Abstract
Background
All medical specialties have an inherent intrinsic risk of malpractice lawsuits. Radiodiagnosis is also not averse to this risk as it involves making decisions under uncertain situations which determine patient management.
Main body
There is an increasing trend of malpractice lawsuits against the radiologist due to the increased involvement of the radiologist in the management of the patient and the ever-increasing reliance of the referring physician on the radiologist for making a diagnosis and guiding management. These lawsuits commonly occur due to patient mismanagement and lack of communication. In this article, we overview the medical malpractice law and the causes of litigations against radiologists. This paper also reviews the ways by which a radiologist can reduce the risks and consequences of these lawsuits.
Conclusion
Awareness of the main medico-legal issues and insurance in the radiology field is very important for the radiologist to protect himself from malpractice litigation.
Similar content being viewed by others
Background
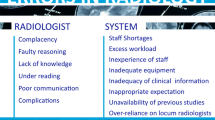
Over the last decade, radiology has become an integral part of the management of patients. This has led to new duties and liabilities related to diagnosis as well as interventional procedures. 4% of radiological interpretations have errors [1]. Many errors are small or are corrected before patient care. However, with increasing caseloads many errors still occur which affect patients and lead to malpractice lawsuits. Improper patient management or miscommunication between patient-physician due to these errors are the communist cause of medical malpractice lawsuits. Knowledge of state and federal laws can help the physician and the radiologist in managing complications arising from the errors. In this review article, we report the common reasons for lawsuits against radiologists and their legal consequences. We also highlight the present rules regarding radiological malpractice. Finally, we review the advice provided in multiple published literature for reducing the risk of malpractice [2] (Figs. 1 and 2).
Main text
Common causes of malpractice
A US-based study [3] revealed that the commonest cause of lawsuits against radiologists was an error in diagnosis (14.83 claims per 1000 person-years) rather than a delay in diagnosis. The next commonest cause was complications during a procedure and miscommunication with the patient or their doctors. Among body parts, breast-related imaging findings were the most frequent reason for incorrect diagnoses and lawsuits. In interventional radiology, vascular injuries were the commonest cause of lawsuits. Miscommunication with either treating doctors or patients was the least frequent cause of malpractice lawsuits.
A European study reported a frequency of 44 per 1000 cases of malpractice lawsuits annually with the total incidence ranging between 3.6 and 12.6% depending on the European country [4]. Most of them involved interventional radiological procedures. Among the procedures, vascular injuries followed by injury due to needle biopsies were the commonest cause of lawsuits. The commonest body parts for diagnostic errors were the bones (44.5%), breast (25.8%), chest (11.4%), and lastly the abdomen (8.3%) [4].
A retrospective study in England similarly showed that the commonest cause of a lawsuit was an incorrect or delayed diagnosis of cancer, out of which the majority were related to breast imaging [5].
A Dutch study had similar findings and stated that missed breast cancer by the breast radiologist was the commonest cause of malpractice lawsuits [6].
A study in Germany [7] also showed that missed findings on radiography, mammography, and angiography were the commonest cause of a lawsuit leading to civil (30%) and criminal convictions (5.5%).
Different laws in different countries influence the radiology practice and the outcome of the litigations.
Malpractice laws
Medical malpractice is defined as a disregard for the guidelines to provide ethical and correct care to the patients. Medical negligence, on the other hand, is a failure to maintain certain standards [1].
In the United States, medical malpractice is under the authority of the states and not the federal government. It is the state which determines the rules leading to different rules in different states of the country [3]. In the United States, medical malpractice law comes under a general law called “tort law” which is a combination of legislative enactment and common law principles. It is derived from the English common law and is the basis of jurisprudence in the United States and other commonwealth countries [5].
In the United Kingdom jury trials are less common however, the legal handling of medical lawsuits is like the USA. The National Health System Litigation Authority (NHSLA) coordinates claims against radiologists in the British National Health System.
In European countries like Italy, malpractice lawsuit is not under a “tort law” but under civil and penal regulations. Tort actions are civil claims by the patient for actions of the doctor who commits the tortuous act that causes a loss or harm to the patient. Physicians and radiologists come under both civil as well as criminal persecution. In Germany, it is the mediation boards comprising of experts of the German Physicians’ Guild that handle such cases. German courts are stricter than the rest of Europe.
The general procedure is that the “plaintiff” must prove that they were in care of the physician being charged. The principle is that radiologists have an obligation to their patients.
Another important lawsuit is the proof of “the standard of care” applied or not applied by the radiologist. Standard of care is “the watchfulness, caution, and prudence that a reasonable person in the circumstances would exercise. Failure to meet the standard of care is called negligence.”
The next step is to provide evidence that the radiologist had provided substandard care and it caused the injury.
The expert witnesses chosen are also important and often decide the decision on the lawsuit. An expert witness experienced in the type of radiological exam or interventional procedure subject to the malpractice claim is very important. His role is of utmost importance as he replaces the judge's lack of radiological knowledge and thus is “the bridge” between medicine and law.
In India, radiologist are held responsible under the Consumer Protection Act in Civil suit consumer court. Doctors are considered ‘service providers’ and patients are considered ‘consumers’. This the civil remedy where compensation is sought as a relief. Case of Criminal Negligence is filed under Section 304A of the Indian Penal Code that deals with death due to negligent and rash act. Punishment is 2 years imprisonment or fine or both. Case against radiologists can also be registered in Medical Council to warn, suspend or revoke their license. In addition, radiologists also are responsible to not disclose the gender of the fetus under the Pre-natal Diagnostic Techniques (Regulation and Prevention of Misuse) Act (PNDT Act). This is a law enacted to prevent female feticide [38].
Protection from malpractice litigation
The easiest and best way is to follow the maximum possible standard of care, improve communication skills with patients, and get insured.
New York appeals court defines the standard of care as: The law requires a physician to possess the skill and learning which is possessed by the average member of the medical profession… and to apply that skill and learning with ordinary reasonable care. He is not liable for a mere error in judgment, provided he does what he thinks is best after a careful examination. He does not guarantee a good result [8, 9].
The guidelines published by the Radiological Society of North America (RSNA), American College of Radiology (ACR), European Society of Radiology (ESR), and other such reputed societies need to be strictly followed by the radiologist. Patient checklists for interventions need to be completed before and after all procedures. Standardized training and continued medical education need to be undertaken by the radiologist to keep him up to date with the latest guidelines and standards of care. Also, the radiologist should always ask for help or refer the physician to another colleague if he has any doubts while performing a diagnostic or interventional procedure.
Preventing miscommunications
Whang et al. [3] state that communication failure was a frequent cause of radiology lawsuits. Failure to suggest additional investigations was the next common cause.
The main types of communication with the patient that can get the radiologist into trouble are conveying bad news, informed consent, and admitting medical errors. All information as to the purpose and nature of the intervention as well as its consequences and risks should be provided to the patient. After that written informed consent should be taken with the patient given the freedom to withdraw consent at any time. Consent cannot be taken from a minor or mentally disabled adult. A legally adequate informed consent is one in which the right information is provided to the patient so that they can take an independent decision. An understandable language should be used to make sure the patient agrees with its outcome despite knowing all the risks.
Regarding giving bad news to the patient the radiologist often focuses on technical terms placing little importance on the emotional factors of the patient, his values, and wishes. Physicians are not perfect at presenting information correctly many times. The patient should be given full explanation regarding the procedural complexity and its limits before explaining the reason for the error. Body language displaying empathy is also very important.
Another significant matter is the communication with referring physicians and colleagues. A correct formal report plays a significant part in this. Apart from the structure of the report, it is very important to proofread the report to avoid typing errors or dictaphone errors. As per the American College of Radiology, a radiologist’s report should include demographics, gender, clinical information, clinical issues, comparison studies, limitations, findings, and overall impression [10]. Abbreviations should be avoided. Non-standard abbreviations should never be used. Numeric dating should be avoided as it can confuse. For example, “10/6” means October 6 in the United States but may mean 10 June elsewhere. Pertinent negatives should be included in the report [11]. For example, fracture findings should also talk about callus formation and intra-articular extension. Hedge vocabulary should be avoided. Some of the examples include apparent, obvious, possible, borderline, doubtful, suspected, indeterminate, gross, no significant, probable, nonspecific, equivocal, and vague. Quantitative adjectives like small, tiny, moderate, gross, severe, and add prominently should be avoided [12]. Ideally, the top differential diagnosis should be listed in the impression and then the most likely one should be highlighted. Appropriate follow-up recommendations should be included at the end of the report. The use of disclaimers is not protective in litigation [13,14,15,16,17,18,19,20]. An error during reporting resulting in patient injury can lead to a legal battle despite using disclaimers. For example, the disclaimer “5%–10% of cases of fractures are missed on radiographs” leads to questions such as “How did you arrive at the 5%–10% range?” and “Have there been any studies at your hospital to see if your target population matches the study sample population?” Still, disclaimers are helpful in certain situations; for example, if a clinician orders a fetal congenital anomaly scan, it may be helpful to point out in the report that not every imaging study can identify all congenital anomalies. Phrases describing the suboptimal nature of the study should include not only the reason for the suboptimal nature of the study but also how much it leads to incomplete interpretation. It is also significant to mention how to rectify the suboptimal images and repeat studies should be advised if the region of interest is involved. An addendum is a revision made to a previous report and should include the date, time, and signature of the radiologist making the addendum. It should begin with the statement “This addendum supersedes the prior report dated [date].” The radiologist who created the initial report should ideally dictate the addendum. In his absence, the addendum can be provided by another radiologist. If another radiologist is taking ownership of the report, then he should ideally rewrite the entire report in his own language rather than just creating an addendum. If interpretation or re-interpretation of an old study is requested, then the radiologist should specify the same in the initial part of the report. Re-communication of the important findings is still required to the referring physician or patient despite the study being old [15, 21,22,23,24,25,26,27]. In case of a complex report, the radiologist should consult colleagues for a second look. The name of the colleague and the references should be included in the report. Sometimes radiology reports should be tailored according to the target audience. Simple language should be used whenever possible however medical terminology should be strictly followed.
Any conversation in person or by telephone with the referring doctor should be properly documented. Confidentiality is another topic that needs to be taken seriously by the radiologist, especially when dispatching reports outside the hospital. Patients’ images should be anonymized if they are used for teaching or research purposes [28,29,30,31,32,33,34]. Digital privacy should be given at most importance due to the easy nature of these data being transferred. A digital signature, authentication, and encryption it’s mandatory for all online data regarding the patient.
Liability insurance
Various malpractice policies exist in different countries. The radiologist who signs a contract with the insurance company should read every contract carefully before giving his consent. There are two types of liability insurance available: occurrence and claim made.
A professional liability insurance policy only covers claims of malpractice reported during the policy period, irrespective of when the medical service was administered. If a lawsuit is filed after the expiry date of the policy, then the policy will not pay for the lawsuit unless an extra premium is paid for “tail coverage”.
“Occurrence” basis means that policy covers claims of alleged malpractice that occurred during the policy period, irrespective of when the lawsuit was filed. In most of the cases insurance does not cover the criminal prosecution. The radiologist should consider very carefully the insurance carrier he chooses and the amount of malpractice coverage he pays for in his premium. The insurance application should be read thoroughly and accurately. A copy of the insurance coverage should always be kept by the insured radiologist. All terms of coverage or exclusion should be verified before signing the insurance policy document [35,36,37].
Role of AI in decreasing malpractice in radiology
Artificial intelligence can reduce the time radiologist have to spend on easy cases allowing them more time to concentrate on the complex cases that demand more attention. This not only increases the speed of the radiologist but also increases his accuracy for complex cases. Artificial intelligence can also act as a safety net by indicating areas that have been missed by the radiologist. It can also increase the confidence level by confirming the abnormal findings reported by the radiologist. It has also been found that the jurors that judge the medico-legal cases are more in favor of those radiologist who have utilized artificial intelligence-based tools to double check their reports. Also, contrary to common perception patients are less averse to radiologist who have utilized artificial intelligence to check their report.
Jonathan L. Mezrich, MD, a radiologist at Yale University School of Medicine’s Department of Radiology and Biomedical Imaging in New Haven, Conn., noted: “Keep up to date on and use available technology. If a finding is easily located with the aid of computer-aided detection or dual-energy sequences and your facility has access to those, not using this technology may be hard to sell to a jury [39].”
Conclusions
Radiology is increasingly getting involved in patient management and thus in the “duty of care”. Increasing scrutiny for medical errors is also becoming increasingly common in many countries. Knowledge about the main medico-legal issues and insurance in the radiology field is very important for the radiologist to protect himself from malpractice litigation.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Berlin L (2007) Radiologic errors and malpractice: a blurry distinction. AJR 189:517–522
Cannavale A, Santoni M, Mancarella P, Passariello R, Arbarello P (2013) Malpractice in radiology: what should you worry about? Radiol Res Pract 2013:219259
Whang JS, Baker SR, Patel R, Luk L, Castro A III (2013) The causes of medical malpractice suits against radiologists in the United States. Radiology 266:548–554
Fileni A, Magnavita N (2006) A 12-year follow-up study of malpractice claims against radiologists in Italy. Radiologia Medica 111:1009–1022
Halpin SFS (2009) Medico-legal claims against English radiologists: 1995–2006. Br J Radiol 82(982–988):2009
van Breast Smallenburg V, Setz-Pels W, Groenewoud JH (2012) Malpractice claims following screening mammography in the Netherlands. Int J Cancer 131:1360–1366
Tomczak R, Schnabel S, Ulrich P, Brambs HJ, Rilinger N, Niehoff C (2006) Frequency and causes of civil and criminal proceedings in radiology. Anal Surv Radiol 46:557–566
MacKinzie v Carman (1905) NYS 92:1063–1067
Eisenberg RL, Berlin L (2002) When does malpractice become manslaughter? AJR 179:331–335
ACR practice guideline for communication of diagnostic imaging findings (2010) ACR. http://www.acr.org/∼/media/C5D1443C9EA4424AA12477D1AD1D927D.pdf. Accessed 20 Feb 2014
Physicians’ weekly website (2016) Understanding damages in a medical malpractice case. www.physiciansweekly.com/understanding-damages-in-a-medical-malpractice-case/. Accessed 4 March 2019
Crisler RS (2006) The burden of proof in medical liability cases: a preponderance of the evidence. https://www.datatrace.com/media/wysiwyg/pdf/AAOS_Review.pdf. Accessed 29 Jan 2023
Raskin MM (2006) Survival strategies for radiology: some practical tips on how to reduce the risk of being sued and losing. J Am Coll Radiol 3:689–693
Clauss ER, Siglock TJ (1994) The fundamentals of avoiding and winning medical malpractice suits. Otolaryngol Head Neck Surg 110:141–145
Berlin L (1999) Admitting mistakes. AJR 172:879–884
Berlin L (2011) Liability for typographical errors. AJR 196:W215–W215
American College of Radiology (2001) ACR practice parameter for communication of diagnostic imaging findings. www.acr.org/-/media/ACR/Files/Practice-Parameters/CommunicationDiag.pdf. Accessed 25 July 2018
Panting G (2004) How to avoid being sued in clinical practice. Postgrad Med J 80:165–168
Berlin L (2000) Pitfalls of the vague radiology report. Am J Roentgenol 174:1511–1518
Mirvis S (2016) Let’s trim those overgrown hedges. Appl Radiol 45(6):8
Hoang JK (2017) Do not hedge when there is a certainty. J Am Coll Radiol 14:5
Ackerman BG (2018) You had me at “I’m sorry”: the impact of physicians’ apologies on medical malpractice litigation. www.natlawreview.com/article/you-had-me-i-m-sorry-impact-physicians-apologies-medical-malpractice-litigation. Accessed 11 Feb 2019
AMA Council on Ethical and Judicial Affairs (2011) Virtual mentor 13:626–628
Joint Commission on the Accreditation of Healthcare Organizations (2005) Hospital accreditation standards: standard RI.2.90. Oak Brook
Robbennolt JK (2009) Apologies and medical error. Clin Orthop Relat Res 467:376–382
Saitta N, Hodge SD Jr (2012) Efficacy of a physician’s words of empathy: an overview of state apology laws. J Am Osteopath Assoc 112:302–306
Roberts RG (2017) The art of the apology: when and how to seek forgiveness. Fam Pract Manag 14:44–49
Legant P (2011) Physician apologies for adverse outcomes: beware the minefields of mea culpa. J Oncol Pract 7:393–394
Berlin L (2018) I made a diagnostic error: should I apologize for it or ignore it? AJR 210:W180–W181
Mezrich JL (2019) Sometimes less is more: data acquisition and its impact on liability. Clin Imaging 53:v–vi
Berlin L (2017) Should CT and MRI scout images be interpreted? AJR 209:W43
Hanna TN, Lamoureux C, Krupinski EA, Weber S, Johnson JO (2018) Effect of shift, schedule, and volume on interpretive accuracy: a retrospective analysis of 2.9 million radiologic examinations. Radiology 287:205–212
Berlin L (2018) Contemporary risk management for radiologists. Radiographics 38:1717–1728
Mezrich JL (2012) Legal perspective: surgeons and im-aging—are self-reads a mistake? Am J Surg 204:545–547
Johnson PT, Scott WW, Gayler BW, Lewin JS, Fishman EK (2014) The CT scout view: does it need to be routinely reviewed as part of the CT interpretation? AJR 202:1256–1263
Coxon J, Rees J. Avoiding medical errors in general practice (2019) Trends in Urology and Mens’ www.trendsinmenshealth.com/article/avoiding-medical-errors-in-general-practice/. Accessed 19 May 2019
Drew T, Võ ML, Wolfe JM (2013) The invisible gorilla strikes again: sustained inattentional blindness in expert observers. Psychol Sci 24:1848–1853
Singh SS, Jayaram N (2015) Medico-legal issues in radiology: Indian context. J Med Soc 29:129–134
Tumbeva N (2021) Can AI help reduce malpractice risks for breast radiologists? MammoScreen. https://www.mammoscreen.com/can-ai-reduce-malpractice-risks
Acknowledgments
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
SSB and SB analyzed and interpreted the data. HG was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Biswas, S., Biswas, S., Awal, S.S. et al. Malpractice and lawsuits in radiology: what the radiologist should know. Egypt J Radiol Nucl Med 54, 19 (2023). https://doi.org/10.1186/s43055-023-00971-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-00971-9