Abstract
Objective
The purpose of this study was to determine how well radiologists could visually detect a change in lung nodule size on the basis of visual image perception alone.
Subjects and methods
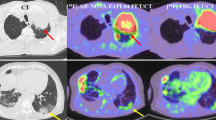
Under IRB approval, 109 standard chest CT image series were anonymized and exported from PACS. Nine hundred forty virtual lung nodule pairs (six baseline diameters, six relative volume differences, two nodule types—solid and ground glass—and 14 repeats) were digitally inserted into the chest CT image series (same location, different sizes between the pair). These digitally altered CT image pairs were shown to nine radiologists who were tasked to visually determine which image contained the larger nodule using a two-alternative forced-choice perception experimental design. These data were statistically analyzed using a generalized linear mixed effects model to determine how accurately the radiologists were able to correctly identify the larger nodule.
Results
Nominal baseline nodule diameter, relative volume difference, and nodule type were found to be statistically significant factors (p < 0.001) in influencing the radiologists’ accuracy. For solid (ground-glass) nodules, the baseline diameter needed to be at least 6.3 mm (13.2 mm) to be able to visually detect a 25% change in volume with 95 ± 1.4% accuracy. Accuracy was lowest for the nodules with the smallest baseline diameters and smallest relative volume differences. Additionally, accuracy was lower for ground-glass nodules compared to solid nodules.
Conclusions
Factors that impacted visual size assessment were baseline nodule diameter, relative volume difference, and solid versus non-solid nodule type, with larger and more solid lesions offering a more precise assessment of change.
Key Points
• For solid nodules, radiologists could visually detect a 25% change in volume with 95% accuracy for nodules having greater than 6.3-mm baseline diameter.
• For ground-glass nodules, radiologists could visually detect a 25% change in volume with 95% accuracy for nodules having greater than 13.2-mm baseline diameter.
• Accuracy in detecting a change in nodule size began to stabilize around 90–100% for nodules with larger baseline diameters (> 8 mm for solid nodules, > 12 mm for ground-glass nodules) and larger relative volume differences (>15% for solid nodules, > 25% for ground-glass nodules).




Similar content being viewed by others
Abbreviations
- 2AFC:
-
Two-alternative forced-choice
References
National Lung Screening Trial Research Team, Aberle DR, Adams AM et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365:395–409
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34
Yousaf-Khan U, van der Aalst C, de Jong PA et al (2017) Final screening round of the NELSON lung cancer screening trial: the effect of a 2.5-year screening interval. Thorax 72:48–56
Bankier AA, MacMahon H, Goo JM, Rubin GD, Schaefer-Prokop CM, Naidich DP (2017) Recommendations for measuring pulmonary nodules at CT: a statement from the Fleischner Society. Radiology 285:584–600
Callister ME, Baldwin DR, Akram AR et al (2015) British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax 70(Suppl 2):ii1–ii54
Devaraj A, van Ginneken B, Nair A, Baldwin D (2017) Use of volumetry for lung nodule management: theory and practice. Radiology 284:630–644
van Klaveren RJ, Oudkerk M, Prokop M et al (2009) Management of lung nodules detected by volume CT scanning. N Engl J Med 361:2221–2229
Wilson DO, Ryan A, Fuhrman C, Schuchert M, Shapiro S, Siegfried JM, Weissfeld J (2012) Doubling times and CT screen–detected lung cancers in the Pittsburgh Lung Screening Study. Am J Respir Crit Care Med 185:85–89
Scholten ET, de Hoop B, Jacobs C et al (2013) Semi-automatic quantification of subsolid pulmonary nodules: comparison with manual measurements. PLoS One 8:e80249
Strasburger H, Huber J, Rose D (2018) Ewald Hering’s (1899) On the limits of visual acuity: a translation and commentary: with a supplement on Alfred Volkmann’s (1863) physiological investigations in the field of optics. Iperception 9:2041669518763675
Field JK, Duffy SW, Baldwin DR et al (2016) The UK Lung Cancer Screening Trial: a pilot randomised controlled trial of low-dose computed tomography screening for the early detection of lung cancer. Health Technol Assess 20:1–146
Pastorino U, Rossi M, Rosato V et al (2012) Annual or biennial CT screening versus observation in heavy smokers: 5-year results of the MILD trial. Eur J Cancer Prev 21:308–315
Solomon J, Samei E (2014) A generic framework to simulate realistic lung, liver and renal pathologies in CT imaging. Phys Med Biol 59:6637–6657
Singh S, Pinsky P, Fineberg NS et al (2011) Evaluation of reader variability in the interpretation of follow-up CT scans at lung cancer screening. Radiology 259:263–270
Revel MP, Bissery A, Bienvenu M, Aycard L, Lefort C, Frija G (2004) Are two-dimensional CT measurements of small noncalcified pulmonary nodules reliable. Radiology 231:453–458
Funding
This study did not have funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ehsan Samei.
Conflict of interest
The authors of this manuscript declare relationships with the following companies:
-
Justin Solomon has relationships with the following entities, unrelated to the present publication: 12 Sigma, Sun Nuclear, Metis Health Analytics.
-
Ehsan Samei has relationships with the following entities unrelated to the present publication: GE, Siemens, Bracco, Imalogix, 12 Sigma, Sun Nuclear, Metis Health Analytics, Cambridge University Press, and Wiley and Sons.
Statistics and biometry
Justin Solomon and Ehsan Samei have statistical expertise and provided the analysis.
Informed consent
Written informed consent was waived by the Institutional Review Board because this was a retrospective study on anonymized image data.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lukas Ebner is a co-first author.
Rights and permissions
About this article
Cite this article
Solomon, J., Ebner, L., Christe, A. et al. Minimum perceivable size difference: how well can radiologists visually detect a change in lung nodule size from CT images?. Eur Radiol 31, 1947–1955 (2021). https://doi.org/10.1007/s00330-020-07326-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07326-2