Abstract
Background
To describe the concept, implementation, patient characteristics, and preliminary outcomes of a Neonatal Neurocritical Care Service (NNCS) recently established at the University of California, San Francisco.
Methods
The NNCS was developed to better address the special needs of neonates at risk for neurological injury. The service combines dedicated neurological care, specialized neonatal medical and nursing expertise, neuromonitoring, neuroimaging, neurodevelopmental care, and long-term follow up. Newborns evaluated by the NNCS between July 2008 and June 2009 were included in the analysis. Demographic data (gestational age at birth, sex, admission diagnosis, and reason for consult), outcome (mortality, length of stay), and neurophysiology and imaging resources were extracted from patient charts.
Results
Over the 12-month period, 155 newborns were evaluated (approximately 25% of all admissions); of these, 51 were preterm (<36 weeks gestation) and 104 were term. Approximately half were admitted for primary medical diagnoses, such as preterm birth, congenital malformations or apnea/apparent life-threatening event (ALTE), with the remainder admitted for primary neurological problems, including perinatal asphyxia, seizures/possible seizures, or congenital cerebral malformation. The most common neurological diagnoses were hypoxic-ischemic encephalopathy (38%) and seizure (35%). Among preterm newborns, intraventricular hemorrhage grade III and periventricular hemorrhagic infarction were most common. Mortality was approximately 20% in both preterm and term populations.
Conclusions
While specialized neurocritical care has improved outcomes in adult populations, longitudinal studies are needed to determine whether specialized neurocritical care services will also result in improved neurodevelopmental outcomes for newborns.
Similar content being viewed by others
Introduction
Neurocritical care is a growing multidisciplinary subspecialty that combines expertise in intensive care, neurology, neurosurgery, and neuroradiology. Recent advances in adult neurocritical care include continuous multimodal monitoring, recombinant tissue plasminogen activator (TPA) for acute stroke, hypothermia for neuroprotection after cardiac arrest, and therapy for vascular malformations [1–5]. In 2002, the Neurocritical Care Society was established with the mission “to improve outcomes for patients with life-threatening neurological illnesses.” In 2007, the Accreditation Council for Graduate Medical Education (ACGME) gave the first certification examination, and as of May 2009 there were 40 accredited programs in the United States. Currently, several national guidelines or practice parameters pertinent to adult neurocritical care have been adopted [6–8]. Early evidence suggests that specialized neurocritical care units can improve outcomes following stroke, trauma, and subarachnoid hemorrhage [9–13]. Because of advances in monitoring and therapy, as well as accumulating evidence of improved outcomes, there is increasing acceptance of adult neurocritical care as a distinct subspecialty [14, 15].
Like adult neurocritical care, dedicated pediatric neurocritical care is emerging as a distinct subspecialty. The Department of Neurology at Children’s Hospital Boston is the first to provide a dedicated training program in pediatric neurocritical care [16]. Bell et al. recently described the initial effort to establish a Pediatric Neurocritical Care (PNCCM) service at the Children’s National Medical Center in Washington D.C. [17], a model which Bell subsequently brought to Children’s Hospital of Pittsburgh, where they have trained 18 fellows in Pediatric Neurocritical Care since 2000. While there are fewer evidence-based guidelines in pediatric neurocritical care, and no evidence yet that this type of specialization will improve outcomes, the latter papers argue that expertise in pediatric neurocritical care will provide an essential foundation for improved education and research.
Neonatal intensive care nurseries (or ICNs) were initially developed as specialized units to provide improved temperature support and feeding for at-risk newborns. An important feature was low nurse-to-patient ratios, and training for nurses, with special emphasis on the unique problems experienced by newborns. As with adults, improved cardiopulmonary care has led to increased survival following preterm birth and critical neonatal illnesses. Neurological morbidity remains high, however, with increased risk of motor and cognitive disability in newborns with neurological illnesses [18–20].
Recent advances in diagnosis and treatment of neurological illnesses seen in the ICN suggest that the need for dedicated expertise in newborn neurocritical care equals that for adults and children. For example, therapeutic hypothermia may reduce morbidity and mortality in newborns with hypoxic-ischemic encephalopathy (HIE) [21–25]. Advances in brain monitoring, including digital video-electroencephalogram (EEG) and amplitude-integrated EEG (aEEG) allow real-time monitoring of cerebral function [26, 27]. Progress in magnetic resonance imaging (MRI) and transport of newborns for imaging has allowed detailed anatomical evaluation of brain injury and developmental abnormalities [28].
In 2007, specialists in neonatology, neurology, neuroradiology, and neurodevelopmental care at the University of California at San Francisco (UCSF) came together to create an interdisciplinary Neonatal Neurocritical Care Service (NNCS) to address the perceived need for more specialized neurological monitoring and support in the ICN setting. This is a specialized service within the closed unit ICN, which provides dedicated neurology care, specialized nursing, intensive monitoring, and standardized management guidelines for newborns with congenital or acquired neurological conditions. This report describes the structure of specialized neurocritical care for neonates by evaluating the volume, patient demographics, underlying neurological conditions, and resource utilization during the first 12 months of operation.
Materials and Methods
Development of a Neonatal Neurocritical Care Service
In 2007, members of the Departments of Pediatrics and Neurology at UCSF developed a plan for a dedicated service to provide specialized care for newborns with neurological conditions. The mission and ultimate goal of the NNCS is to improve neurodevelopmental outcomes in newborns at risk of neurological disability. The approach is multi-disciplinary, and includes a dedicated pediatric neurology service, specialized neonatal medical and nursing expertise, neuromonitoring, neuroimaging, neurosurgery, neurodevelopmental care (including Newborn Individualized Developmental Care and Assessment Program, NIDCAP), and infant follow up. The service cares for all newborns admitted to the ICN with primary neurological or neurosurgical conditions at the time of admission to the ICN, or neurological complications as a result of their primary admitting diagnosis.
Newborns cared for by the NNCS are admitted to the ICN at UCSF, with access to medical intensive care such as extracorporeal membrane oxygenation (ECMO). Once a child is identified as having a neurological condition, the dedicated neurologist is notified and the child is assigned to a neonatal nurse with specialized neurological intensive care training.
The NNCS team consists of an attending neonatologist, an attending pediatric neurologist, specialized bedside nurse, and housestaff and neonatal nurse practitioners in neonatology and neurology. The NNCS team members round at least daily to co-manage newborns with acute neurological conditions. The neonatology attending is responsible for the primary clinical care of the newborns. The neurologist is responsible for management of acute neurological issues (i.e., HIE, seizures) from the time of admission, and other neurological illnesses or brain injury as identified in children with primary medical conditions. The attending pediatric neurologist helps to identify patients at risk for neurological sequelae (i.e., evaluating encephalopathy in newborns with asphyxia), monitor newborns at high risk for seizures, diagnose and manage seizures and status epilepticus, request and interpret imaging and other investigations, provide prognosis, and ongoing, frequent, counseling to family members. Neurosurgeons are consulted when appropriate. Children with acute neurological illnesses are assigned to a bedside nurse with specialized neurological intensive care training. At UCSF, all neonatologists and pediatric neurologists attend on the neurocritical care service; however, a smaller self-identified group of neurologists provides the majority of care.
A working group consisting of neurologists, neonatologists, and nursing staff have developed institution-specific guidelines for: (i) hypothermia therapy for newborns with HIE (including initial outborn management and transport management for initiation of cooling prior to arrival at UCSF, as well as inborn management,); (ii) electroencephalogram (EEG) and aEEG monitoring, and (iii) seizure therapy.
The working group has also implemented an educational program that consists of core curriculum training and competencies for dedicated nursing staff, outreach to referral centers, monthly housestaff lectures, quarterly case review, and dedicated time for members of the Division of Neonatology to review cases and discuss controversial issues.
Data Collection
Following approval from the Committee for Human Research at UCSF, demographic and mortality data for all admissions to the ICN were extracted from the Division of Neonatology database for the time period June 2008 to May 2009. Hospital medical records were used to extract data for all patients evaluated by the NNCS during its first year of operation (July 1, 2008 to June 30, 2009). Clinical data included date of birth, gestational age at birth, date of admission, and timing of consult relative to the ICN admission. Primary diagnoses and reason for evaluation by the NNCS were determined from the admitting and discharge summaries, as well as from the consult notes. The primary diagnosis was defined as the main condition leading to the admission to the ICN. We further collected outcome data, including length of stay and mortality. Finally, we noted the resources utilized to diagnose and manage neurological conditions, including neurosurgical consult, neuroimaging [cranial ultrasound, computed tomography (CT), MRI], electroencephalogram (EEG), including prolonged studies (>24 h), and aEEG.
Results
Basic Demographics
The NNCS evaluated 155 children over 1 year, which represented approximately one-quarter of newborns admitted to the ICN. The demographic data appear in Table 1.
Underlying Conditions, Acuity, and Mortality
The primary reason for intensive care varied widely (Table 2). Close to half of the patients had a primary medical condition as the reason for intensive care, while the remainder had a primary neurological condition. The most common medical reasons for admission were preterm birth (requiring respiratory and/or cardiac support), congenital malformation (non-cerebral), or apnea/apparent life-threatening event (ALTE). Perinatal asphyxia, seizures/possible seizures, and congenital cerebral malformations (including cerebral vascular malformations) were the most common neurological reasons for admission.
Overall, the group represented high acuity admissions, with long hospital stays and high mortality. The median length of stay was 14 days (range 1, 267), with longer stays for preterm newborns. Death prior to discharge occurred in 21% of those newborns evaluated by the NNCS, compared with 7% of all ICN admissions. The most common neurological conditions leading to death were intraventricular hemorrhage with periventricular hemorrhagic infarction (56% mortality), brain malformation (30% mortality), and HIE (25% mortality). In all but two cases, death occurred following redirection of care to comfort measures based on neurological prognosis alone (18 children), neurologic prognosis plus need for long-term complex medical or surgical care (12 children), or severe systemic illness without serious neurological complications (1 child). Two children died despite maximal intervention (one during embolization procedure for congenital cerebral vascular malformation and one with refractory hypotension and necrotizing enterocolitis).
Neurological Conditions
Reasons for evaluation by the NNCS were diverse (Table 3). The most common primary reasons for evaluation were: HIE/possible HIE (38%), seizures/possible seizures (25%), intracranial hemorrhage (10%), and brain malformation (10%). Abnormal neurological examination, abnormal imaging, encephalopathy, and dysmorphic syndrome were less common causes. Among the newborns with a primary medical reason for admission to the ICN, the most common reasons were seizures/possible seizures (34%), intracranial hemorrhage (20%), and hypotonia (10%).
Of the term newborns, 50% were evaluated by the first postnatal day of life (range 0, 62 days); preterm newborns were evaluated at a median age of 15 days of life (range 1,192 days). A pediatric neurologist evaluated the term newborns a median of five times (range 1, 18), a frequency that was similar for preterm infants.
The most common neurological diagnoses were HIE, seizure, brain malformation, and acquired brain injury (Table 4). Several newborns carried multiple neurological diagnoses. Thirteen newborns had normal neurological evaluations despite clinical concern for a neurological condition.
Therapeutic Hypothermia for Hypoxic-Ischemic Encephalopathy
Fifty-six babies were evaluated for therapeutic hypothermia therapy. Of these, 51 (91%) were referred from other centers or the UCSF Emergency Department (following home delivery). Forty-four newborns were treated for 72 h at 33.5°C using whole body cooling with the Blanketrol III™ (Cincinnati Sub-Zero Products, Cincinnati, OH) according to clinical entry criteria and a cooling protocol that is similar to that of Shankaran et al. [22]. Reasons for exclusion from the 72-h therapeutic hypothermia protocol included: late referral outside the 6-h time window (two infants), only mild HIE (three infants), or wrong diagnosis (one infant), leaving 50 appropriate referrals. Six infants were rewarmed prior to 72 h for worsening persistent pulmonary hypertension of the newborn, including three who required ECMO. A total of 14 newborns died as a result of profound hypoxic-ischemic injury.
Neuromonitoring and Neonatal Seizures
Newborns were monitored primarily for suspected seizures, as part of the therapeutic hypothermia protocol (72–96 h of monitoring using both bedside aEEG and continuous video-EEG), or to evaluate encephalopathy of unknown etiology. The bedside nurse and housestaff reviewed the aEEG every 2–3 h. The continuous video-EEG recordings were reviewed at least twice daily by the attending neurologist or neurophysiologist, or more often, as clinically indicated. Starting in early 2009, EEG recordings were accessible for real-time interpretation by an off-site neurologist via the internet.
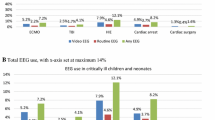
Overall, 106 children (68%) were monitored using conventional video-EEG (according to the international 10–20 system modified for neonates) and 101 (65%) were evaluated using aEEG (primarily using needle electrodes in a single-channel bi-parietal montage). Of the newborns monitored using video-EEG, 85% had prolonged or multiple recordings lasting longer than 24 h.
Thirty-nine newborns were evaluated primarily for a clinical event that was suspicious for seizure. Of these 23 (59%) were >36 weeks gestation at birth. Thirty-six (92%) were evaluated using video-EEG and 28 (72%) using aEEG (three newborns were felt not to have seizures based on clinical features of posturing or jitteriness). Of the infants evaluated for possible seizures, 22 (56%) were felt to have had seizures by clinical and/or electrographic criteria, whereas the remainder were thought to have spells or aEEG events that were not consistent with seizure. In addition to the infants evaluated primarily for seizures, another 32 newborns were diagnosed with clinical and/or electrographic seizures during their ICN stay. In all, 54 newborns were diagnosed with seizures; 19 had clinical events with semiology and clinical course that was consistent with seizure prior to monitoring, but no subsequent seizures recorded once EEG monitoring was initiated (35%), 12 with only electrographic seizures (22%), and 23 with both clinical and electrographic seizures (43%). Of the newborns that were monitored with continuous EEG during therapeutic hypothermia, 52% had electrographic seizures and five had clinical events that were suspicious for seizure, but were without EEG correlate.
Resource Utilization/Neonatal Neuroimaging
Most of the newborns were imaged during their hospital stay using cranial ultrasonography via anterior and posterolateral fontanelles (112, 72%) and/or MRI (114, 74%). MRI studies included noncontrast morphologic imaging (volumetric T1-weighted spoiled gradient echo images and conventional or fast spin echo axial T2-weighted images), diffusion tensor imaging (with a b value of 700 s/mm2 and diffusion sensitization in a minimum of six directions), and single voxel proton MR spectroscopy localized to the basal ganglia and frontal white matter (PRESS technique with echo time of 288 ms). The total imaging time is approximately 45–60 min and the children are typically away from the ICN for 60–90 min. Newborns were imaged only when stable for transport to the imaging suite. For newborns with HIE, MRI was typically performed at 4–7 days of life. For other indications, the timing was variable and ranged from the first 48 h of life (e.g., for seizures and suspected stroke) to several weeks of life (e.g., as part of the evaluation of a syndromic infant). Of the newborns imaged with MRI, 39 studies (25%) were performed as part of a research protocol, including 31 term newborns with perinatal asphyxia and eight preterm newborns. Common abnormalities included findings seen in hypoxic-ischemic injury (15%), white matter injury (12%), developmental abnormality (13%), intracranial hemorrhage (8%), and stroke (5%). Only 21 (18%) had a normal imaging study (Table 5).
Only six infants (4%) were evaluated using CT. Neurosurgical evaluation was requested for 23 newborns (15%).
Follow-up
Of the surviving children (and excluding the 13 with normal evaluations), 86 (78%) were seen in one of the UCSF follow-up programs. A neurologist or rehabilitation specialist saw more than half of the children, and 60% were seen in the High Risk Infant Follow-Up Clinic. The follow-up rate for children evaluated for therapeutic hypothermia was 95%, for children with intraventricular hemorrhage 93%, for children with seizures 88%, and for children with stroke 86%.
Discussion
Neonatology as a field has grown tremendously over the last 50 years. Progress in treatment of vital organ systems such as lung and heart using surfactant, ventilation and ECMO have resulted in improved survival rates for children born at very early gestational ages or with critical illnesses due to infection, asphyxia, or congenital malformations [29–31]. Improvement in neurodevelopmental outcome, however, has not kept pace with improvement in survival.
There is increasing evidence from experimental animal and human clinical studies to suggest that the developing brain is unique in its response to injury, and that recovery is mediated by different mechanisms from those observed in adults. First, excitation predominates in the developing cerebral cortex and limbic structures, leading to a lower threshold for seizures and excitotoxic hypoxic/ischemic injury (reviewed in [32]). Second, the neonatal brain is selectively vulnerable to oxidative stress due to relatively high levels of free iron (reviewed in [33]). Third, inflammation plays a different role. Since the neonatal blood–brain barrier appears more resistant than its adult counterpart, microglia may be supportive rather than harmful, and cytokines may be different in their mediating effects (reviewed in [34]). Fourth, the perinatal period is unique in terms of neurogenesis, gliogenesis and circuit formation, all of which can be impacted by disease. Indeed, these differences appear to result in selective vulnerability of different cell populations through development (reviewed in [35]).
This emerging evidence, and our experience and observation suggest that neonatal neurocritical care is a distinct subspecialty that requires specialized physician and nurse training, and an approach that is different from both adult and pediatric neurocritical care. It is unique in its patient populations, need for neurology/neonatology co-management, nursing expertise, and specialized equipment.
Patient Population
Although both children and neonates requiring critical care have high rates of seizures and associated primary medical conditions, the latter do not have tumors or traumatic brain injury, differentiating them from the most common causes for neurological consultation in the pediatric ICU [17]. Even in the context of seizures, neurological management of newborns is unique: newer anticonvulsant agents have not been tested in this population and seizures remain very difficult to treat. Increasing evidence reveals the benefits of therapeutic hypothermia in neonates with HIE, one of the most common conditions. In addition, preterm newborns (who accounted for 1/3 of our population) are at very high risk of acquired brain injury and seizures at a time when they are undergoing critical brain development, and thus require specialized evaluation and follow up.
Neonatology/Neurology Co-Management
Our co-management model incorporating neonatologists and neurologists is optimal for patient care due to the high rates of primary medical conditions, as well as frequent multi-system disease and complex neurological problems present in our population. Multidisciplinary care has increased our ability to recognize high rates of clinically silent injury and seizures, as well as the effects of intensive medical care on brain function. A neonatologist is essential to provide multi-system critical care. However, in our nursery, the neurologists spend a significant amount of time at the bedside to assist with moment-to-moment management decisions for conditions such as HIE and seizures. Neurologists are required in these cases for EEG interpretation (especially given the high rate (22%) of newborns with electrographic seizures without clinical correlate) and to examine for signs of encephalopathy in an asphyxiated newborn. The neurology team also guides appropriate investigations for less common conditions such as brain malformations or isolated hypotonia, helps integrate results from specialized tests, and assists in the determination of prognosis in newborns with injury or underlying problems.
There is accumulating evidence from animal models and humans studies that seizures may harm the developing brain [36–40]. Early and accurate recognition of seizures through trained bedside nursing and continuous monitoring is important for managing appropriate therapy, and may ultimately lead to better outcomes in this high-risk population. Amplitude-integrated and full montage EEG provide complementary information about brain function [41–43] and technical expertise in application and interpretation that is available 24 h a day and 7 days a week is essential for detecting seizures and monitoring background function.
Finally, the MR examination for newborns is quite different from that of an older child or adult, as the neonatal brain has a different appearance (due to immature sulcation and myelination) and responds differently to injury than more mature brains. Therefore, a neuroradiologist with training and experience in MR, diffusion tensor, and spectroscopy imaging of the neonatal brain is required for interpretation of these studies in newborns.
Specialized Nursing Care
A high level of bedside and transport nursing expertise has been essential to the functioning of our service. For newborns with HIE, early treatment with hypothermia may be beneficial [25, 44, 45], supporting the need for trained teams to apply this therapy during transport to a referral center. Furthermore, specialized training in neonatal neurological intensive care is necessary to recognize seizures and address the potential complications seen in newborns treated with hypothermia.
Forty-nine of our 150 bedside nurses have participated in specialized education, which includes neurological examination skills, seizure recognition, aEEG application and basic interpretation, set-up and use of therapeutic hypothermia, and methods for safe transport for MRI. At UCSF, there are two NNCS-trained nurses in the intensive care nursery at all times.
Specialized Equipment and Technical Expertise
Specialized equipment and technical expertise are important for applying emerging neurotherapies, monitoring brain function, and detecting injury.
Therapeutic hypothermia appears to reduce death and disability in newborns with HIE [21–25]. Though this therapy has been achieved without specialized equipment in a low resource setting [46], most North American and European centers are using either whole body or selective head cooling with Blanketrol™, CoolCap™, or other specialized devices to achieve therapeutic hypothermia.
Studies by our group and others have found that MRI is superior to head ultrasound and CT for detecting the injuries seen most commonly in newborns, including white matter injury, findings seen in HIE, and developmental anomalies and malformations [28, 47–52]. Using MRI to better identify injury or developmental anomalies may help clinicians to identify those children who are most likely to benefit from early referral for interventional services such as physical and occupational therapy. Critically ill newborns can be safely transported for imaging using an MR-compatible isolette, ventilator, infusion pumps, and monitoring devices [53]. At UCSF, newborns are transported for imaging in an isolette designed for our research studies, a commercial MR-compatible isolette (Lammers Medical Technology, Luebeck, Germany) or in an open crib, and are accompanied by two nurses, a physician and, if intubated, a respiratory therapist. All personnel are trained both in neonatal critical care and in MR safety. The MR technologists have training and experience in imaging the neonatal brain.
Conclusions
Specialized neurocritical care has led to improved outcomes in adult populations. There has been recent interest in pediatric neurocritical care as a subspecialty that is separate from its adult counterpart. Our first year of experience providing dedicated neurological care in the ICN at UCSF suggests that neonatal neurocritical care is a sub-specialty that is distinct from both adult and pediatric neurocritical care.
We propose that newborns with neurologic illnesses should be cared for by a multi-disciplinary service consisting of neurologists, neonatologists and specialized nurses, and in a facility capable of providing specialized care as we have described. Because of high rates of co-morbidities, access to medical and surgical intensive care such as ECMO, and surgical subspecialties is essential. As such, optimal practice of neonatal neurocritical care would likely be restricted to regional neonatal care centers.
Improved brain monitoring and imaging have widened our field of view on the developing brain. It is our hope that dedicated neonatal neurocritical care, applied through a multidisciplinary team of trained personnel, using specialized equipment will lead to better neurodevelopmental outcomes, not merely better survival.
Longitudinal studies by our center and others to study novel neuroprotective agents and examine the efficacy of monitoring, impact of seizure therapy, usefulness of MRI as a surrogate marker, and cost effectiveness of these measures will be essential to determine whether the presence of specialized neurocritical care will result in improved neurodevelopmental outcomes for newborns.
References
The National of Institute Neurological Disorders, Stroke (NINDS) rt-PA Stroke Study Group. Effect of intravenous recombinant tissue plasminogen activator on ischemic stroke lesion size measured by computed tomography NINDS. Stroke. 2000;31(12):2912–9.
Clark WM, et al. The rtPA (alteplase) 0- to 6-hour acute stroke trial, part A (A0276g): results of a double-blind, placebo-controlled, multicenter study. Thromblytic therapy in acute ischemic stroke study investigators. Stroke. 2000;31(4):811–6.
The Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–56.
Bernard SA, Buist M. Induced hypothermia in critical care medicine: a review. Crit Care Med. 2003;31(7):2041–51.
Mazzeo AT, Bullock R. Monitoring brain tissue oxymetry: will it change management of critically ill neurologic patients? J Neurol Sci. 2007;261(1–2):1–9.
Wijdicks EF, et al. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67(2):203–10.
Broderick J, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Stroke. 2007;38(6):2001–23.
Adams HP Jr, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38(5):1655–711.
Varelas PN, et al. Impact of a neurointensivist on outcomes in patients with head trauma treated in a neurosciences intensive care unit. J Neurosurg. 2006;104(5):713–9.
Varelas PN, et al. The impact of a neuro-intensivist on patients with stroke admitted to a neurosciences intensive care unit. Neurocrit Care. 2008;9(3):293–9.
Lerch C, et al. Specialized neurocritical care, severity grade, and outcome of patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2006;5(2):85–92.
Suarez JI. Outcome in neurocritical care: advances in monitoring and treatment and effect of a specialized neurocritical care team. Crit Care Med. 2006;34(9 Suppl):S232–8.
Suarez JI, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 2004;32(11):2311–7.
Suarez JI. Neurocritical care. J Neurosurg. 2006;104(5):711–2 (discussion 712).
Rincon F, Mayer SA. Neurocritical care: a distinct discipline? Curr Opin Crit Care. 2007;13(2):115–21.
LaRovere KL, Riviello JJ Jr. Emerging subspecialties in neurology: building a career and a field: pediatric neurocritical care. Neurology. 2008;70(22):e89–91.
Bell MJ, et al. Development of a pediatric neurocritical care service. Neurocrit Care. 2009;10(1):4–10.
Ronen GM, et al. Long-term prognosis in children with neonatal seizures: a population-based study. Neurology. 2007;69(19):1816–22.
Stephens BE, Vohr BR. Neurodevelopmental outcome of the premature infant. Pediatr Clin North Am. 2009;56(3):631–46. Table of Contents.
Westmacott R, et al. Late emergence of cognitive deficits after unilateral neonatal stroke. Stroke. 2009;40(6):2012–9.
Eicher DJ, et al. Moderate hypothermia in neonatal encephalopathy: efficacy outcomes. Pediatr Neurol. 2005;32(1):11–7.
Shankaran S, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005;353(15):1574–84.
Gluckman PD, et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet. 2005;365(9460):663–70.
Jacobs S, et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2007;4:CD003311.
Azzopardi DV, et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med. 2009;361(14):1349–58.
Toet MC, Lemmers PM. Brain monitoring in neonates. Early Hum Dev. 2009;85(2):77–84.
Hirsch LJ. Continuous EEG monitoring in the intensive care unit: an overview. J Clin Neurophysiol. 2004;21(5):332–40.
Barkovich AJ. MR imaging of the neonatal brain. Neuroimaging Clin N Am. 2006;16(1):117–35 (viii–ix).
Gregory GA, et al. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971;284(24):1333–40.
Phibbs RH, et al. Initial clinical trial of EXOSURF, a protein-free synthetic surfactant, for the prophylaxis and early treatment of hyaline membrane disease. Pediatrics. 1991;88(1):1–9.
Levin DL, et al. Persistent pulmonary hypertension of the newborn infant. J Pediatr. 1976;89(4):626–30.
Jensen FE. Developmental factors regulating susceptibility to perinatal brain injury and seizures. Curr Opin Pediatr. 2006;18(6):628–33.
Ferriero DM. Oxidant mechanisms in neonatal hypoxia-ischemia. Dev Neurosci. 2001;23(3):198–202.
Vexler ZS, Yenari MA. Does inflammation after stroke affect the developing brain differently than adult brain? Dev Neurosci. 2009;31(5):378–93.
Miller SP, Ferriero DM. From selective vulnerability to connectivity: insights from newborn brain imaging. Trends Neurosci. 2009;32(9):496–505.
Ben-Ari Y, Holmes GL. Effects of seizures on developmental processes in the immature brain. Lancet Neurol. 2006;5(12):1055–63.
Sankar R, Rho JM. Do seizures affect the developing brain? Lessons from the laboratory. J Child Neurol. 2007;22(5 Suppl):21S–9S.
Silverstein FS, Jensen FE. Neonatal seizures. Ann Neurol. 2007;62(2):112–20.
Miller SP, et al. Seizure-associated brain injury in term newborns with perinatal asphyxia. Neurology. 2002;58(4):542–8.
Glass HC, et al. Clinical neonatal seizures are independently associated with outcome in infants at risk for hypoxic-ischemic brain injury. J Pediatr. 2009;155(3):318–23.
Shellhaas RA, Clancy RR. Characterization of neonatal seizures by conventional EEG and single-channel EEG. Clin Neurophysiol. 2007;118(10):2156–61.
Shellhaas RA, Soaita AI, Clancy RR. Sensitivity of amplitude-integrated electroencephalography for neonatal seizure detection. Pediatrics. 2007;120(4):770–7.
Toet MC, et al. Comparison between simultaneously recorded amplitude integrated electroencephalogram (cerebral function monitor) and standard electroencephalogram in neonates. Pediatrics. 2002;109(5):772–9.
Gunn AJ, et al. Therapeutic hypothermia: from lab to NICU. J Perinat Med. 2005;33(4):340–6.
Gunn AJ, et al. Cerebral hypothermia is not neuroprotective when started after postischemic seizures in fetal sheep. Pediatr Res. 1999;46(3):274–80.
Robertson NJ, et al. Therapeutic hypothermia for birth asphyxia in low-resource settings: a pilot randomised controlled trial. Lancet. 2008;372(9641):801–3.
Miller SP, et al. Comparing the diagnosis of white matter injury in premature newborns with serial MR imaging and transfontanel ultrasonography findings. AJNR Am J Neuroradiol. 2003;24(8):1661–9.
Inder TE, et al. White matter injury in the premature infant: a comparison between serial cranial sonographic and MR findings at term. AJNR Am J Neuroradiol. 2003;24(5):805–9.
Maalouf EF, et al. Comparison of findings on cranial ultrasound and magnetic resonance imaging in preterm infants. Pediatrics. 2001;107(4):719–27.
Rutherford MA, et al. Abnormal magnetic resonance signal in the internal capsule predicts poor neurodevelopmental outcome in infants with hypoxic-ischemic encephalopathy. Pediatrics. 1998;102(2 Pt 1):323–8.
Sie LT, et al. Predictive value of neonatal MRI with respect to late MRI findings and clinical outcome. A study in infants with periventricular densities on neonatal ultrasound. Neuropediatrics. 2005;36(2):78–89.
Barkovich AJ. Pediatric neuroimaging. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005.
Mathur AM, et al. Transport, monitoring, and successful brain MR imaging in unsedated neonates. Pediatr Radiol. 2008;38(3):260–4.
Acknowledgments
The authors would like to thank the neonatologists, neurologists, nurses, and families who have contributed, especially the NCRC research nurses, Michael Kuzniewicz, MD, from the ICN, Suzanne Golden, NNP, from the High Risk Infant Follow-Up Clinic and Kathleen Vandenberg, PhD (NIDCAP). The authors would also like to thank Drs. Wade Smith and Patrick McQuillen, and Ms. Amy Markowitz for their thoughtful review of the manuscript. This project was supported by NINDS/NCRR/OD UCSF-CTSI Grant Numbers KL2 RR024130 (HCG) and UL1 RR024131, the UCSF Newborn Institute and the Skippy Fund. DHR is a HHMI investigator. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Additional information
H. C. Glass and S. L. Bonifacio have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Glass, H.C., Bonifacio, S.L., Peloquin, S. et al. Neurocritical Care for Neonates. Neurocrit Care 12, 421–429 (2010). https://doi.org/10.1007/s12028-009-9324-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-009-9324-7