Abstract
Purpose
To systematically investigate the frequency and types of allegations related to radiology practice handled by the Dutch Medical Disciplinary Court in the past 10 years.
Methods
The Dutch Medical Disciplinary Court database was searched for verdicts concerning radiology practice between 2010 and 2019. The association between the number of verdicts and time (years) was assessed by Spearman’s rho. Other data were summarized using descriptive statistics.
Results
There were 48 verdicts (mean 4.8 per year). There was no significant association between the number of verdicts and time (Spearman’s rho < 0.001, p = 0.99). Most allegations were in breast imaging and musculoskeletal radiology (each 18.8%), followed by interventional radiology, head and neck imaging, and abdominal imaging (each 12.5%), neuroradiology and vascular imaging (each 10.4%), and chest imaging (4.2%). There were 46 allegations against radiologists (95.8%) and 2 against residents (4.2%). The most common allegation (37.5%) was error in diagnosis. In 20.8% of verdicts, the allegation was judged (partially) founded; disciplinary measures were warnings (n = 8) and reprimands (n = 2). An appeal was submitted by the patient in 11 cases and by the radiologist in 3 cases. All appeals by patients were rejected, whereas 2 of the 3 appeals by radiologists were granted and previously imposed disciplinary measures were reversed.
Conclusion
Allegations against radiologists at the Dutch Medical Disciplinary Court are relatively few, their number has remained stable over the past 10 years, and a minority were judged to be (partially) founded. We can learn from the cases presented in this article, which may improve patient care.
Key Points
• The frequency of allegations against radiologists at the Dutch Medical Disciplinary Court is relatively low and has not exhibited any temporal change over the past 10 years.
• These allegations reflect patient dissatisfaction, but this infrequently equals malpractice.
• Knowledge of the circumstances under which these allegations have arisen may improve patient care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiology is one of the medical specialties with the highest number of malpractice suits in the USA [1]. The likelihood of a radiologist in the USA being the defendant in at least one suit is 50% by age 60 [2]. It can be expected that the number of malpractice suits will further increase [3, 4]. Data from the USA show that diagnostic errors are by far the most common cause of malpractice suits, whereas failure to communicate and failure to recommend additional testing are both uncommon reasons for initiating a suit [1, 5]. There are relatively few published data regarding malpractice suits against radiologists in Europe [6, 7] compared with those against radiologists in the USA [1, 2, 5, 8,9,10,11,12,13,14,15,16,17]. The medical disciplinary law system in The Netherlands is unique and essentially different from a medical malpractice claim system, because its main objective is to maintain and improve the quality of healthcare rather than punishing healthcare professionals and/or financially compensating patients [18, 19]. In addition, patients can allege healthcare professionals without proceeding to civil court or insurance claims. To our knowledge, verdicts by the Dutch Medical Disciplinary Court related to radiology practice have not been systematically investigated yet. In addition, it is still unknown if the frequency of patient allegations has remained stable or if it has changed over the years. This information may be helpful to radiologists to improve the care they provide to their patients, and to prevent patient dissatisfaction and allegations. Furthermore, this experience may be valuable to governmental bodies and healthcare policy makers in other countries who wish to reform their medical disciplinary law system from a malpractice claim system into a system akin the Dutch. Therefore, the objective of our study was to systematically investigate the frequency and types of allegations related to radiology practice handled by the Dutch Medical Disciplinary Court in the past 10 years.
Methods
The online database of the Dutch Medical Disciplinary Court is publicly available and all data are anonymized. Therefore, ethics committee approval was not applicable for this study.
Data collection
The database of the Dutch Medical Disciplinary Court (https://tuchtrecht.overheid.nl/nieuw/gezondheidszorg) was searched for verdicts published in the past 10 years (2010–2019). All cases handled by this institute (which consists of independent medical and legal experts) are published in detail online 1 day after the verdict. Only verdicts concerning allegations against radiologists or radiology residents were selected and included in the present study. Verdicts concerning allegations which were not directly related to radiology practice (such as private affairs or non-radiological work) were excluded.
Data extraction and analysis
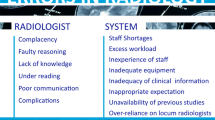
The following data were extracted for each verdict: radiological subspecialty, whether a radiologist or resident was alleged, number of days between date of filing the allegation and date of the verdict, the type of allegation, the verdict, the type of disciplinary measure (Table 1), if the allegation was judged to be (partially) founded, and whether there was an appeal against the verdict. In order to determine whether the number of verdicts has either increased or remained stable over time, we calculated Spearman’s rho between the number of verdicts and time (years). Other data were summarized using descriptive statistics. In cases in which the allegation was judged (partially) founded, we determined (potential) causes that have led to error/malpractice [20, 21].
Results
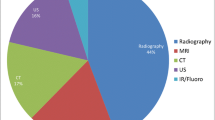
There were 52 verdicts. Four verdicts were excluded, because they were not directly related to radiology practice. Eventually, 48 verdicts were included (Table 2).There was no significant association between the number of verdicts and time (Spearman’s rho < 0.001, p = 0.99) (Fig. 1a). Most allegations were in breast imaging and musculoskeletal radiology (each 18.8%), followed by interventional radiology, head and neck imaging, and abdominal imaging (each 12.5%), neuroradiology and vascular imaging (each 10.4%), and chest imaging (4.2%) (Fig. 1b). There were 46 allegations against radiologists (95.8%) and 2 allegations against residents (4.2%) (Fig. 1c). The most common allegation was error in diagnosis (19/48 cases, 39.6%). In 10/48 verdicts (20.8%), the allegation was judged (partially) founded; disciplinary measures were warnings (n = 8) and reprimands (n = 2) (Fig. 1d). All 11 appeals by patients were rejected, whereas 2 of 3 appeals by radiologists were granted and the previously imposed disciplinary measures were reversed. (Potential) causes leading to error/malpractice in cases in which the allegation was judged (partially) founded are displayed in Table 3.
Number of verdicts by the Dutch Medical Disciplinary Court for each year between 2010 and 2019 (a), number of allegations per subspecialty (b), number of allegations against radiologists and residents (c), and types of disciplinary measures for the 10 verdicts in which the allegation was judged (partially) founded by the Dutch Medical Disciplinary Court (d)
Discussion
The results of our study show that the Dutch Medical Disciplinary Court handles a mean of 4.8 allegations against radiologists related to radiology practice per year, and that this frequency has remained stable over the past 10 years. A mean of 4.8 allegations per year can be considered few, given that the mean number of cases against all Dutch health care professionals is 1709 per year [22] and that there are nearly as much as 1300 regular registered radiologists in The Netherlands at present [23]. There is no real financial obstacle or risk for a patient to file an allegation against a health care professional at the Dutch Medical Disciplinary Court. Patients can file an allegation for a total amount of 50 €, which will be refunded if the allegation is judged to be (partially) founded [24]. This very much contrasts with the civil court in The Netherlands, where the costs of the lawsuit process and the legal fees of the winning party have to be paid by the losing party if decided by the judge [25]. The relatively low number of allegations against radiologists filed at the Dutch Medical Disciplinary Court may be explained because there is not a real compensation culture in The Netherlands yet. One may also speculate that individual healthcare institutions handle a lot of patient complaints by themselves, which could reduce or avoid the number of allegations filed at the Dutch Medical Disciplinary Court. However, written complaints regarding radiological procedures in The Netherlands are also relatively few (14.4 per 100,000 radiological procedures) [26]. Therefore, the relatively low number of allegations may also indicate an overall high quality of radiology practice in The Netherlands. Accordingly, The Netherlands is frequently ranked as having one of the best healthcare systems in Europe [27].
A minority of allegations were judged to be (partially) founded. The Dutch Medical Disciplinary Court imposed 8 warnings and 2 reprimands to radiologists in the past 10 years (of which two were rejected after appeal). These disciplinary measures are the lowest penalties which can be imposed by the Dutch Medical Disciplinary Court. However, the impact of the disciplinary process and the measures itself should not be underestimated. Alleged healthcare professionals describe feelings of misery and insecurity both during the process as in its aftermath, and they fear receiving new complaints and provide care more cautiously after the imposed measure [28, 29]. This in turn may lead to defensive medicine, which is an important contributor to healthcare costs without adding any benefit to patients [30,31,32,33].
Error in diagnosis was the most common allegation (39.6%) filed at the Dutch Medical Disciplinary Court and most allegations were in the subspecialties breast imaging and musculoskeletal radiology. These findings are in accordance with previous studies on medical malpractice suits in the USA [1, 34], the UK [6], and Italy [7]. Errors are common, with an estimated day-to-day rate of 3–5% of radiology studies reported [35]. Radiologist reporting performance cannot be perfect, and some errors are inevitable [35]. However, there are strategies to avoid error and malpractice and we can learn from our mistakes (see Table 3). We also refer to the informative medicolegal series by L. Berlin, which have been published in the American Journal of Roentgenology in the past years [36]. We further note that radiologists should think about the consequences of error and malpractice in the context of the trend of using artificial intelligence. However, the question of “who is responsible for the diagnosis” when using artificial intelligence (being it either data scientists, manufacturers, and/or radiologists) remains to be answered [37].
Our study has some limitations. First, because our study included only data from The Netherlands, it is not sure whether our results are generalizable to other (European) countries, which have different law systems. Notably, a study which was published in 2010 showed a much higher risk of medical malpractice litigation for Italian radiologists, which was comparable to that for radiologists in the USA [7].
Italy, however, may be an exception among European countries [38]. Second, we only included data from the Dutch Medical Disciplinary Court. Because patients may also proceed to the civil court where they can file an allegation in parallel or separately from the Dutch Medical Disciplinary Court, the number of all official allegations may be underestimated. However, it was not possible to perform an unbiased research of civil court data, because only a selected part of civil court verdicts are publicly published [39]. Furthermore, the Dutch Medical Disciplinary Court essentially differs from civil court in that its main objective is to maintain and improve the quality of healthcare rather than punishing healthcare professionals. Third, we did not investigate the amount of time and attorney costs (83.3% used an attorney during the court session) spent by defendants. Fourth, we did not investigate the psychological impact of disciplinary measures on radiologists and whether these disciplinary measures achieved their primary goal: to maintain and improve the quality of healthcare. The systematic presentation of cases in this article may further contribute to the quality of radiology practice in general.
In conclusion, allegations against radiologist at the Dutch Medical Disciplinary Court are relatively few, their number has remained stable over the past 10 years, and a minority were judged to be (partially) founded. We can learn from the cases presented in this article, which may improve patient care.
Abbreviations
- UK:
-
United Kingdom
- USA:
-
United States of America
References
Whang JS, Baker SR, Patel R, Luk L, Castro A 3rd (2013) The causes of medical malpractice suits against radiologists in the United States. Radiology 266:548–554
Baker SR, Whang JS, Luk L, Clarkin KS, Castro A 3rd, Patel R (2013) The demography of medical malpractice suits against radiologists. Radiology 266:539–547
Bonetti M, Cirillo P, Musile Tanzi P, Trinchero E (2016) An analysis of the number of medical malpractice claims and their amounts. PLoS One 11:e0153362
Klemann DMTV, Mertens HJMM, van Merode GG (2018) More and higher claims for damages: analysis of claims for damages in Dutch hospital care 2007-2016. Ned Tijdschr Geneeskd 162:D2279
Harvey HB, Tomov E, Babayan A et al (2016) Radiology malpractice claims in the United States from 2008 to 2012: characteristics and implications. J Am Coll Radiol 13:124–130
Halpin SF (2009) Medico-legal claims against English radiologists: 1995-2006. Br J Radiol 82:982–988
Fileni A, Magnavita N, Mirk P, Iavicoli I, Magnavita G, Bergamaschi A (2010) Radiologic malpractice litigation risk in Italy: an observational study over a 14-year period. AJR Am J Roentgenol 194:1040–1046
Hamer MM, Morlock F, Foley HT, Ros PR (1987) Medical malpractice in diagnostic radiology: claims, compensation, and patient injury. Radiology 164:263–266
Royal SA, Cloud GA, Atchison WM (1994) Malpractice in pediatric radiology: a survey in the United States and Canada. Pediatr Radiol 24:519–522
Berlin L, Berlin JW (1995) Malpractice and radiologists in Cook County, IL: trends in 20 years of litigation. AJR Am J Roentgenol 165:781–788
Barloon TJ, Shumway J (1995) Medical malpractice involving radiologic colon examinations: a review of 38 recent cases. AJR Am J Roentgenol 165:343–346
Baker SR, Patel RH, Yang L, Lelkes VM, Castro A 3rd (2013) Malpractice suits in chest radiology: an evaluation of the histories of 8265 radiologists. J Thorac Imaging 28:388–391
Baker SR, Lelkes V, Patel RH, Castro A 3rd, Sarmast U, Whang J (2013) Spinal-related malpractice suits against radiologists in the USA-rates, anatomic location, percent of adverse judgments, and average payments. Emerg Radiol 20:513–516
Baker SR, Patel RH, Lelkes V, Castro A 3rd, Sarmast U, Whang J (2014) Non-spinal musculoskeletal malpractice suits against radiologists in the USA - rates, anatomic locations, and payments in a survey of 8,265 radiologists. Emerg Radiol 21:29–34
Baker SR, Shah S, Ghosh S, Castro A (2015) Radiology medical malpractice suits in gastrointestinal radiology: prevalence, causes, and outcomes. Emerg Radiol 22:141–145
Breen MA, Dwyer K, Yu-Moe W, Taylor GA (2017) Pediatric radiology malpractice claims - characteristics and comparison to adult radiology claims. Pediatr Radiol 47:808–816
Baker SR, Pentakota SR, Hubbi B (2018) Breast radiology malpractice suits: characteristics of frequency and outcomes- national and statewide distinctions. Breast J 24:360–364
https://www.tuchtcollege-gezondheidszorg.nl/ Accessed 22 Oct 2019
Alhafaji FY, Frederiks BJ, Legemaate J (2009) The Dutch system of handling complaints in health care. Med Law 28:241–255
Raskin MM (2006) Survival strategies for radiology: some practical tips on how to reduce the risk of being sued and losing. J Am Coll Radiol 3:689–693
Mezrich JL (2019) Hiding in the hedges: tips to minimize your malpractice risks as a radiologist. AJR Am J Roentgenol 5:1–5
https://www.tuchtcollege-gezondheidszorg.nl/over-de-tuchtcolleges/jaarcijfers-tuchtcolleges/jaarcijfers-2017/regionale-tuchtcolleges/overzicht-klachten-2013%2D%2D-2017 Accessed 22 Oct 2019
https://www.radiologen.nl/nvvr Accessed 22 Oct 2019
https://www.tuchtcollege-gezondheidszorg.nl/ik-heb-een-klacht Accessed 22 Oct 2019
https://wetten.overheid.nl/BWBR0001827/2015-07-01 Accessed 22 Oct 2019
van den Berg PF, Yakar D, Glaudemans AWJM, Dierckx RAJO, Kwee TC (2019) Patient complaints in radiology: 9-year experience at a European tertiary care center. Eur Radiol 29:5395–5402
Euro Health Consumer Index 2018. Available via https://healthpowerhouse.com/publications/#200118 Accessed 22 Oct 2019
Verhoef LM, Weenink JW, Winters S, Robben PB, Westert GP, Kool RB (2015) The disciplined healthcare professional: a qualitative interview study on the impact of the disciplinary process and imposed measures in the Netherlands. BMJ Open 5:e009275
Laarman BS, Bouwman RJ, de Veer AJ, Hendriks M, Friele RD (2019) How do doctors in the Netherlands perceive the impact of disciplinary procedures and disclosure of disciplinary measures on their professional practice, health and career opportunities? A questionnaire among medical doctors who received a disciplinary measure. BMJ Open 9:e023576
Studdert DM, Mello MM, Sage WM et al (2005) Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 293:2609–2617
Panella M, Rinaldi C, Leigheb F et al (2017) Prevalence and costs of defensive medicine: a national survey of Italian physicians. J Health Serv Res Policy 22:211–217
Reschovsky JD, Saiontz-Martinez CB (2018) Malpractice claim fears and the costs of treating Medicare patients: a new approach to estimating the costs of defensive medicine. Health Serv Res 53:1498–1516
Vento S, Cainelli F, Vallone A (2018) Defensive medicine: it is time to finally slow down an epidemic. World J Clin Cases 6:406–409
Siegal D, Stratchko LM, DeRoo C (2017) The role of radiology in diagnostic error: a medical malpractice claims review. Diagnosis (Berl) 4:125–131
Brady AP (2017) Error and discrepancy in radiology: inevitable or avoidable? Insights Imaging 8:171–182
https://www.ajronline.org/topic/mls Accessed 15 Dec 2019
European Society of Radiology (ESR) (2019) What the radiologist should know about artificial intelligence - an ESR white paper. Insights Imaging 10:44
Traina F (2009) Medical malpractice: the experience in Italy. Clin Orthop Relat Res 467:434–442
https://uitspraken.rechtspraak.nl/ Accessed 22 Oct 2019
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Robert M. Kwee.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Informed consent was not applicable for this study.
Ethical approval
Ethics committee approval was not applicable for this study.
Methodology
• Retrospective
• Observational
• Multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kwee, R.M., Kwee, T.C. Medical disciplinary jurisprudence in alleged malpractice in radiology: 10-year Dutch experience. Eur Radiol 30, 3507–3515 (2020). https://doi.org/10.1007/s00330-020-06685-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06685-0