Abstract
Objective
To investigate the structural brain abnormalities and their diagnostic accuracy through qualitative and quantitative analysis in term born and very preterm birth or with very low birth weight (VP/VLBW) adults.
Methods
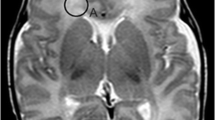
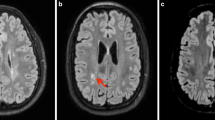
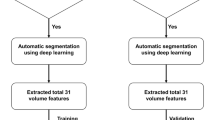
We analyzed 3-T MRIs acquired in 2011–2013 from 67 adults (27 term born controls, mean age 26.4 years, 8 females; 40 VP/VLBWs, mean age 26.6 years, 16 females). We compared automatic segmentations of the white matter, deep gray matter and cortical gray matter, manual corpus callosum measurements and visual ratings of the ventricles and white matter with t tests, logistic regression, and receiver operator characteristic (ROC) curves.
Results
Automatic segmentation correctly classified 84% of cases; visual ratings correctly classified 63%. Quantitative volumetry based on automatic segmentation revealed higher ventricular volume, lower posterior corpus callosum, and deep gray matter volumes in VP/VLBW subjects compared to controls (p < 0.01). Visual rating and manual measurement revealed a thinner corpus callosum in VP/VLBW adults (p = 0.04) and deformed lateral ventricles (p = 0.03) and tendency towards more “dirty” white matter (p = 0.06). Automatic/manual measures combined with visual ratings correctly classified 87% of cases. Stepwise logistic regression identified three independent features that correctly classify 81% of cases: ventricular volume, deep gray matter volume, and white matter aspect.
Conclusion
Enlarged and deformed lateral ventricles, thinner corpus callosum, and “dirty” white matter are prevalent in preterm born adults. Their visual evaluation has low diagnostic accuracy. Automatic volume quantification is more accurate but time consuming. It may be useful to ask for prematurity before initiating further diagnostics in subjects with these alterations.
Key Points
• Our study confirms prior reports showing that structural brain abnormalities related to preterm birth persist into adulthood.
• In the clinical practice, if large and deformed lateral ventricles, small and thin corpus callosum, and “dirty” white matter are visible on MRI, ask for prematurity before considering other diagnoses.
• Although prevalent, visual findings have low accuracy; adding automatic segmentation of lateral ventricles and deep gray matter nuclei improves the diagnostic accuracy.



Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- FLAIR:
-
Fluid attenuated inversion recovery
- PACS:
-
Picture archiving and communication system
- ROC:
-
Receiver operator characteristic
- T1- or T2-w:
-
T1- or T2-weighted
- VP/VLBW:
-
Very preterm birth or very low birth weight
References
Blencowe H, Cousens S, Oestergaard MZ et al (2012) National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379:2162–2172. https://doi.org/10.1016/S0140-6736(12)60820-4
Murphy M, McLoughlin G (2015) Born too soon: preterm birth in Europe trends, causes and prevention. Entre Nous:10–12
Zeitlin J, Szamotulska K, Drewniak N et al (2013) Preterm birth time trends in Europe: a study of 19 countries. BJOG 120:1356–1365. https://doi.org/10.1111/1471-0528.12281
Martin JA, Hamilton BE, Ph D et al (2017) Births: final data for 2015. Natl Vital Stat Rep 66
Delnord M, Blondel B, Zeitlin J (2015) What contributes to disparities in the preterm birth rate in European countries? Curr Opin Obstet Gynecol 27:133–142. https://doi.org/10.1097/GCO.0000000000000156
Saigal S, Doyle LW (2008) An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 371:261–269. https://doi.org/10.1016/S0140-6736(08)60136-1
Allin M, Rooney M, Griffiths T et al (2006) Neurological abnormalities in young adults born preterm. J Neurol Neurosurg Psychiatry 77:495–499. https://doi.org/10.1136/jnnp.2005.075465
Anderson PJ (2014) Neuropsychological outcomes of children born very preterm. Semin Fetal Neonatal Med 19:90–96. https://doi.org/10.1016/j.siny.2013.11.012
Baron IS, Rey-Casserly C (2010) Extremely preterm birth outcome: a review of four decades of cognitive research. Neuropsychol Rev 20:430–452. https://doi.org/10.1007/s11065-010-9132-z
Crump C, Sundquist K, Sundquist J, Winkleby MA (2011) Gestational age at birth and mortality in young adulthood. JAMA 306:1233–1240. https://doi.org/10.1001/jama.2011.1331
Lawn JE, Blencowe H, Oza S et al (2014) Every newborn: progress, priorities, and potential beyond survival. Lancet 384:189–205. https://doi.org/10.1016/S0140-6736(14)60496-7
Hack M, Flannery DJ, Schluchter M et al (2002) Outcomes in young adulthood for very-low-birth-weight infants. N Engl J Med 346:149–157. https://doi.org/10.1056/NEJMoa010856
Rees S, Inder T (2005) Fetal and neonatal origins of altered brain development. Early Hum Dev 81:753–761. https://doi.org/10.1016/j.earlhumdev.2005.07.004
Bäuml JG, Daamen M, Meng C et al (2014) Correspondence between aberrant intrinsic network connectivity and gray-matter volume in the ventral brain of preterm born adults. Cereb Cortex. https://doi.org/10.1093/cercor/bhu133
Mathur AM, Neil JJ, Inder TE (2010) Understanding brain injury and neurodevelopmental disabilities in the preterm infant: the evolving role of advanced magnetic resonance imaging. Semin Perinatol 34:57–66. https://doi.org/10.1053/j.semperi.2009.10.006
Ment LR, Hirtz D, Hüppi PS (2009) Imaging biomarkers of outcome in the developing preterm brain. Lancet Neurol 8:1042–1055. https://doi.org/10.1016/S1474-4422(09)70257-1
Glass HC, Bonifacio SL, Peloquin S et al (2010) Neurocritical care for neonates. Neurocrit Care 12:421–429. https://doi.org/10.1007/s12028-009-9324-7
Barkovich AJ, Raybaud C (2012) Pediatric neuroimaging. Wolters Kluwer Health, Philadelphia
Cheong JLY, Thompson DK, Wang HX et al (2009) Abnormal white matter signal on MR imaging is related to abnormal tissue microstructure. AJNR Am J Neuroradiol 30:623–628. https://doi.org/10.3174/ajnr.A1399
Dubois J, Hu PS, Hüppi PS, Dubois J (2006) Diffusion tensor imaging of brain development. Semin Fetal Neonatal Med 11:489–497. https://doi.org/10.1016/j.siny.2006.07.006
Rutherford MA, Supramaniam V, Ederies A et al (2010) Magnetic resonance imaging of white matter diseases of prematurity. Neuroradiology 52:505–521. https://doi.org/10.1007/s00234-010-0700-y
Degnan AJ, Wisnowski JL, Choi S et al (2015) Alterations of resting state networks and structural connectivity in relation to the prefrontal and anterior cingulate cortices in late prematurity. Neuroreport 26:22–26. https://doi.org/10.1097/WNR.0000000000000296
Volpe JJ (2009) The encephalopathy of prematurity–brain injury and impaired brain development inextricably intertwined. Semin Pediatr Neurol 16:167–178. https://doi.org/10.1016/j.spen.2009.09.005
Basten M, Jaekel J, Johnson S et al (2015) Preterm birth and adult wealth: mathematics skills count. Psychol Sci 26:1608–1619. https://doi.org/10.1177/0956797615596230
Eryigit Madzwamuse S, Baumann N, Jaekel J et al (2014) Neuro-cognitive performance of very preterm or very low birth weight adults at 26 years. J Child Psychol Psychiatry n/a–n/a. https://doi.org/10.1111/jcpp.12358
Greene MF (2002) Outcomes of very low birth weight in young adults. N Engl J Med 346:146–148. https://doi.org/10.1056/NEJM200201173460302
Baumann N, Bartmann P, Wolke D (2016) Health-related quality of life into adulthood after very preterm birth. Pediatrics 137. https://doi.org/10.1542/peds.2015-3148
Aukland SM, Elgen IB, Odberg MD et al (2014) Ventricular dilatation in ex-prematures: only confined to the occipital region? MRI-based normative standards for 19-year-old ex-prematures without major handicaps. Acta Radiol 55:470–477. https://doi.org/10.1177/0284185113497476
Bjuland KJ, Rimol LM, Løhaugen GCC, Skranes J (2014) Brain volumes and cognitive function in very-low-birth-weight (VLBW) young adults. Eur J Paediatr Neurol 18:578–590. https://doi.org/10.1016/j.ejpn.2014.04.004
Nosarti C, Woo K, Walshe M et al (2014) Preterm birth and structural brain alterations in early adulthood. Neuroimage Clin 6:180–191. https://doi.org/10.1016/j.nicl.2014.08.005
Odberg MD, Aukland SM, Rosendahl K, Elgen IB (2010) Cerebral MRI and cognition in nonhandicapped, low birth weight adults. Pediatr Neurol 43:258–262. https://doi.org/10.1016/j.pediatrneurol.2010.05.014
Breeman LD, Jaekel J, Baumann N et al (2017) Neonatal predictors of cognitive ability in adults born very preterm: a prospective cohort study. Dev Med Child Neurol 59:477–483. https://doi.org/10.1111/dmcn.13380
Daamen M, Bäuml JG, Scheef L et al (2015) Neural correlates of executive attention in adults born very preterm. Neuroimage Clin 9:581–591. https://doi.org/10.1016/j.nicl.2015.09.002
Jurcoane A, Daamen M, Scheef L et al (2016) White matter alterations of the corticospinal tract in adults born very preterm and/or with very low birth weight. Hum Brain Mapp 37:289–299. https://doi.org/10.1002/hbm.23031
Riegel K, Ohrt B, Wolke D, Österlund K (1995) Die Entwicklung gefährdet geborener Kinder bis zum fünften Lebensjahr. (The development of at-risk children until the fifth year of life. The Arvo Ylppö longitudinal study in South Bavaria and South Finland). Ferdinand Enke Verlag, Stuttgart
Wolke D, Meyer R (1999) Cognitive status, language attainment, and prereading skills of 6-year-old very preterm children and their peers: the Bavarian Longitudinal Study. Dev Med Child Neurol 41:94–109
Aster M von, Wechsler D (2009) Wechsler-Intelligenztest für Erwachsene : WIE ; Manual ; Übersetzung und Adaptation der WAIS-III von David Wechsler, 2., korr. Aufl. Pearson Assessment & Information, Frankfurt/M
Tschampa HJ, Urbach H, Malter M et al (2015) Magnetic resonance imaging of focal cortical dysplasia: comparison of 3D and 2D fluid attenuated inversion recovery sequences at 3T. Epilepsy Res 116:8–14. https://doi.org/10.1016/j.eplepsyres.2015.07.004
Jenkinson M, Beckmann CF, Behrens TEJ et al (2012) FSL. Neuroimage 62:782–790. https://doi.org/10.1016/j.neuroimage.2011.09.015
Ge Y, Grossman RI, Babb JS et al (2003) Dirty-appearing white matter in multiple sclerosis: volumetric MR imaging and magnetization transfer ratio histogram analysis. AJNR Am J Neuroradiol 24:1935–1940
Rothman KJ, Greenland S, Lash TL (2008) Modern epidemiology, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
Efron B, Tibshirani R (1993) An introduction to the bootstrap. Chapman & Hall, New York
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol 57:289–300
Pandit AS, Ball G, Edwards AD, Counsell SJ (2013) Diffusion magnetic resonance imaging in preterm brain injury. Neuroradiology 55:65–95. https://doi.org/10.1007/s00234-013-1242-x
Feldman HM, Lee ES, Loe IM et al (2012) White matter microstructure on diffusion tensor imaging is associated with conventional magnetic resonance imaging findings and cognitive function in adolescents born preterm. Dev Med Child Neurol 54:809–814. https://doi.org/10.1111/j.1469-8749.2012.04378.x
Stewart AL, Rifkin L, Amess PN et al (1999) Brain structure and neurocognitive and behavioural function in adolescents who were born very preterm. Lancet 353:1653–1657
Griffiths ST, Elgen IB, Chong WK et al (2013) Cerebral magnetic resonance imaging findings in children born extremely preterm, very preterm, and at term. Pediatr Neurol 49:113–118. https://doi.org/10.1016/j.pediatrneurol.2013.03.006
Ifflaender S, Rüdiger M, Konstantelos D et al (2013) Prevalence of head deformities in preterm infants at term equivalent age. Early Hum Dev 89:1041–1047. https://doi.org/10.1016/j.earlhumdev.2013.08.011
Melbourne L, Murnick J, Chang T et al (2015) Regional brain biometrics at term-equivalent age and developmental outcome in extremely low-birth-weight infants. Am J Perinatol 32:1177–1184. https://doi.org/10.1055/s-0035-1552936
Meng C, Bäuml JG, Daamen M et al (2015) Extensive and interrelated subcortical white and gray matter alterations in preterm-born adults. Brain Struct Funct. https://doi.org/10.1007/s00429-015-1032-9
Nosarti C, Giouroukou E, Healy E et al (2008) Grey and white matter distribution in very preterm adolescents mediates neurodevelopmental outcome. Brain 131:205–217. https://doi.org/10.1093/brain/awm282
Giger ML (2018) Machine learning in medical imaging. J Am Coll Radiol. https://doi.org/10.1016/j.jacr.2017.12.028
Acknowledgements
We thank all current and former Bavarian Longitudinal Study Group members who contributed to study organization, recruitment, data collection, management, and analyses, including (in alphabetical order) Stephan Czeschka, Claudia Grünzinger, Julia Jaekel, Christian Koch, Diana Kurze, Sonja Perk, Andrea Schreier, Antje Strasser, Julia Trummer, and Eva van Rossum. Most importantly, we thank all the study participants for their efforts to take part in this study.
Funding
This study has received funding from the German Federal Ministry of Education and Science (BMBF 01ER0801 to PB and DW, BMBF 01EV0710 to AMW, BMBF 01ER0803 to CS) and the Kommission für Klinische Forschung, Technische Universität München (KKF 8765162 to CS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Alina Jurcoane.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors, GL, has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
The Ethics Committee at the University Hospital Bonn approved the study.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in several articles (https://www.ncbi.nlm.nih.gov/pubmed/?term=bartmann+wolke+mri). These were on topics of functional MRI, diffusion tensor imaging or behavioral measures; the current article is the only publication with neuroradiological focus.
Methodology
• prospective
• cross-sectional study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Milka Marinova and Elke Hattingen share authorship.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Jurcoane, A., Daamen, M., Keil, V.C. et al. Automated quantitative evaluation of brain MRI may be more accurate for discriminating preterm born adults. Eur Radiol 29, 3533–3542 (2019). https://doi.org/10.1007/s00330-019-06099-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06099-7