Abstract
Objectives
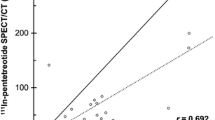
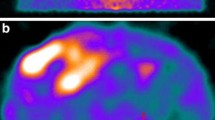
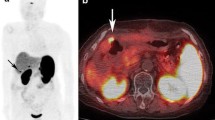
To compare the diagnostic accuracy of 111In-pentetreotide-scintigraphy with 68Ga-DOTATOC-positron emission tomography (PET)/computed tomography (CT) in patients with metastatic-neuroendocrine tumour (NET) scheduled for peptide receptor radionuclide therapy (PRRT). Incremental lesions (ILs) were defined as lesions observed on only one modality.
Methods
Fifty-three metastatic-NET-patients underwent 111In-pentetreotide-scintigraphy (24 h post-injection; planar+single-photon emission CT (SPECT) abdomen) and whole-body 68Ga-DOTATOC-PET/CT. SPECT and PET were compared in a lesion-by-lesion and organ-by-organ analysis, determining the total lesions and ILs for both modalities.
Results
Significantly more lesions were detected on 68Ga-DOTATOC-PET/CT versus 111In-pentetreotide-scintigraphy. More specifically, we observed 1,098 lesions on PET/CT (range: 1–105; median: 15) versus 660 on SPECT (range: 0–73, median: 9) (p<0.0001), with 439 PET-ILs (42/53 patients) and one SPECT-IL (1/53 patients). The sensitivity for PET/CT was 99.9 % (95 % CI, 99.3–100.0), for SPECT 60.0 % (95 % CI, 48.5–70.2). The organ-by-organ analysis showed that the PET-ILs were most frequently visualized in liver and skeleton.
Conclusion
Ga-DOTATOC-PET/CT is superior for the detection of NET-metastases compared to 111In-pentetreotide SPECT.
Key Points
• Somatostatin receptor PET is superior to SPECT in detecting NET metastases
• PET is the scintigraphic method for accurate depiction of NET tumour burden
• The sensitivity of PET is twofold higher than the sensitivity of SPECT




Similar content being viewed by others
References
Modlin IM, Oberg K, Chung DC et al (2008) Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol 9:61–72
Reubi JC, Schar JC, Waser B et al (2000) Affinity profiles for human somatostatin receptor subtypes SST1-SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med 27:273–282
Reubi JC, Waser B (2003) Concomitant expression of several peptide receptors in neuroendocrine tumours: molecular basis for in vivo multireceptor tumour targeting. Eur J Nucl Med Mol Imaging 30:781–793
Kwekkeboom DJ, Kooij PP, Bakker WH et al (1999) Comparison of 111In-DOTA-Tyr3-octreotide and 111In-DTPA-octreotide in the same patients: biodistribution, kinetics, organ and tumor uptake. J Nucl Med 40:762–767
Imhof A, Brunner P, Marincek N et al (2011) Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol 29:2416–2423
Kwekkeboom DJ, de Herder WW, Kam BL et al (2008) Treatment with the radiolabeled somatostatin analog [177 Lu-DOTA 0, Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol 26:2124–2130
Hofmann M, Maecke H, Borner R et al (2001) Biokinetics and imaging with the somatostatin receptor PET radioligand (68)Ga-DOTATOC: preliminary data. Eur J Nucl Med 28:1751–1757
Kwekkeboom DJ, Krenning EP, Scheidhauer K et al (2009) ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: somatostatin receptor imaging with (111)In-pentetreotide. Neuroendocrinology 90:184–189
Haug AR, Cindea-Drimus R, Auernhammer CJ et al (2012) The Role of 68Ga-DOTATATE PET/CT in Suspected Neuroendocrine Tumors. J Nucl Med 53:1686–1692
Koukouraki S, Strauss LG, Georgoulias V et al (2006) Evaluation of the pharmacokinetics of 68Ga-DOTATOC in patients with metastatic neuroendocrine tumours scheduled for 90Y-DOTATOC therapy. Eur J Nucl Med Mol Imaging 33:460–466
Teunissen JJ, Krenning EP, de Jong FH et al (2009) Effects of therapy with [177Lu-DOTA 0, Tyr 3]octreotate on endocrine function. Eur J Nucl Med Mol Imaging 36:1758–1766
Gabriel M, Decristoforo C, Kendler D et al (2007) 68Ga-DOTA-Tyr3-octreotide PET in neuroendocrine tumors: comparison with somatostatin receptor scintigraphy and CT. J Nucl Med 48:508–518
Buchmann I, Henze M, Engelbrecht S et al (2007) Comparison of 68Ga-DOTATOC PET and 111In-DTPAOC (Octreoscan) SPECT in patients with neuroendocrine tumours. Eur J Nucl Med Mol Imaging 34:1617–1626
Srirajaskanthan R, Kayani I, Quigley AM et al (2010) The role of 68Ga-DOTATATE PET in patients with neuroendocrine tumors and negative or equivocal findings on 111In-DTPA-octreotide scintigraphy. J Nucl Med 51:875–882
van Essen M, Krenning EP, Kam BL et al (2009) Peptide-receptor radionuclide therapy for endocrine tumors. Nat Rev Endocrinol 5:382–393
Meyer GJ, Macke H, Schuhmacher J et al (2004) 68Ga-labelled DOTA-derivatised peptide ligands. Eur J Nucl Med Mol Imaging 31:1097–1104
Van Binnebeek S, Deroose CM, Baete K et al (2011) Altered biodistribution of somatostatin analogues after first cycle of Peptide receptor radionuclide therapy. J Clin Oncol 29:e579–e581
Van Binnebeek S, Baete K, Terwinghe C et al (2013) Significant impact of transient deterioration of renal function on dosimetry in PRRT. Ann Nucl Med 27:74–77
Van Binnebeek S, Baete K, Vanbilloen B et al (2014) Individualized dosimetry-based activity reduction of (9)(0)Y-DOTATOC prevents severe and rapid kidney function deterioration from peptide receptor radionuclide therapy. Eur J Nucl Med Mol Imaging 41:1141–1157
Kowalski J, Henze M, Schuhmacher J et al (2003) Evaluation of positron emission tomography imaging using [68Ga]-DOTA-D Phe(1)-Tyr(3)-Octreotide in comparison to [111In]-DTPAOC SPECT. First results in patients with neuroendocrine tumors. Mol Imaging Biol 5:42–48
Geijer H, Breimer LH (2013) Somatostatin receptor PET/CT in neuroendocrine tumours: update on systematic review and meta-analysis. Eur J Nucl Med Mol Imaging 40:1770–1780
Treglia G, Castaldi P, Rindi G et al (2012) Diagnostic performance of Gallium-68 somatostatin receptor PET and PET/CT in patients with thoracic and gastroenteropancreatic neuroendocrine tumours: a meta-analysis. Endocrine 42:80–87
Schreiter NF, Brenner W, Nogami M et al (2012) Cost comparison of 111In-DTPA-octreotide scintigraphy and 68Ga-DOTATOC PET/CT for staging enteropancreatic neuroendocrine tumours. Eur J Nucl Med Mol Imaging 39:72–82
Acknowledgments
The scientific guarantor of this publication is Christophe M. Deroose. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. This study has received funding from the Instituut voor de Aanmoediging van Innovatie door Wetenschap en Technologie in Vlaanderen (IWT) http://www.iwt.be ; PROTOCOL: IWT-TBM Project: 0707181. Dr. K. Bogaerts, an profession expert on biostatistics from the Division of Public Health and primary Care (I-biostat), KU Leuven, Belgium is co-author of the article and provided statistical advice for this manuscript. Institutional Review Board approval was obtained from the ethics committee of the university hospitals and university of Leuven. Written informed consent was obtained from all subjects (patients) in this study.
Some results from this cohort have already been published. No data regarding the topic of this article, the comparison of diagnostic accuracy between 68Ga-DOTATOC and 111In-pentreotide, has been previously published. These findings are the integral and definitive results of this section of our prospective study, no other publications regarding this topic will follow. We published two case reports about two patients in this cohort. The first case report discusses the aberrant distribution of 68Ga-DOTATOC 7 weeks after one cycle of PRRT [1]. The second case report discusses the impact of renal insufficiency on kidney dose after PRRT [2]. Both these topics are unrelated to the diagnostic accuracy of the imaging methods. We also published results of the limited nephrotoxicity after PRRT using kidney dosimetry to modulate the administered activity to the patients [3]. This topic as well is fully unrelated to the diagnostic accuracy of the imaging methods discussed in the current manuscript.
Methodology: prospective, experimental, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Binnebeek, S., Vanbilloen, B., Baete, K. et al. Comparison of diagnostic accuracy of 111In-pentetreotide SPECT and 68Ga-DOTATOC PET/CT: A lesion-by-lesion analysis in patients with metastatic neuroendocrine tumours. Eur Radiol 26, 900–909 (2016). https://doi.org/10.1007/s00330-015-3882-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3882-1