studies included in the funnel plot were the ten studies that were meta-analyzed (Fig. 5). The funnel plot showed an asymmetrical shape, giving an indication for publication bias among included studies. Besides, not all studies were plotted within the area under the curve of the pseudo-95% CI, supporting the indication of possible publication bias [28].
Discussion
Various MLAs for the automated segmentation of gliomas were reviewed. Although heterogenous, MLAs showed to have a good DSC score with no differences between the segmentation of LGG and HGG. However, there were some indications for publication bias within this field of research.
Currently, segmentation of tumor lesions is a subjective and time-consuming task [58]. By replacing the current manual methods with an automated computer-aided approach, improvement of glioma quantification and subsequently radiomics can be achieved. However, automated segmentation of gliomas is a challenging task, due to the large variety of morphological tumor characteristics among patients [11]. As HGGs usually show more heterogeneous MRI characteristics, their automated segmentation could be expected to be more challenging compared to LGGs. Furthermore, the low proliferative state of LGGs likely results in lower perfusion and higher diffusion values in affected tissue [73, 74]. No performance difference was observed between the segmentation of HGGs and LGGs. Given the differences between HGGs and LGGs, it was expected that significant differences would arise in automatic segmentation tasks. Nevertheless, the ground truth segmentations were based on manual delineation by a (neuro)radiologist, indicating that the performance of automatic segmentation could only be as good as the ground truth segmentations. In addition, the ground truth of BraTS 2015 was first produced by algorithms and then verified by annotators, whereas the ground truth of BraTS 2013 fused multiple manual annotations.
Although MLAs performing automated segmentation show quite promising results (overall DSC score of 0.84; 95% CI: 0.82–0.86), there is still no wide acceptance and implementation of these methodologies in daily clinical practice. One of the explanations for this can be found in the different MLA methodologies; different MLA approaches and their exact details have a significant impact on the outcomes, even when applied to the same dataset. For example, in the BraTS 2019 challenge, the top three with regard to the segmentation task comprised a two-stage cascaded U-Net [75], a deep convolution neural network [76], and an ensemble of 3D-to-2D CNNs [77].
Another reason may be the absence of standardized procedures on how to properly use these segmentation systems. There are substantial differences between advanced systems that offer computer-aided segmentation and the current standards for neuroradiologists, which impedes the integration of MLA methods. CE-certified software is limitedly available in clinical practice, which is one of the reasons for the impediment. Also, the purpose for the use of MLAs varies; where radiologists mainly use these techniques for follow-up, neurosurgeons mostly use MLAs for therapeutic planning. In addition, direct integration into the neuroradiologist’s daily practice without extra time spent on the task will be needed to make automatic glioma segmentation feasible. Moreover, the current automated segmentations still need to be supervised by trained observers. It seems more likely that implementation of MLAs in neuroradiology will lead to an interaction between doctor and computer so that neuroradiologists will utilize more advanced technologies in the establishment of diagnoses [78]. The future implementation of MLAs in the diagnosis of glioma is of great clinical relevance, as these algorithms can support the non-invasive analysis of tumor characteristics without the need of histopathological tissue assessment. More specifically, automatic segmentations form the basis of further sophisticated analyses to clarify meaningful and reliable associations between neuroimaging features and survival rate [79, 80]. In conclusion, as automated segmentation of glioma is considered to be the first step in this process, the implementation of MLAs holds great potential for the future of neuroradiology.
Various publications were found with regard to the automated segmentation of gliomas in the post-operative setting [81,82,83,84]. Quantitative metrics are believed to be needed for therapy guidance, risk stratification, and outcome prognostication in the post-operative setting. MLAs could also represent a potential solution for automated quantitative measurements of the burden of disease in the post-operative setting. As shown in Table 2, however, the DSC scores of these studies are lower as compared to the DSC scores of the pre-operative MLA-based segmentations [81,82,83,84]. An explanation for these differences in performance could be the post-surgical changes of the brain parenchyma and the presence of air and blood products in the post-operative setting. Together these factors have been reported to affect the performance of MLAs [81].
Several methodological shortcomings of the present meta-analysis should be considered. First, various studies were excluded for the quantitative synthesis, due to missing data. Besides, heterogeneity of all analyses was considerably high, probably caused by technical variances of different MLA methodologies for segmentation. Lastly, only four out of 42 studies performed an out-of-sample external validation, emphasizing the importance of external validation to assess the robustness. It is probable that publication bias was present as there is no interest in the publication of poorly performing MLAs. In addition, differences in MR sequence input, ground truth, and other variables could play a role with regard to the outcomes, although this was considered a minor limitation as the source data across studies was similar in most studies.
Future gains of research on this topic may include an ensemble approach, as this might significantly boost the performance of segmentation. Thus, in addition, to focus current research on training individual segmentation systems, it may be interesting to investigate the fusion of multiple systems as well (i.e., segmentation of different imaging features in order to obtain different imaging biomarkers) [11]. Lastly, all included studies used retrospectively collected data, most of which using data from the BRATS databases. In order to further validate the performance of segmentation systems in clinical practice, larger-scale and external validated studies are preferred. In addition, data availability and providing online tools or downloadable scripts of the used MLAs could enhance future developments within this field of research significantly.
Conclusion
In this study, a systematic review and meta-analysis of different studies using MLA for glioma segmentation shows good performance. However, external validation is often not carried out, which should be regarded as a significant limitation in this field of research. Therefore, further verification of the accuracy of these models is recommended. It is crucial that quality guidelines are followed when reporting on MLAs, which includes validation on an external test set.
Abbreviations
- AI:
-
Artificial intelligence
- BraTS:
-
Brain tumor segmentation
- CI:
-
Confidence interval
- DSC:
-
Dice similarity coefficient
- GBM:
-
Glioblastoma multiforme
- HGG:
-
High-grade glioma
- LGG:
-
Low-grade glioma
- MLA:
-
Machine learning algorithm
- MRI:
-
Magnetic resonance imaging
- SD:
-
Standard deviation
- SE:
-
Standard error
References
Perry A, Wesseling P (2016) Histologic classification of gliomas handbook of clinical neurology. Elsevier, pp 71–95
Mazzara GP, Velthuizen RP, Pearlman JL, Greenberg HM, Wagner H (2004) Brain tumor target volume determination for radiation treatment planning through automated MRI segmentation. Int J Radiat Oncol Biol Phys 59:300–312
Yamahara T, Numa Y, Oishi T et al (2010) Morphological and flow cytometric analysis of cell infiltration in glioblastoma: a comparison of autopsy brain and neuroimaging. Brain Tumor Pathol 27:81–87
Bauer S, Wiest R, Nolte LP, Reyes M (2013) A survey of MRI-based medical image analysis for brain tumor studies. Phys Med Biol 58:R97–R129
Johnson DR, Guerin JB, Giannini C, Morris JM, Eckel LJ, Kaufmann TJ (2017) 2016 Updates to the WHO brain tumor classification system: what the radiologist needs to know. Radiographics 37:2164–2180
Larsen J, Wharton SB, McKevitt F et al (2017) ‘Low grade glioma’: an update for radiologists. Br J Radiol 90:20160600
Gordillo N, Montseny E, Sobrevilla P (2013) State of the art survey on MRI brain tumor segmentation. Magn Reson Imaging 31:1426–1438
Velthuizen RP, Hall LO, Clarke LP (1999) Feature extraction for MRI segmentation. J Neuroimaging 9:85–90
Ditmer A, Zhang B, Shujaat T et al (2018) Diagnostic accuracy of MRI texture analysis for grading gliomas. J Neurooncol 140:583–589
Egger J, Kapur T, Fedorov A et al (2013) GBM volumetry using the 3D Slicer medical image computing platform. Sci Rep 3:1364. https://doi.org/10.1038/srep01364
Menze BH, Jakab A, Bauer S et al (2015) The multimodal brain tumor image segmentation benchmark (BRATS). IEEE Trans Med Imaging 34:1993–2024
Chaddad A, Kucharczyk MJ, Daniel P et al (2019) Radiomics in glioblastoma: current status and challenges facing clinical implementation. Front Oncol 9:374
Pereira S, Pinto A, Alves V, Silva CA (2016) Brain tumor segmentation using convolutional neural networks in MRI images. IEEE Trans Med Imaging 35:1240–1251
Havaei M, Dutil F, Pal C, Larochelle H, Jodoin P-M (2015) A convolutional neural network approach to brain tumor segmentation BrainLes 2015. Springer, pp 195–208
Randhawa RS, Modi A, Jain P, Warier P (2016) Improving boundary classification for brain tumor segmentation and longitudinal disease progression. Brainlesion: Glioma, Multiple Sclerosis, Stroke and Traumatic Brain Injuries, 2016 10154:65–74
Long J, Shelhamer E, Darrell T (2015) Fully convolutional networks for semantic segmentation. 2015 Ieee Conference on Computer Vision and Pattern Recognition (Cvpr). https://doi.org/10.1109/cvpr.2015.7298965:3431-3440
Kamnitsas K, Ledig C, Newcombe VFJ et al (2017) Efficient multi-scale 3D CNN with fully connected CRF for accurate brain lesion segmentation. Med Image Anal 36:61–78
Ronneberger O, Fischer P, Brox T (2015) U-Net: convolutional networks for biomedical image segmentation. In: Navab N, Hornegger J, Wells W, Frangi A (eds) MICCAI 9351. Springer, Cham. https://doi.org/10.1007/978-3-319-24574-4_28
Çiçek Ö, Abdulkadir A, Lienkamp SS, Brox T, Ronneberger O (2016) 3D U-Net: learning dense volumetric segmentation from sparse annotation International conference on medical image computing and computer-assisted intervention. Springer, pp 424–432
Sakai K, Yamada K (2019) Machine learning studies on major brain diseases: 5-year trends of 2014-2018. Jpn J Radiol 37:34–72
Lotan E, Jain R, Razavian N, Fatterpekar GM, Lui YW (2018) State of the art: machine learning applications in glioma imaging. AJR Am J Roentgenol 212:26–37
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341
Liu XX, Faes L, Kale AU et al (2019) A comparison of deep learning performance against health-care professionals in detecting diseases from medical imaging: a systematic review and meta-analysis. Lancet Digital Health 1:E271–E297
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594
Moons KG, Altman DG, Reitsma JB et al (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162:W1–W73
Collins GS, Moons KGM (2019) Reporting of artificial intelligence prediction models. Lancet 393:1577–1579
Pinto dos Santos D (2020) Assessing radiology research on artificial intelligence: a brief guide for authors, reviewers and readers. European Society of Radiology. Available via https://ai.myesr.org/publications/assessing-radiology-research-on-artificial-intelligence-a-brief-guide-for-authors-reviewers-and-readers/. Accessed 5 Oct 2020
Higgins JPT (2011) GSe Cochrane handbook for systematic reviews of interventions Version 5.1.0 [updated March 2011], The Cochrane Collaboration
Yeghiazaryan V, Voiculescu I (2018) Family of boundary overlap metrics for the evaluation of medical image segmentation. J Med Imaging (Bellingham) 5:015006
Taha AA, Hanbury A (2015) Metrics for evaluating 3D medical image segmentation: analysis, selection, and tool. BMC Med Imaging 15:29
Viechtbauer W (2010) Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software, 36(3):1–48. https://doi.org/10.18637/jss.v036.i03
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Amirmoezzi Y, Salehi S, Parsaei H, Kazemi K, Torabi Jahromi A (2019) A knowledge-based system for brain tumor segmentation using only 3D FLAIR images. Australas Phys Eng Sci Med 42:529–540
Banerjee S, Mitra S (2020) Novel volumetric sub-region segmentation in brain tumors. Front Comput Neurosci 14:3
Bonte S, Goethals I, Van Holen R (2018) Machine learning based brain tumour segmentation on limited data using local texture and abnormality. Comput Biol Med 98:39–47
Choi Y, Nam Y, Lee YS et al (2020) IDH1 mutation prediction using MR-based radiomics in glioblastoma: comparison between manual and fully automated deep learning-based approach of tumor segmentation. Eur J Radiol 128:109031
Cui S, Mao L, Jiang J, Liu C, Xiong S (2018) Automatic semantic segmentation of brain gliomas from MRI images using a deep cascaded neural network. J Healthc Eng 2018:4940593
Hasan SMK, Linte CA (2018) A modified U-Net convolutional network featuring a nearest-neighbor re-sampling-based elastic-transformation for brain tissue characterization and segmentation. Proc IEEE West N Y Image Signal Process Workshop 2018
Havaei M, Davy A, Warde-Farley D et al (2017) Brain tumor segmentation with deep neural networks. Med Image Anal 35:18–31
Havaei M, Larochelle H, Poulin P, Jodoin PM (2016) Within-brain classification for brain tumor segmentation. Int J Comput Assist Radiol Surg 11:777–788
Hussain S, Anwar SM, Majid M (2017) Brain tumor segmentation using cascaded deep convolutional neural network. Annu Int Conf IEEE Eng Med Biol Soc 2017:1998–2001
Iqbal S, Ghani Khan MU, Saba T et al (2019) Deep learning model integrating features and novel classifiers fusion for brain tumor segmentation. Microsc Res Tech 82:1302–1315
Iqbal S, Ghani MU, Saba T, Rehman A (2018) Brain tumor segmentation in multi-spectral MRI using convolutional neural networks (CNN). Microsc Res Tech 81:419–427
Jiang J, Wu Y, Huang M, Yang W, Chen W, Feng Q (2013) 3D brain tumor segmentation in multimodal MR images based on learning population- and patient-specific feature sets. Comput Med Imaging Graph 37:512–521
Kao PY, Shailja S, Jiang J et al (2019) Improving patch-based convolutional neural networks for MRI brain tumor segmentation by leveraging location information. Front Neurosci 13:1449
Li Z, Wang Y, Yu J et al (2017) Low-grade glioma segmentation based on CNN with fully connected CRF. J Healthc Eng 2017:9283480
Liu Y, Shi X, Xia Y et al (2018) Multi-scale V-Net: a deep learning framework for brain tumor segmentation in multiparametric MRI. Med Phys 45(6):e568
Meng Z, Fan Z, Zhao Z, Su F (2018) ENS-Unet: end-to-end noise suppression U-Net for brain tumor segmentation. Annu Int Conf IEEE Eng Med Biol Soc 2018:5886–5889
Naceur MB, Saouli R, Akil M, Kachouri R (2018) Fully automatic brain tumor segmentation using end-to-end incremental deep neural networks in MRI images. Comput Methods Programs Biomed 166:39–49
Naser MA, Deen MJ (2020) Brain tumor segmentation and grading of lower-grade glioma using deep learning in MRI images. Comput Biol Med 121:103758
Perkuhn M, Stavrinou P, Thiele F et al (2018) Clinical evaluation of a multiparametric deep learning model for glioblastoma segmentation using heterogeneous magnetic resonance imaging data from clinical routine. Invest Radiol 53:647–654
Razzak MI, Imran M, Xu G (2019) Efficient brain tumor segmentation with multiscale two-pathway-group conventional neural networks. IEEE J Biomed Health Inform 23:1911–1919
Savareh BA, Emami H, Hajiabadi M, Azimi SM, Ghafoori M (2019) Wavelet-enhanced convolutional neural network: a new idea in a deep learning paradigm. Biomed Tech (Berl) 64:195–205
Soltaninejad M, Yang G, Lambrou T et al (2018) Supervised learning based multimodal MRI brain tumour segmentation using texture features from supervoxels. Comput Methods Programs Biomed 157:69–84
Sun J, Chen W, Peng S, Liu B (2019) DRRNet: dense residual refine networks for automatic brain tumor segmentation. J Med Syst 43:221
Wang F, Niu J, Fan W, Cao Q (2018) Brain tumor medical image segmentation based on CRF 3D-CNN introduction. Basic Clin Paharmacol Toxicol 124(Supplement 2):12
Wu S, Li H, Quang D, Guan Y (2020) Three-plane-assembled deep learning segmentation of gliomas. Radiol Artif Intell 2:e190011
Wu Y, Zhao Z, Wu W, Lin Y, Wang M (2019) Automatic glioma segmentation based on adaptive superpixel. BMC Med Imaging 19:73
Yang C, Guo X, Wang T et al (2019) Automatic brain tumor segmentation method based on modified convolutional neural network. Annu Int Conf IEEE Eng Med Biol Soc 2019:998–1001
Yang T, Song J, Li L (2019) A deep learning model integrating SK-TPCNN and random forests for brain tumor segmentation in MRI. Biocybern Biomed Eng 39(3):613–623. https://doi.org/10.1016/j.bbe.2019.06.003
Yang T, Song J, Li L, Tang Q (2020) Improving brain tumor segmentation on MRI based on the deep U-net and residual units. J Xray Sci Technol 28:95–110
Zhao L, Wu W, Corso JJ (2013) Semi-automatic brain tumor segmentation by constrained MRFs using structural trajectories. Med Image Comput Comput Assist Interv 16:567–575
Zhou Z, He Z, Shi M, Du J, Chen D (2020) 3D dense connectivity network with atrous convolutional feature pyramid for brain tumor segmentation in magnetic resonance imaging of human heads. Comput Biol Med 121:103766
Zhuge Y, Krauze AV, Ning H et al (2017) Brain tumor segmentation using holistically nested neural networks in MRI images. Med Phys 44:5234–5243
Dong H, Yang G, Liu F, Mo Y, Guo Y (2017) Automatic brain tumor detection and segmentation using U-Net based fully convolutional networks. In: Valdés Hernández M, González-Castro V (eds) Medical image understanding and analysis. Springer International Publishing, Cham, pp 506–517
Dvorak P, Menze B (2015) Local structure prediction with convolutional neural networks for multimodal brain tumor segmentation. In International MICCAI workshop on medical computer vision. Springer, Cham, pp 59–71
Lyksborg M, Puonti O, Agn M, Larsen R (2015) An ensemble of 2D convolutional neural networks for tumor segmentation. In: Paulsen RR, Pedersen KS (eds) Image Analysis. Springer International Publishing, Cham, pp 201–211
Pinto A, Pereira S, Correia H, Oliveira J, Rasteiro DMLD, Silva CA (2015) Brain tumour segmentation based on extremely randomized forest with high-level features. 2015 37th Annual International Conference of the Ieee Engineering in Medicine and Biology Society (Embc):3037–3040
Tustison NJ, Shrinidhi KL, Wintermark M et al (2015) Optimal symmetric multimodal templates and concatenated random forests for supervised brain tumor segmentation (simplified) with ANTsR. Neuroinformatics 13:209–225
Usman K, Rajpoot K (2017) Brain tumor classification from multi-modality MRI using wavelets and machine learning. Pattern Anal Applic 20:871–881
Xue Y, Xu T, Zhang H, Long LR, Huang XL (2018) SegAN: adversarial network with multi-scale L (1) loss for medical image segmentation. Neuroinformatics 16:383–392
Zikic D, Glocker B, Konukoglu E et al (2012) Decision forests for tissue-specific segmentation of high-grade gliomas in multi-channel MRInternational Conference on Medical Image Computing and Computer-Assisted Intervention. Springer, 369–376
Durmo F, Lätt J, Rydelius A et al (2018) Brain tumor characterization using multibiometric evaluation of MRI. Tomography 4:14–25
De Baene W, Rutten GJM, Sitskoorn MM (2017) The temporal pattern of a lesion modulates the functional network topology of remote brain regions. Neural Plast 2017:3530723
Jiang Z, Ding C, Liu M, Tao D (2020) Two-stage cascaded U-Net: 1st place solution to BraTS challenge 2019 segmentation task. Springer International Publishing, Cham, pp 231–241
Zhao Y-X, Zhang Y-M, Liu C-L (2020) Bag of tricks for 3D MRI brain tumor segmentation. Springer International Publishing, Cham, pp 210–220
McKinley R, Rebsamen M, Meier R, Wiest R (2020) Triplanar ensemble of 3D-to-2D CNNs with label-uncertainty for brain tumor segmentation. Springer International Publishing, Cham, pp 379–387
Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts H (2018) Artificial intelligence in radiology. Nat Rev Cancer 18:500–510
Kumar V, Gu Y, Basu S et al (2012) Radiomics: the process and the challenges. Magn Reson Imaging 30:1234–1248
Lambin P, Rios-Velazquez E, Leijenaar R et al (2012) Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer 48:441–446
Herrmann E, Ermis E, Meier R et al (2019) Fully automated segmentation of the brain resection cavity for radiation target volume definition in glioblastoma patients. Strahlenther Onkol 195:586–586
Meier R, Knecht U, Loosli T et al (2016) Clinical evaluation of a fully-automatic Segmentation method for longitudinal brain tumor volumetry. Sci Rep 6:23376. https://doi.org/10.1038/srep23376
Zeng K, Bakas S, Sotiras A et al (2016) Segmentation of gliomas in pre-operative and post-operative multimodal magnetic resonance imaging volumes based on a hybrid generative-discriminative framework. Brainlesion 10154:184–194
Tang F, Liang S, Zhong T et al (2020) Postoperative glioma segmentation in CT image using deep feature fusion model guided by multi-sequence MRIs. Eur Radiol 30:823–832
Acknowledgements
The authors would like to acknowledge Dr. Rogier Donders for his statistical insights.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is professor Mathias Prokop (MD, PhD) of Radboudumc, Nijmegen, The Netherlands.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Biostatistician Dr. Rogier Donders kindly provided statistical advice for this manuscript. Also, multiple authors have significant statistical expertise.
Informed consent
No informed consent was needed for the conducting of this review.
Ethical approval
Institutional Review Board approval was not required because this review did not include specimens or involve any treatments or interventions.
Study subjects or cohorts overlap
All of the included studies have been previously reported, either as an original research paper or a conference paper.
Methodology
• Systematic review
• meta-analysis
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 19 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Kempen, E.J., Post, M., Mannil, M. et al. Performance of machine learning algorithms for glioma segmentation of brain MRI: a systematic literature review and meta-analysis. Eur Radiol 31, 9638–9653 (2021). https://doi.org/10.1007/s00330-021-08035-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08035-0