Abstract
Fedratinib is an oral Janus kinase 2-selective inhibitor for the treatment of adult patients with intermediate-2 or high-risk myelofibrosis; however, some patients have difficulty with oral dosing. This randomized, phase 1, open-label, 2-part crossover study evaluated the relative bioavailability, safety, tolerability, taste, and palatability of fedratinib resulting from various alternative oral administration methods in healthy adults. Participants could receive fedratinib 400 mg orally as intact capsules along with a nutritional supplement; as contents of capsules dispersed in a nutritional supplement, delivered via nasogastric tube; or as a divided dose of 200 mg orally twice daily as intact capsules with a nutritional supplement. Fifty-eight participants received treatment. Total exposure to fedratinib was similar after oral administration of intact capsules or when dispersed in a nutritional supplement (area under the plasma concentration–time curve from time 0 to the time of the last quantifiable concentration geometric mean ratio [AUC0–t GMR] [90% CI], 1.007 [0.929–1.092]). Total exposure to fedratinib was slightly reduced following nasogastric administration (AUC0–t GMR 0.850 [0.802–0.901]) and as a divided dose (AUC0–t GMR 0.836 [0.789–0.886]). No new safety signals were identified for fedratinib, and most participants found the taste and palatability acceptable when dispersed in a nutritional supplement. Overall, results suggest no clinically meaningful differences in total exposure to fedratinib between the tested oral administration methods. These findings may facilitate administration of fedratinib to patients who are intolerant of swallowing the capsule dosage form. (ClinicalTrials.gov: NCT05051553).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelofibrosis is a myeloproliferative neoplasm associated with mutations in the cytoplasmic tyrosine kinase Janus kinase (JAK) 2, and dysregulation of the JAK/signal transducer and activator of transcription pathway [1]. Myelofibrosis is characterized by debilitating symptoms and poor survival rates [2]. Fedratinib, an oral, JAK2-selective inhibitor, is approved in the USA for the treatment of adult patients with intermediate-2 or high-risk myelofibrosis [3] and in the European Union for the treatment of splenomegaly or symptoms of disease in adult patients with myelofibrosis who are JAK-inhibitor naive or have been treated with ruxolitinib [4]. In the recent phase 3b, single-arm FREEDOM trial (NCT03755518) of 38 patients with myelofibrosis resistant/intolerant to prior ruxolitinib, fedratinib 400 mg/day reduced spleen volume (25.7% of patients achieved ≥ 35% spleen volume reduction at the end of cycle 6; 62.9% of patients had a best overall response of ≥ 35% spleen volume reduction at any time) and myelofibrosis symptom burden (44.4% of patients achieved ≥ 50% reduction in total symptom score at end of cycle 6) [5].
The current fedratinib 400 mg dosing is given as 4 × 100-mg, 21.4–22.0 mm (size 0) hard capsules, and is recommended to be taken with food [4]. However, for those patients who have difficulty swallowing solid-form medications [6], solid-form dosing may lead to reduced treatment adherence or treatment modifications by patients, potentially affecting safety and efficacy [7, 8]. Patients with myelofibrosis also experience a perception of early satiety and abdominal pain/discomfort resulting from spleen enlargement [9], which may contribute to an aversion to orally administered medication. Those who cannot take medications by mouth may require a nasogastric tube; however, alternative administration routes can affect medication pharmacokinetics (PKs) and bioavailability, and alter the benefit/risk profile of medications for patients [10, 11]. Previous studies have found that fedratinib shows a biphasic disposition and linear, time-invariant PKs [12], with a 3 h median (range, 2–4 h) time to peak concentration of the current fedratinib 400 mg dosing in patients with myelofibrosis [3]. The results of two phase 1 studies in healthy volunteers demonstrated that food has minimal impact on the bioavailability of fedratinib at 100 mg and 500 mg doses. Both studies showed a slight increase in maximum observed plasma concentration (Cmax), time to Cmax (Tmax), area under the plasma concentration–time curve (AUC) when fedratinib was administered directly after food compared with a 10-h fasted condition; however, increases in exposure were not clinically significant (< 25%) and terminal elimination half-life (t½) remained unaffected by fed and fasted conditions. Fedratinib tolerability was improved when taken following a high-fat breakfast [13].
Nausea is also a potential side effect of fedratinib. A total of 39.5% of patients in the FREEDOM study and 62% of patients in the JAKARTA trial experienced nausea [2, 5]. The improvement of gastrointestinal effects in the FREEDOM study versus JAKARTA was likely due to the administration of concomitant antiemetic medications, such as ondansetron, before fedratinib administration. These medications have been shown to reduce fedratinib-related nausea and vomiting without affecting the PKs of fedratinib [16], and are administered to all participants in postmarketing clinical pharmacology studies [17,18,19]. Additionally, the administration of fedratinib alongside a nutritional supplement has been found also to help alleviate nausea symptoms [3, 4].
In an effort to facilitate treatment of patients with myelofibrosis who have difficulty with the current fedratinib solid dosage form, this study evaluated administration of fedratinib dispersed in a nutritional supplement (either orally or via nasogastric tube) compared with intact capsules. In addition, to reduce the pill burden for patients who have difficulty taking all 4 × 100-mg capsules of fedratinib in a single dose, study part 2 investigated the impact of splitting the fedratinib intact capsule dose into 2 × 100-mg capsules administered twice daily (BID) on the total exposure to fedratinib compared with 4 × 100-mg capsules administered once daily (QD) alongside a nutritional supplement. The primary objective of this study (NCT05051553) was to evaluate the relative bioavailability of fedratinib 400 mg when administered orally as the contents of capsules dispersed in a nutritional supplement, the contents of capsules dispersed in a nutritional supplement via nasogastric tube, or as intact capsules with a nutritional supplement as a divided dose (200 mg BID) in comparison to intact capsules with a nutritional supplement in healthy adults.
The secondary objective was to evaluate the safety and tolerability of fedratinib administered by these methods in healthy adults. This study also had an exploratory objective of determining the taste and palatability of fedratinib when capsule contents were dispersed in a nutritional supplement.
Methods
Ethics approval
This phase 1 (NCT05051553), open-label, 2-part crossover study in healthy adult participants was conducted in compliance with the International Council on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use/Good Clinical Practice and applicable regulatory requirements. The protocol complied with the Declaration of Helsinki as well as applicable guidelines of the USA, the country where the study was conducted. The protocol was submitted to an independent review board (Advarra, Columbia, MD, USA) for review and written approval. This study was run by Syneos Health (Miami, FL, USA). Written informed consent was obtained from all participants at screening, prior to the conduct of any study-related procedures.
Study population
Healthy adults aged 18–65 years, with a body mass index 18–33 kg/m2, were eligible to be enrolled in either part of the study. Participants were confirmed to be healthy based on normal/clinically acceptable vital signs, laboratory results, and electrocardiograms at screening. People of childbearing potential were neither pregnant nor lactating, and all participants were required to use highly effective contraceptive measures until 30 days after the last dose of the study drug. Participants with a history of Wernicke’s encephalopathy, thiamine deficiency, hypersensitivity to ondansetron or any components of study drug, or contraindications for insertion of a nasogastric tube were excluded from the study.
Study design and treatment
This study comprised 2 parts in a randomized, multiple-sequence design. The study parts were planned to run in any order, or in parallel. Participants could only join 1 part of the study. Each study part was composed of a screening, a treatment phase, and a follow-up phone call (approximately 4 days [± 2 days] after discharge).
Study part 1 was a 2-period, 2-sequence, open-label, crossover design (Fig. 1A). Treatment 1A (reference) consisted of fedratinib 400 mg (4 × 100-mg capsules) administered orally along with approximately 180 mL of a commercially available nutritional supplement (ie, Ensure Plus). Treatment 1B (test) consisted of fedratinib 400 mg dispersed in a nutritional supplement and administered orally. Participants were randomized to receive treatment in one of the following sequences: 1A–1B or 1B–1A. All participants underwent a supervised overnight fast of ≥ 10 h the night before fedratinib dosing. No food or beverages (except water and any nutritional supplement administered with the treatment) were allowed for at least 4 h after dosing.
Study part 2 was a 3-period, 6-sequence, open-label, crossover design (Fig. 1B). Treatment 2A (reference) consisted of fedratinib 400 mg (4 × 100-mg capsules) administered orally alongside a nutritional supplement. Treatment 2B (test) consisted of fedratinib 400 mg dispersed in the nutritional supplement (180 mL, Ensure Plus), administered via nasogastric tube, and flushed with 60 mL of sterile water. Treatment 2C (test) consisted of fedratinib 400 mg as a divided dose (2 × 100-mg capsules BID) administered alongside the nutritional supplement. Participants were randomized to receive treatment in one of the following sequences: 2A–2B–2C, 2A–2C–2B, 2B–2A–2C, 2B–2C–2A, 2C–2A–2B, or 2C–2B–2A. As in study part 1, all participants underwent a supervised overnight fast of ≥ 10 h the night before dosing. In the case of an evening (second) dose in the divided dosing plan of treatment 2C, participants were directed to pre-fast at least 2 h before fedratinib dose, and 4 h after fedratinib dose, with water restricted from approximately 2 h before and 1 h after dosing, excluding water given with the treatment.
Approximately 1 h before each fedratinib administration, ondansetron oral tablet (film coated) 8 mg was given orally to reduce the potential for fedratinib-related nausea and vomiting [16]. There was a washout period of at least 12 days between each dose of fedratinib. The duration from screening through the follow-up phone call was approximately 10 weeks. Participants resided at the clinical site from days -1 to 23 (study part 1), or days -1 to 35 (study part 2). If a participant discontinued from the study for any reason, an early termination visit was performed, with only the safety assessments scheduled for the day of discharge taking place. Additionally, each participant who discontinued also received a follow-up phone call 4 (± 2) days after completion of the early termination visit.
Pharmacokinetic sampling, bioanalysis, and variables
For study part 1, and part 2 treatments 2A and 2B, blood samples were collected pre-dose (0 h) and at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 24, 48, 72, 120, 168, 192, and 240 h post-dose. For treatment 2C, blood samples were collected pre-dose (0 h) and at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 12.5, 13, 13.5, 14, 15, 16, 18, 24, 48, 72, 120, 168, 192, and 240 h post-dose of the first dose. The plasma concentration of fedratinib was measured using a validated liquid chromatography-tandem mass spectrometry assay with a lower limit of quantification of 1.00 ng/mL [12, 20].
Plasma PK parameters were calculated using noncompartmental methods by a validated PK analysis program (Phoenix® WinNonlin®, v8.3.4 [Certara USA, Inc., Princeton, NJ, USA]) using actual times. The PK parameters determined for fedratinib Cmax, Tmax, AUC from time 0 to the time of the last quantifiable concentration (AUC0–t), AUC from time 0 to infinity (AUC0–∞), and t½. Additionally for treatment 2C, Cmax and Tmax were estimated after both the first dose (Cmax and Tmax) and the second dose (Cmax2 and Tmax2). AUC0–t and AUC0–∞ were estimated from time 0 (the first dose) through 240 h after the first dose. AUC parameters were calculated using the linear-log trapezoidal method.
Safety assessment
The safety population included all participants who received at least 1 dose of fedratinib. Participants were monitored for adverse events (AEs) during the study, including assessments for clinical symptoms, biochemical, hematologic, and urinalysis laboratory results, physical examinations, 12-lead electrocardiograms, and vital signs. AEs were assessed for seriousness, severity, and relationship to the drug. AEs were assigned to the last study treatment administered at the time of onset, starting during or after the administration of the first dose. AEs that occurred after discharge were assigned to the last study treatment received for up to 30 days after the last dose of fedratinib.
Taste and palatability assessment
As an exploratory endpoint, participants in part 1 were asked to answer a questionnaire regarding taste and palatability on days 1 and 13 of the study. The questionnaire assessed participant perceptions of bitterness, astringency, and sandiness/grittiness at 2, 5, and 15 min after administration, other taste attributes, and impulse to chew or swallow.
Statistical considerations
The sample size for this study was based on consideration of the precision in the comparison of PK parameters, represented by the 90% confidence interval (CI) of the geometric mean ratios of Cmax and AUC of fedratinib. The evaluable PK population, used for PK summary and statistical analyses, was defined as all participants who received at least 1 dose of fedratinib and had at least 1 evaluable PK parameter. Only participants with valid PK data were included in the summary statistics and statistical analysis.
To compare the PK parameters and estimated relative bioavailability of fedratinib following different administration methods in each study part (treatment 1B to 1A, and treatment 2B and 2C to 2A), a linear mixed-effect model with treatment, period, and sequence as fixed effects and participant nested within sequence as a random effect was fitted to the natural log-transformed PK parameters (Cmax, AUC0–t, and AUC0–∞) for use in estimation of effects and construction of CIs.
In study parts 1 and 2, point estimates and 90% CI for the difference between test and reference treatments was exponentiated, and the ratio of geometric means (test/reference) and associated 90% CI was presented on the original scale. For comparison of treatment 2C to 2A in study part 2, the relative bioavailability assessment was based on only AUC. For Tmax, the difference between test and reference was assessed for significance using Wilcoxon signed-rank test. Kenward–Rogers degrees of freedom were specified in the linear mixed-effect model. The Hodges–Lehmann estimate and its 90% CI were calculated for median difference between treatments.
All statistical analyses were conducted using SAS v9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Participants and disposition
A total of 161 participants were enrolled, and 58 were randomized (36.0%) into the study and included in the PK and safety analyses. Of the 58 participants, 28 were included in study part 1 and 30 were included in study part 2 (Table 1). In total, 4 participants discontinued from the study, including 3 due to AEs (part 1, 2; part 2, 1); 1 participant withdrew from the study in part 1 (Table S1). Participant demographics and baseline characteristics were similar between the treatment groups and study parts (Table 1). For study parts 1 and 2, the mean age of participants was 38.5 and 41.7 years, respectively, and most participants were male (53.6% and 66.7% in parts 1 and 2, respectively; Table 1).
Relative bioavailability of fedratinib and PK parameters by oral administration method
Study part 1
Absorption of fedratinib occurred rapidly for both treatment 1A (intact capsules with nutritional supplement) and 1B (contents of capsules dispersed in nutritional supplement). In treatment 1A, the median (range) Tmax occurred at 2.1 (1.5–5.9) hours, compared with 2.0 (0.6–3.0) hours for treatment 1B (Table 2). After reaching Cmax, the decline in plasma concentration was gradual and prolonged for both treatment 1A and 1B (Fig. 2A and B), as indicated by long t½ (mean [standard deviation (SD)]: 103.0 [30.0] and 98.7 [28.2] hours for treatments 1A and 1B, respectively; Table 2). The ratio of geometric means (90% CI) for PK parameters between treatments 1B and 1A showed no apparent difference in exposure, with 1.007 (0.929–1.092) for AUC0–t, 1.009 (0.939–1.085) for AUC0–∞, and 1.059 (0.969–1.157) for Cmax (Table 3).
Fedratinib plasma concentration profile over time. Part 1 mean (+ SD) plasma concentration of fedratinib over time in linear (A) and semilogarithmic scales (B), and part 2 mean (+ SD) plasma concentration of fedratinib over time in linear (C) and semilogarithmic scales (D). On the linear profiles, points show mean + SD. BID, twice daily; LLOQ, lower limit of quantification; SD, standard deviation. 1A, oral administration of a single fedratinib 400-mg dose (4 × 100-mg capsules) with a nutritional supplement; 1B, oral administration of a single fedratinib 400-mg dose with contents of 4 × 100-mg capsules dispersed into a nutritional supplement; 2A, oral administration of a single fedratinib 400-mg dose (4 × 100-mg capsules) with a nutritional supplement; 2B, single fedratinib 400-mg dose administered via nasogastric tube as contents from 4 × 100-mg capsules dispersed into a nutritional supplement; 2C, oral administration of fedratinib 400 mg given as a divided dose (2 × 100-mg capsules BID) with a nutritional supplement
Interparticipant variability across treatments was moderate, with coefficient of variation (CV) ranging from 39 to 46% for Cmax, AUC0–t, and AUC0–∞ across treatments 1A and 1B (Table 2).
Study part 2
Treatment 2B (dispersed capsules, nasogastric tube) versus Treatment 2A (intact capsules)
The median (range) Tmax occurred rapidly in both treatments, at 2.9 (1.4–6.1) hours for treatment 2A and at 1.9 (1.0–3.0) hours for treatment 2B (Table 2). The decline in plasma fedratinib concentration after Cmax was gradual and prolonged with both treatments 2A and 2B (Fig. 2C and D), with a mean (SD) t½ of 96.8 (27.6) and 106.0 (31.4) hours, respectively. Overall, fedratinib exposure was slightly reduced for treatment 2B compared with 2A. The ratio of geometric means (90% CI) for PK parameters between treatment 2B and 2A was 0.850 (0.802–0.901) for AUC0–t, 0.863 (0.816–0.912) for AUC0–∞, and 0.898 (0.837–0.963) for Cmax (Table 5).
Interparticipant variability across treatments was moderate, with CV ranging from 35 to 38% for Cmax, AUC0–t, and AUC0–∞ across treatments 2A and 2B (Table 2).
Treatment 2C (divided dose, 2 × 100-mg intact capsules BID) versus treatment 2A (4 × 100-mg intact capsules)
Absorption of fedratinib was rapid for treatment 2C and treatment 2A, with median (range) Tmax occurring at 1.9 (1.4–6.0) and 2.9 (1.4–6.1) hours, respectively, after first doses. After the second dose of treatment 2C, the median (range) Tmax2 was 3.9 (1.0–6.0) hours (Table 2). The geometric mean Cmax for treatment 2C after the first dose (641.0 ng/mL) was approximately half of the Cmax of treatment 2A (1388.0 ng/mL), as expected. After reaching Cmax, the decline of plasma concentration was gradual and prolonged (Fig. 2C and D), with the mean (SD) t½ of fedratinib being similar between treatment 2A (96.8 [27.6] hours) and treatment 2C (96.7 [26.2] hours). Overall, exposure to fedratinib was reduced for treatment 2C compared with treatment 2A. The ratio of geometric means (90% CI) for PK parameters between treatment 2C and treatment 2A was 0.836 (0.789–0.886) for AUC0–t and 0.850 (0.804–0.899) for AUC0–∞ (Table 4).
Interparticipant variability for treatment 2C was moderate, with CV of 40% to 41% for Cmax, AUC0–t, and AUC0–∞ (Table 2).
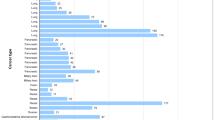
Safety
Overall, 38/58 (65.5%) of participants in the safety population had at least 1 AE. The number and proportion of participants who reported AEs was similar among all treatment groups. In study part 1, 11/27 (40.7%) participants who received treatment 1A and 10/27 (37.0%) participants who received treatment 1B reported at least 1 AE (Table S2). In study part 2, 9/30 (30.0%) participants who received treatment 2A, 9/30 (30.0%) participants who received treatment 2B, and 12/30 (40.0%) participants who received treatment 2C reported at least 1 AE (Table S2). In the full safety population (n = 58) the most common AEs were constipation (12.1%), diarrhea (10.3%), and somnolence (10.3%). Most AEs were mild in severity (4 moderate AEs were reported by 3 participants in study part 2), suspected to be related to the study drug, and resolved without any medication. While no deaths or serious/severe AEs were reported during the study, 3 participants discontinued due to AEs, with 2 AEs suspected to be related to the study drug (gamma-glutamyl transferase and alanine transaminase increases, which resolved within 2 months without medication; influenza-like illness, which resolved within 2 weeks of onset; and ear pain, which resolved within 2 days of onset).
Taste and palatability
In part 1A (fedratinib 400 mg [4 × 100-mg capsules] administered orally alongside a nutritional supplement), 100% of participants with recorded assessments reported the bitterness, astringency, and sandiness to be acceptable at all time points, and most participants (55.6%) had an impulse to swallow. In part 1B (fedratinib 400 mg dispersed in a nutritional supplement and administered orally), all participants with recorded assessments found the bitterness, astringency, and sandiness associated with drug administration to be acceptable after initial drug administration, and 77.8% of participants had an impulse to swallow. After 15 min, 96.3% of participants found the astringency and sandiness to be acceptable, while bitterness acceptability was 81.5%. Overall, the reporting of unacceptable taste and palatability was higher when the contents of the capsule were dispersed in nutritional supplement (treatment 1B) compared with swallowing an intact capsule (treatment 1A).
Discussion
It is important to investigate alternative routes of oral administration to assist with patient comfort and treatment adherence [8]; however, changes in oral administration methods may alter the PK properties of the compound, thus affecting bioavailability [7, 8]. This study evaluated impact of various alternative oral dosing options on fedratinib bioavailability.
In part 1 of this study, exposure to fedratinib was shown to be similar following oral administration of intact capsules (treatment 1A), or oral administration of the contents of capsules dispersed in a nutritional supplement (treatment 1B). Tmax occurred slightly sooner with treatment 1B, possibly as no time was required for capsule disintegration, and the fine particles in the capsule contents may have dissolved quickly. In part 2, exposure to fedratinib was slightly reduced following administration via a nasogastric tube (treatment 2B) or as a divided dose (treatment 2C) compared with the one-time orally administered dose (treatment 2A), though no clinically meaningful differences were observed. Reduced exposure with nasogastric tube administration compared with oral formulation has been observed in multiple compounds with distinct PK properties, although the extent varies and exact reasons have not been well understood [10, 21,22,23,24]. For example, small differences in Cmax and AUC values between intact capsules and nasogastric administration have been observed for gefitinib, a tyrosine kinase inhibitor, with no clinically significant differences in bioavailability and PK parameters found overall [22].
In this study, reduced exposure following administration via a nasogastric tube was unlikely to be caused by drug instability or inadequate flushing, as in vitro studies demonstrated near-complete drug recovery from the nasogastric tube and the compound remained stable up to 1 h in suspension (data on file). Reduced exposure was also unlikely to be due to misplacement of the nasogastric tube, as placement was confirmed through X-ray imaging (data on file). The differences in exposure to fedratinib between treatments 2B, 2C, and 2A were likely to be due to interparticipant variability. Furthermore, the 90% CI for the difference in exposure to fedratinib between treatments 2B and 2A fell within the 0.8–1.25 range conventionally defined as having no clinical effect [25,26,27,28]. While the lower boundary of the 90% CI of the difference in AUC0–t between 2C and 2A only fell slightly lower than 0.8 (0.789), the other PK results in this study would suggest that there were no clinically meaningful differences between 2C and 2A.
Within study part 2, Tmax2 was slightly longer than Tmax after the first dose in treatment 2C. This was likely due to a shorter fasting period, approximately 3 h, compared with the overnight fasting in treatments 2B and 2A and before the first dose of treatment 2C, as food has been shown to affect the Tmax of fedratinib without affecting fedratinib exposure [13].
There is a general lack of published PK data for kinase inhibitors through alternative oral administration routes, which may be due to the general poor aqueous solubility of small molecular tyrosine kinase inhibitors [29]. Exploratory PK analyses of patients who received baricitinib, a JAK inhibitor indicated for use in some patients with moderately to severely active rheumatoid arthritis [30], as a solution of crushed tablets via a nasogastric tube were consistent with PK results previously reported for baricitinib in healthy adults and in patients with rheumatoid arthritis [31]. To our knowledge, this is the first study evaluating the effect of alternative administration methods on the PK parameters of a JAK inhibitor for myelofibrosis. While ruxolitinib can be administered through a nasogastric tube and the prescribing information contains specific instructions for the suspension, dilution, and timing of administration [32], the effect of this route of administration on drug exposure has not been demonstrated [32]. The prescribing information for pacritinib, like fedratinib, states that capsules should not be opened, broken, or chewed [33], but no studies of the effect on pacritinib exposure appear to have been published. Thus, no data about other JAK inhibitors are available for comparison with the fedratinib data from this study.
Few oral cancer drugs report enteral tube administration alternatives, and fewer still have instructions of nasogastric administration [34]. Vandetanib, gefitinib, and osimertinib, all tyrosine kinase inhibitors used in various cancer therapies, state in their prescribing information that they can be administered through a nasogastric tube, and each have specific instructions for the suspension, dilution, and timing of administration [35,36,37], though only gefitinib appears to have published bioavailability and safety results of different administration methods [22, 38]
Overall, no new safety signals were identified compared with the FREEDOM study and other previous studies, including any treatment-emergent serious AEs [2, 5, 19, 39]. The number and proportion of participants experiencing AEs was similar among all treatment groups. Most of the AEs suspected to be related to fedratinib were mild in intensity and resolved without medication, though 3 individuals were discontinued from the study due to AEs.
Lastly, most participants in study part 1 found the taste and palatability of fedratinib administration to be acceptable for both treatment 1A and 1B. The taste and palatability of alternative administration methods is an important consideration as taste, texture, and smell may affect overall treatment adherence [6,7,8]
Some potential limitations of the study include that the participants in study part 2C, oral administration of fedratinib 400 mg given as a divided dose (2 × 100-mg capsules BID) with a nutritional supplement, were unable to have the same fasting period for both doses due to practical reasons, potentially affecting the results as described above. Finally, not all participants in study part 1A had taste and palatability reported at all time points; therefore, the assessment of taste and palatability could not be interpreted with rigor.
Conclusion
Overall, the results of this study suggest that there is no clinically meaningful difference in exposure to fedratinib 400 mg/day after nasogastric tube administration or oral administration as a divided dose (2 × 100-mg capsules BID) compared with standard capsule administration (4 × 100-mg/day). These findings provide an alternative means of administering fedratinib to patients with myelofibrosis who are intolerant of swallowing capsule dosage forms.
Data sharing statement
The data that support the findings of this study are available on request from Bristol Myers Squibb. The data are not publicly available due to privacy or ethical restrictions. The Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.
References
Vainchenker W, Kralovics R (2017) Genetic basis and molecular pathophysiology of classical myeloproliferative neoplasms. Blood 129(6):667–679
Pardanani A, Tefferi A, Masszi T et al (2021) Updated results of the placebo-controlled, phase III JAKARTA trial of fedratinib in patients with intermediate-2 or high-risk myelofibrosis. Br J Haematol 195(2):244–248
Celgene Corp. Inrebic® (fedratinib) prescribing information. May 23. Available at: https://packageinserts.bms.com/pi/pi_inrebic.pdf. Accessed 26 Jun 2023
Inrebic® (fedratinib) summary of product characteristics. Denham, UK; Bristol-Myers Squibb; June 2022. June 2023. https://www.ema.europa.eu/en/documents/product-information/inrebic-epar-product-information_en.pdf. Accessed 12 July 2023
Gupta V, Yacoub A, Verstovsek S et al (2022) Safety and efficacy of fedratinib in patients with primary (P), post-polycythemia vera (post-PV), and post-essential thrombocythemia (post-ET) myelofibrosis (MF) previously treated with ruxolitinib: primary analysis of the FREEDOM trial. Blood 140(Supplement 1):3935–3937
Fields J, Go JT, Schulze KS (2015) Pill properties that cause dysphagia and treatment failure. Curr Ther Res Clin Exp 77:79–82
Mc Gillicuddy A, Crean AM, Sahm LJ (2016) Older adults with difficulty swallowing oral medicines: a systematic review of the literature. Eur J Clin Pharmacol 72(2):141–151
McCloskey AP, Penson PE, Tse Y, Abdelhafiz MA, Ahmed SN, Lim EJ (2022) Identifying and addressing pill aversion in adults without physiological-related dysphagia: a narrative review. Br J Clin Pharmacol 88(12):5128–5148
Mesa RA, Schwager S, Radia D et al (2009) The Myelofibrosis Symptom Assessment Form (MFSAF): an evidence-based brief inventory to measure quality of life and symptomatic response to treatment in myelofibrosis. Leuk Res 33(9):1199–1203
Song Y, Wang X, Perlstein I et al (2015) Relative bioavailability of apixaban solution or crushed tablet formulations administered by mouth or nasogastric tube in healthy subjects. Clin Ther 37(8):1703–1712
Undre N, Dickinson J (2017) Relative bioavailability of single doses of prolonged-release tacrolimus administered as a suspension, orally or via a nasogastric tube, compared with intact capsules: a phase 1 study in healthy participants. BMJ Open 7(4):e012252
Ogasawara K, Zhou S, Krishna G, Palmisano M, Li Y (2019) Population pharmacokinetics of fedratinib in patients with myelofibrosis, polycythemia vera, and essential thrombocythemia. Cancer Chemother Pharmacol 84(4):891–898
Zhang M, Xu C, Ma L et al (2015) Effect of food on the bioavailability and tolerability of the JAK2-selective inhibitor fedratinib (SAR302503): results from two phase I studies in healthy volunteers. Clin Pharmacol Drug Dev 4(4):315–321
Pardanani A, Gotlib JR, Jamieson C et al (2011) Safety and efficacy of TG101348, a selective JAK2 inhibitor, in myelofibrosis. J Clin Oncol 29(7):789–796
Harrison CN, Schaap N, Vannucchi AM et al (2020) Fedratinib in patients with myelofibrosis previously treated with ruxolitinib: An updated analysis of the JAKARTA2 study using stringent criteria for ruxolitinib failure. Am J Hematol 95(6):594–603
Ogasawara K, Vince B, Xu C, Zhang M, Palmisano M, Krishna G (2020) A phase I study of the effect of repeated oral doses of pantoprazole on the pharmacokinetics of a single dose of fedratinib in healthy male subjects. Cancer Chemother Pharmacol 85(5):995–1001
Chen Y, Ogasawara K, Wood-Horrall R et al (2022) Effect of fluconazole on the pharmacokinetics of a single dose of fedratinib in healthy adults. Cancer Chemother Pharmacol 90(4):325–334
Ogasawara K, Kam J, Thomas M et al (2021) Effects of strong and moderate CYP3A4 inducers on the pharmacokinetics of fedratinib in healthy adult participants. Cancer Chemother Pharmacol 88(3):369–377
Ogasawara K, Wood-Horrall RN, Thomas M et al (2021) Impact of fedratinib on the pharmacokinetics of transporter probe substrates using a cocktail approach. Cancer Chemother Pharmacol 88(6):941–952
Ogasawara K, LoRusso PM, Olszanski AJ et al (2020) Assessment of effects of repeated oral doses of fedratinib on inhibition of cytochrome P450 activities in patients with solid tumors using a cocktail approach. Cancer Chemother Pharmacol 86(1):87–95
Yuk JH, Nightingale CH, Sweeney KR, Quintiliani R, Lettieri JT, Frost RW (1989) Relative bioavailability in healthy volunteers of ciprofloxacin administered through a nasogastric tube with and without enteral feeding. Antimicrob Agents Chemother 33(7):1118–1120
Cantarini MV, McFarquhar T, Smith RP, Bailey C, Marshall AL (2004) Relative bioavailability and safety profile of gefitinib administered as a tablet or as a dispersion preparation via drink or nasogastric tube: results of a randomized, open-label, three-period crossover study in healthy volunteers. Clin Ther 26(10):1630–1636
Rosemurgy AS, Markowsky S, Goode SE, Plastino K, Kearney RE (1995) Bioavailability of fluconazole in surgical intensive care unit patients: a study comparing routes of administration. J Trauma 39(3):445–447
Dodds Ashley ES, Varkey JB, Krishna G et al (2009) Pharmacokinetics of posaconazole administered orally or by nasogastric tube in healthy volunteers. Antimicrob Agents Chemother 53(7):2960–2964
Heinig R, Fricke R, Wertz S, Nagelschmitz J, Loewen S (2022) Results from drug-drug Interaction studies in vitro and in vivo investigating the inhibitory effect of finerenone on the drug transporters BCRP, OATP1B1, and OATP1B3. Eur J Drug Metab Pharmacokinet 47(6):803–815
Chen G, Lee R, Hojer AM, Buchbjerg JK, Serenko M, Zhao Z (2013) Pharmacokinetic drug interactions involving vortioxetine (Lu AA21004), a multimodal antidepressant. Clin Drug Investig 33(10):727–736
Jiang W, Makhlouf F, Schuirmann DJ et al (2015) A bioequivalence Aapproach for generic narrow therapeutic index drugs: evaluation of the reference-scaled approach and variability comparison criterion. AAPS J 17(4):891–901
US Food and Drug Administration (2014) Guidance for Industry Bioavailability and Bioequivalence Studies Submitted in NDAs or INDs — General Considerations
Herbrink M, Nuijen B, Schellens JH, Beijnen JH (2015) Variability in bioavailability of small molecular tyrosine kinase inhibitors. Cancer Treat Rev 41(5):412–422
Lilly USA. Olumiant® (baricitinib) prescribing information. June 2022. Available at: https://pi.lilly.com/us/olumiant-uspi.pdf. Accessed June 29, 2023.
Marconi VC, Ramanan AV, de Bono S et al (2021) Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial. Lancet Respir Med 9(12):1407–1418
Incyte. Jakafi®(ruxolitinib) prescribing information. January 2023. https://www.jakafi.com/pdf/prescribing-information.pdf. Accessed April 17, 2023
CTI BioPharma Corp. Vonjo® (pacritinib) prescribing information. February 2022. https://www.ctibiopharma.com/wp-content/uploads/2022/03/VONJO_PI_02-2022.pdf. Accessed April 17, 2023.
Spencer SH, Menard SM, Labedz MZ, Krueger CD, Sarna KV (2020) Enteral tube administration of oral chemotherapy drugs. J Oncol Pharm Pract 26(3):703–717
Genzyme Corp. Caprelsa® (vandetanib) prescribing information. March 2022. https://www.caprelsa.com/files/caprelsa-pi.pdf. Accessed April 17, 2023.
AstraZeneca. Iressa® (gefitinib) prescribing information. February 2023. https://medicalinformation.astrazeneca-us.com/home/prescribing-information/iressa.html. Accessed June 29, 2023.
AstraZeneca. Tagrisso® (osimertinib) prescribing information. June 2023. http://www.astrazeneca-us.com/cgi-bin/az_pi.cgi?product=tagrisso&country=us&popup=no. Accessed June 29, 2023.
Cantarini MV, Bailey CJ, Collins B, Smith RP (2008) The relative bioavailability of gefitinib administered by granular formulation. Cancer Chemother Pharmacol 62(2):203–208
Pardanani A, Harrison C, Cortes JE et al (2015) Safety and efficacy of fedratinib in patients With primary or secondary myelofibrosis: a randomized clinical trial. JAMA Oncol 1(5):643–651
Acknowledgements
The authors thank the participants and families who made this study possible and the clinical study teams who participated in the trial. We would like to acknowledge Donna Carroll, from Bristol Myers Squibb, for assistance with formulation characterization of fedratinib in a nasogastric tube. Professional medical writing support for this manuscript was provided by Alisha B. Adams, PhD, and Katie Walwyn-Brown, PhD of Caudex, a division of IPG Health Medical Communications, funded by Bristol Myers Squibb.
Funding
The clinical study reported was supported and funded by Bristol Myers Squibb.
Author information
Authors and Affiliations
Contributions
YC, DW, Mark Thomas, Michael Thomas, BH, LL, LC, KO, and GK all contributed to the conception or design of the study. Mark Thomas, DW, and YX were involved in the acquisition of data. YC, MA, Mark Thomas, BH, RN, and VS contributed to the analysis of the data. All authors contributed to the interpretation of the data and reviewed and approved article content before submission.
Corresponding author
Ethics declarations
Conflicts of interest
DW has no conflicts of interest to declare. RN is an employee of Bristol Myers Squibb. YC, MA, Mark Thomas, Michael Thomas, BH, LL, VS, YX, LNC, KO, and GK are employees of and hold stock or stock options in Bristol Myers Squibb.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Y., Wyatt, D., Attanasio, M. et al. Relative bioavailability of fedratinib through various alternative oral administration methods in healthy adults. Cancer Chemother Pharmacol 93, 307–317 (2024). https://doi.org/10.1007/s00280-023-04612-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-023-04612-w