Abstract
This study aimed to evaluate the efficacy and safety of chidamide (Chi) combined with a modified Busulfan-Cyclophosphamide (mBuCy) conditioning regimen for T-cell acute lymphoblastic leukemia/lymphoma (T-ALL/LBL) patients undergoing allogeneic hematopoietic stem cell transplantation (allo-HSCT). Twenty-two patients received chidamide combined with mBuCy conditioning regimen (Chi group). A matched-pair control (CON) group of 44 patients (matched 1:2) received mBuCy only in the same period. The leukemia-free survival (LFS), overall survival (OS), cumulative incidence of relapse (CIR), and non-relapse-related mortality (NRM) were evaluated. Patients in the Chi group were associated with lower 2-year CIR (19.0 vs. 41.4%, P = 0.030), better 2-year LFS (76.1 vs. 48.1%, P = 0.014), and had no significant difference in 2-year OS (80.5 vs. 66.4%, P = 0.088). Patients with minimal residual disease (MRD) positive before HSCT in the Chi group exhibited an advantage in 2-year LFS and a trend towards better 2-year OS (75.0 vs. 10.2%, P = 0.048; 75.0 vs. 11.4%, P = 0.060, respectively). Multivariable analysis showed that the chidamide intensified regimen was independently associated with better LFS (HR 0.23; 95%CI, 0.08–0.63; P = 0.004), and showed no significant impact with OS for all patients (HR 0.34, 95%CI, 0.11–1.07; P = 0.064). The cumulative incidence rates of grade II-IV aGVHD were similar (36.4 vs. 38.6%, P = 0.858). 20 patients in Chi group evinced an elevation in γ-glutamyltransferase, as compared to the mBuCy group (90.9 vs. 65.9%, P = 0.029). No transplantation-related mortality was documented within the first 100 days after transplantation. The results demonstrate that the chidamide intensified regimen may be an effective and acceptable safety option for T-ALL/LBL undergoing allo-HSCT, and further validation is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
T-cell acute lymphoblastic leukemia/lymphoma (T-ALL/LBL) has a poor response to chemotherapy and an extremely bad prognosis due to its tendency to high white blood cells, central nervous system, and extramedullary infiltration [1,2,3,4,5]. Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a potentially curative treatment [6, 7]. However, the cumulative incidence of post-transplant relapse in T-ALL/LBL was 30 to 50%, constituting a major cause of patient mortality [8,9,10,11,12]. And the 2-year overall survival (OS) probability after relapse was about 10 to 46% [9, 12, 13]. Intensifying conditioning regimens is one of the potential ways to reduce relapse rates. The modified Bu-Cy (mBuCy) conditioning regimen is the predominant myeloablative therapy in China, owing to its low transplant-related mortality and efficient hematopoietic reconstitution [14, 15]. However, when administered to T-ALL/LBL patients, this regimen remains limited by its inability to eliminate minimal residual disease (MRD) and high incidence of relapse following transplantation. Therefore, further refinement and optimization of the T-ALL/LBL conditioning regimen is imperative.
As the first oral subtype-selective histone deacetylase inhibitor (HDACi) approved in China [16], the real-world study has demonstrated that chidamide has a favorable efficacy and an acceptable safety profile for T-lymphocytic malignancies patients [17]. Chidamide could inhibit proliferation and induce apoptosis via cell cycle arrest and the regulation of apoptotic proteins in T-cell malignancies [18, 19]. Of note, chidamide combined with chemotherapy regimens can decrease MRD in T-ALL patients with NOTCH1 mutation [20]. Given its promising antitumor activity and synergistic effects, Ji et al. incorporated chidamide into the lymphoma pretreatment regimen (ChiCGB). The 4-year progression-free survival (PFS) and OS rates for high-risk or relapsed/refractory lymphomas were significantly improved, reaching 80.6% and 86.1%, respectively [21]. To date, the role of chidamide in T-ALL/LBL conditioning regimens in allo-HSCT has not been explored. Here, we retrospectively compared the clinical efficacy and safety between mBuCy combined with chidamide and mBuCy conditioning regimen for T-ALL/LBL patients undergoing allo-HSCT.
Methods
Patients
We conducted a retrospective study at the First Affiliated Hospital of Soochow University between December 21, 2017, and February 21, 2022, to evaluate the safety and efficacy of the chidamide-containing conditioning regimen for high-risk T-ALL/LBL. 22 patients received the chidamide combined with modified Bu-Cy regimen (Chi group), 44 similar patients received only modified Bu-Cy (CON group) and underwent allo-HSCT during the same period. Disease types included T-ALL/LBL, early T-cell precursor acute lymphoblastic leukemia (ETP-ALL) and T-lymphoid/myeloid mixed phenotype acute leukemia (T/M MPAL). This study was approved by the ethics committee of the First Affiliated Hospital of Soochow University, and all patients provided written informed consent before treatment in accordance with the Helsinki Declaration.
Propensity score matching
To reduce the impact of potential confounders, we employed propensity score matching (PSM). The following matching variables were used as covariates: age and sex of patients, diagnosis, disease status before transplantation, donor/recipient gender match, donor type, source of stem cells and whether patients were relapsed or refractory. Optimal pair matching based on propensity scores in a 1:2 ratio was conducted, with a caliper of 0.2 standard deviations. A propensity score test validated the normalization impact of covariate matching, as indicated in Table S1.
Conditioning regimens
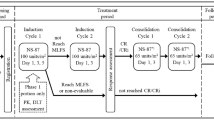
Patients in the Chi group received chidamide in combination with the mBuCy as a conditioning regimen. If the donors were haploidentical type, chidamide was administered 15 mg orally on days − 14, -12, -9, -7, and − 5 before chemotherapy. The patients received Me-CCNU 250 mg/m2/d orally on day − 12, cytarabine 2 g/m2 i.v. every 12 h on days − 11 to − 10 for a total of 4 doses, busulfan 0.8 mg/kg i.v. every 6 h on days − 9 to − 7 (12 doses), and cyclophosphamide 1.8 g/m2/d i.v. on days − 5 and − 4. If the donors were HLA-matched siblings or unrelated types, chidamide was administered 15 mg orally on days − 11, -9, -7, and − 5 before chemotherapy. The patients received Me-CCNU 250 mg/m2/d orally on day − 11, cytarabine 2 g/m2 i.v. every 12 h on day − 10, busulfan 0.8 mg/kg i.v. every 6 h on days − 9 to − 7 (12 doses), and cyclophosphamide 1.8 g/m2/d i.v. on days − 5 and − 4. Patients in the CON group only received the same mBuCy regimen except for chidamide.
Graft-versus-host disease prophylaxis
The graft-versus-host disease (GVHD) prophylaxis protocol is the same as our center’s previously published study [22, 23]. The prophylaxis regimen included cyclosporine A (CsA) with short-course methotrexate (MTX) for related identical donor transplantation, and CsA, short-course MTX, mycophenolate mofetil (MMF), and rabbit anti-thymocyte globulin (Thymoglobulin™) for unrelated and haploidentical transplantation. CsA 3 mg/kg/d was continuously infused for 24 h from day − 9, of which the trough concentration was adjusted to 150–200 ng/ml. It was switched to oral administration when the patient’s bowel function normalized again after the transplant. From day − 9, 0.5 g of MMF was administered orally every 12 h and was discontinued on day + 28 post-transplant. Short-course MTX was administered on days + 1 (15 mg/m2), + 3, +6, and + 11 (10 mg/m2). Rabbit-ATG (2.5 mg/kg/d, i.v.) was used from day − 5 to − 2.
Definitions and statistical methods
OS was the time from transplantation to death. Leukemia-free survival (LFS) was the time from transplantation to leukemia relapse, death, or last follow-up. Non-relapse-related mortality (NRM) was defined as the time from transplantation to death of any causes other than hematologic disease relapse. Relapse was defined as the reappearance of leukemia cells (≥ 5%) in the peripheral blood or bone marrow of patients in complete remission or the development of extramedullary disease. Refractory was defined as (1) Failure of initial induction therapy after two or more courses of treatment; (2) early recurrence less than 6 months after the first remission; (3) inefficacy to response to induction chemotherapy after recurrence; and (4) multiple relapses. For univariate comparison, the Mann–Whitney U test was used for continuous variables, and the chi-square test or Fisher’s exact test for categorical variables. The Cox proportional hazards model was used for univariate and multivariate analysis. OS and LFS were estimated by the Kaplan–Meier method and compared by using the log-rank test. The CIR was estimated using Gray’s sub-distribution method to account for the presence of competing risk due to non-relapse mortality. P values < 0.05 were considered significant. All analyses in this study were performed using the IBM Statistical Package for Social Sciences version 25 and R version 4.2.2.
Results
Patient enrollment and characteristics
66 patients with T-ALL/LBL were screened and enrolled, and 22 patients received a chidamide-containing conditioning regimen. Patients’ characteristics are shown in Table 1. The median age at transplantation was 28 (range, 19–37) years, and 59 (89.4%) of 66 patients were male. The median time from diagnosis to HSCT was 179 (range, 122–229) days. The pre-transplant characteristics were similar between the two groups.
Engraftment and GVHD
All patients achieved hematopoietic reconstitution. The neutrophil engraftment in Chi and CON groups occurred at 11 (range, 11–13) days and 11 (range, 11–12) days (P = 0.412), respectively. Platelet engraftment time was 13 (range 12–17) days in the Chi group and 14 (range 12–14) days in the CON group (P = 0.842), respectively. The incidences of day 100 grade II–IV (36.4 vs. 38.6%; P = 0.858) and III–IV (13.6 vs. 20.5%; P = 0.735) aGVHD were not significantly different between Chi and CON groups, respectively. There was no difference in the incidence of 2-year cGVHD between the Chi group and CON group (36.4 vs. 38.5%, P = 0.858) (Table 2).
Safety
Consistent with patients in the CON group, all patients in the Chi group manifested severe myelosuppression. The foremost non-hematologic adverse event (AE) observed was gastrointestinal tract reactions including diarrhea (Chi group, 59.1%; CON group, 54.9%; P = 0.724) and nausea (Chi group, 54.5%; CON group, 74.3%; P = 0.079). Hepatic dysfunction was more often observed in the Chi group. 20 patients evinced an elevation in γ-glutamyltransferase, as compared to the mBuCy group (90.9 vs. 65.9%, respectively; P = 0.029). (Table 2).
Seventeen (77.3%) patients administered the Chi regimen developed treatment-related infections, primarily pneumonia (54.6%). Severe adverse events including sepsis were reported in 3 cases (13.6%) of the Chi group and 3 cases (6.8%) of the mBuCy group (P = 0.650) (Table 2). All three cases in the Chi group were gram-negative infections. No instances of treatment-related death were reported in the Chi group during the treatment period.
Non-relapse related mortality and overall survival
The median follow-up time in the Chi group was 733 (range 368–1255) days, while that of the CON group was 684 (range 246–1219) days. There was no significant difference in OS between two groups (80.5% for Chi group vs. 60.4% for CON group, P = 0.063, Fig. 1a), while median OS was not reached in either group. The incidence of NRM was similar between the Chi and CON groups (5.5 vs. 21.1%, P = 0.108, Fig. 2b). The 2-year OS for T-ALL patients was similar in both groups (80.8 vs. 66.9%, P = 0.401, Fig. 1c). ETP-ALL and MPAL had similar biological characteristics, immunophenotypes, and poor outcomes [24, 25]. In our study, they were incorporated into the same group. And no differences were observed in two groups for patients with ETP-ALL and MPAL (66.7 vs. 33.2%, P = 0.511, Fig. 1e). Despite being not statistically significant, patients with MRD positive before HSCT in Chi group exhibited an advantage in 2-year OS (75.0 vs. 11.4%, P = 0.060). The univariate analysis of OS was shown in Table 3. In multivariate analysis, chidamide combined with mBuCy showed no correlation with OS for all patients (HR 0.34, 95%CI, 0.11–1.07; P = 0.064), while grade III-IV aGVHD (HR 4.72, 95%CI, 1.53–14.59; P = 0.007), MRD positive before HSCT (HR 3.22, 95%CI, 1.23–8.44; P = 0.018), and non-CR status of primary disease (HR 6.30, 95%CI, 1.96–20.31; P = 0.002) was associated with a lower OS (Table 4).
Kaplan-Meier curves of overall survival and leukemia-free survival. (a) Overall survival and (b) leukemia-free survival of all patients in the Chi group (n = 22) and CON group (n = 44). (c) Overall survival and (d) leukemia-free survival of T-ALL patients in the Chi group (n = 11) and CON group (n = 22). (e) Overall survival and (f) leukemia-free survival of ETP-ALL and T/ M MPAL patients in the Chi group (n = 6) and CON group (n = 14). (g) Overall survival and (h) leukemia-free survival of patients with MRD positive before HSCT in the Chi group (n = 4) and CON group (n = 14)
Relapse and leukemia-free survival
At the time of the last follow-up, 5 patients in the Chi group and 20 patients in the CON group relapsed after transplantation. The median time from transplantation to relapse was 255 days and 266 days, respectively. The Chi group had a significantly lower 2-year CIR than the CON group (19.0 vs. 41.4%, P = 0.030) (Fig .2a). Furthermore, compared to the CON group, the Chi group had a better 2-year LFS (76.1 vs. 45.3%, P = 0.014, Fig. 1b). For patients with T-ALL, 2-year LFS was similar between Chi and CON group (80.8 vs. 59.5%, P = 0.094, Fig. 1d), while no difference was found between two groups for patients with ETP-ALL or T/M MPAL (66.7 vs. 17.3%, P = 0.207, Fig. 1f). In the subgroup of patients with MRD-positive before transplantation, the Chi group exhibited a better 2-year LFS (75.0 vs. 10.2%, P = 0.048). The univariate analysis of LFS was shown in Table 3. In multivariate analysis, chidamide combined with mBuCy (HR 0.23; 95%CI, 0.08–0.63; P = 0.004), and stem cells source of bone marrow stem cells combined with peripheral blood stem cells (PBSC + BM) (HR 0.18, 95%CI, 0.04–0.76; P = 0.020) showed a significant association with a higher LFS, while grade III-IV aGVHD (HR 3.41, 95%CI, 1.08–10.83; P = 0.037) and non-CR status of primary disease (HR 3.72, 95%CI, 1.09–12.73; P = 0.036) was associated with a lower LFS (Table 4).
Discussion
Despite HSCT being a reliable treatment option, T-ALL/LBL is often accompanied by a dismal prognosis, with a high likelihood of post-transplant relapse. In our propensity matched cohort study, the combination of chidamide and mBuCy conditioning regimen improves the survival of patients without increasing the incidence of transplant-related mortality.
The possible mechanisms for chidamide to improve the mBuCy regimen efficacy may include: (1) Chidamide has a direct anti-leukemic effect: chidamide can block the cell cycle at the G0/G1 phase and induce apoptosis by activating the endogenous apoptotic signaling pathways simultaneously [26]. (2) Chidamide has a synergistic effect in combination with chemotherapy, especially the alkylating agent busulfan: preclinical studies had found that HDAC inhibitors lead to a more relaxed chromatin structure through chromatin remodeling, particularly hyperacetylation of lysine residues in the histone tails, which facilitates the expression of tumor suppressor genes as well as the action of chemotherapy [27,28,29,30]. (3) The poor prognosis of DT-negative T-ALL patients was associated with abnormal DNA aggregation leading to drug resistance (e.g. VP16, MTX) [31, 32], and chidamide may be able to overcome conventional chemotherapy resistance based on its chromatin-releasing activity. (4) Chidamide combined with chemotherapy regimens can effectively decrease MRD in T-ALL patients with NOTCH1 mutation [20].
For T-ALL/LBL, especially high risk, a large portion of post-transplant relapse is due to failure to effectively eliminate MRD in bone marrow or extramedullary disease. Intensified conditioning regimens are expected to improve this situation. Our study confirmed that adding chidamide to the mBuCy regimen significantly attenuated the CIR without increasing the incidence of NRM. As a result, the patients who received the chi-intensified regimen achieved a better 2-year LFS compared to those who received the mBuCy conditioning regimen. Multivariate analysis also suggested that the Chi regimen was associated with superior LFS. Currently, TBI-based regimens are more recommended than chemo-based regimens for conditioning of T-ALL [33, 34]. The TBI-based conditioning regimens in ALL appears to be more effective than the mBuCy regimen, especially for T-ALL patients aged < 35 years can benefit significantly from the regimen of TBI based regimen (5-year LFS of 50% for TBI vs. 18% for chemo-only regimen or Bu-Cy regimens) [34,35,36,37]. However, in the haplo-HSCT setting, the application of the mBuCy regimen is more widespread and well established in our center. Recent RCT studies have also shown that, for ALL patients undergoing haplo-HSCT, there were no differences in 2-year OS, CIR, NRM, regimen-related toxicity, GVHD, or late effects between two regimens, indicating noninferiority of BuCy [38]. Given that chidamide has a synergistic effect in combination with the alkylating agent busulfan [27, 29, 30], this may enhance the efficacy of conditioning. Therefore, we choose to add chidamide to the mBuCy regimen rather than TBI-based regimens. Compared to the TBI-based conditioning regimen, a report from the acute leukemia working party of EBMT, our outcomes displayed a higher 2-year OS (80.8 vs. about 60%). Compared with the conventional chemo-based regimen (iv Bu-Cy and oral Bu-Cy), the survival difference was more significant (80.8 vs. about 30%) [34]. TBI-based regimens have advantages for the clearance of extramedullary disease, and in our study, two patients who still with extramedullary disease before transplantation both experienced extramedullary relapse and died after transplantation. There were four patients with MRD positive before transplantation in the Chi group and all were diagnosed with T-ALL, one patient died of relapse 329 days after transplantation, and the remaining three patients continued in leukemia-free survival. Compared to the mBuCy group, the MRD-positive patients in the Chi group exhibited a better LFS and an advantage OS (75.0 vs. 10.2%, 75.0 vs. 11.4%, respectively), which is consistent with previous research [20]. Hence, from the preliminary favorable results, T-ALL/LBL patients without extramedullary infiltration before transplantation may benefit from this chi-intensified regimen, especially for those with positive MRD. Unfortunately, for ETP-ALL and T/M MPAL, compared to a previous study in our center, no significant difference was seen in the OS and LFS [24]. Three patients with ETP-ALL or MPAL experienced relapse in the Chi group. One patient with MPAL died soon after relapse, and two patients with ETP-ALL prolonged survival with reinduction therapy and radiotherapy. As a high-risk subtype in T-ALL/LBL [2], ETP-ALL does not seem to benefit from the Chi-intensified conditioning regimen.
Two previous research have shown that chidamide had little toxicities in the autologous stem cell transplantation of non-Hodgkin’s lymphomas (chidamide 30 mg/day orally on days − 7, -4, 0, + 3, and chidamide 30 mg/day orally on days − 7, -4, + 1, +3) [21, 39]. In our study (chidamide 15 mg/day orally on days − 12, -9, -7, -5 for haploidentical donors and chidamide 15 mg/day orally on days − 11, -9, -7, -5 for HLA match siblings or unrelated donors), despite the Chi group being associated with a higher incidence of elevation in γ-glutamyltransferase, it did not result in fatal or severe toxicity when compared to the mBuCy regimen, and liver dysfunction all had been resolved after symptomatic treatment. Considering SAEs after transplantation were comparable between the two groups, we hold that this regimen is relatively safe and manageable.
It is acknowledged that there are some limitations in our study. Our evaluation was based on a retrospective analysis of a smaller sample size. Additionally, patient selection bias may have arisen during the enrollment. We also recognized that the cytotoxicity and efficacy of chidamide are influenced by the dosage regimen (timing, frequency, and dose), necessitating further optimization. To confirm our results, we anticipate conducting future prospective randomized controlled trials on a larger scale.
To our knowledge, this is the first study to combine chidamide into a conditioning regimen for allo-HSCT in T-ALL/LBL, and the preliminary results are encouraging. Our study suggests that compared with standard mBuCy regimens, chidamide combined with mBuCy conditioning regimen may be an effective and acceptable safety option.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- T-ALL/LBL:
-
T acute lymphoblastic leukemia/lymphoma
- ETP-ALL:
-
Early T-cell precursor acute lymphoblastic leukemia
- T/M MPAL:
-
T/myeloid mixed phenotype acute leukemia
- Allo-HSCT:
-
Allogeneic hematopoietic stem cell transplantation
- MRD:
-
Minimal residual disease
- Haplo:
-
Haploidentical
- SIB:
-
HLA-matched sibling
- URD:
-
HLA-matched unrelated
- PBSC:
-
Peripheral blood stem cells
- BM:
-
Bone marrow
- GVHD:
-
Graft-versus-host disease
- aGVHD:
-
Acute graft-versus-host disease
- cGVHD:
-
Chronic graft-versus-host disease
- OS:
-
Overall survival
- LFS:
-
Leukemia-free survival
- CR:
-
Complete remission
- NR:
-
No remission
- PR:
-
Partial remission
- NRM:
-
Non-relapse-related mortality
- HDAC:
-
Histone deacetylases
- HDACi:
-
Histone deacetylases inhibitor
- CMV:
-
Cytomegalovirus
- EBV:
-
Epstein-Barr virus
References
Guru MG, Pondaiah SK, Abedin S, Atallah E (2019) Incidence and survival of t-cell acute lymphoblastic leukemia in the United States. Leuk Lymphoma 60(5):1171–1178. https://doi.org/10.1080/10428194.2018.1522442
Jain N, Lamb AV, O’Brien S, Ravandi F, Konopleva M, Jabbour E et al (2016) Early t-cell precursor acute lymphoblastic leukemia/lymphoma (etp-all/lbl) in adolescents and adults: a high-risk subtype. Blood 127(15):1863–1869. https://doi.org/10.1182/blood-2015-08-661702
Attarbaschi A, Mann G, Dworzak M, Wiesbauer P, Schrappe M, Gadner H (2002) Mediastinal mass in childhood t-cell acute lymphoblastic leukemia: significance and therapy response. Med Pediatr Oncol 39(6):558–565. https://doi.org/10.1002/mpo.10164
Deangelo DJ, Yu D, Johnson JL, Coutre SE, Stone RM, Stopeck AT et al (2007) Nelarabine induces complete remissions in adults with relapsed or refractory t-lineage acute lymphoblastic leukemia or lymphoblastic lymphoma: cancer and leukemia group b study 19801. Blood. 109(12):5136-42. https://doi.org/10.1182/blood-2006-11-056754
Weinberg OK, Arber DA (2010) Mixed-phenotype acute leukemia: historical overview and a new definition. Leukemia 24(11):1844–1851. https://doi.org/10.1038/leu.2010.202
Tian H, Xu Y, Liu L, Yan L, Jin Z, Tang X et al (2016) Comparison of outcomes in mixed phenotype acute leukemia patients treated with chemotherapy and stem cell transplantation versus chemotherapy alone. Leuk Res 45:40–46. https://doi.org/10.1016/j.leukres.2016.04.002
Kawada H, Yoshimitsu M, Nakamura D, Arai A, Hayashida M, Kamada Y et al (2015) A retrospective analysis of treatment outcomes in adult t cell leukemia/lymphoma patients with aggressive disease treated with or without allogeneic stem cell transplantation: a single-center experience. Biol Blood Marrow Transpl 21(4):696–700. https://doi.org/10.1016/j.bbmt.2014.12.020
Yu J, Ge X, Luo Y, Shi J, Tan Y, Lai X et al (2020) Incidence, risk factors and outcome of extramedullary relapse after allogeneic hematopoietic stem cell transplantation in patients with adult acute lymphoblastic leukemia. Ann Hematol 99(11):2639–2648. https://doi.org/10.1007/s00277-020-04199-9
Kamiunten A, Sekine M, Kameda T, Akizuki K, Tahira Y, Shide K et al (2018) Outcome of allogeneic hematopoietic cell transplantation in patients with adult t-cell leukemia. Hematol Oncol 36(4):651–655. https://doi.org/10.1002/hon.2549
Mcmahon CM, Luger SM (2019) Relapsed t cell all: current approaches and new directions. Curr Hematol Malig Rep 14(2):83–93. https://doi.org/10.1007/s11899-019-00501-3
Kato K, Uike N, Wake A, Yoshimitsu M, Tobai T, Sawayama Y et al (2019) The outcome and characteristics of patients with relapsed adult t cell leukemia/lymphoma after allogeneic hematopoietic stem cell transplantation. Hematol Oncol 37(1):54–61. https://doi.org/10.1002/hon.2558
Candoni A, Lazzarotto D, Ferrara F, Curti A, Lussana F, Papayannidis C et al (2020) Nelarabine as salvage therapy and bridge to allogeneic stem cell transplant in 118 adult patients with relapsed/refractory t-cell acute lymphoblastic leukemia/lymphoma. A campus all study. Am J Hematol 95(12):1466–1472. https://doi.org/10.1002/ajh.25957
Chen H, Qin Y, Yang J, Liu P, He X, Zhou S et al (2022) Dismal outcome of relapsed or primary refractory adult t-cell lymphoblastic lymphoma: a retrospective study from China. Asia Pac J Clin Oncol 18(2):e87–95. https://doi.org/10.1111/ajco.13562
Zhang XH, Chen J, Han MZ, Huang H, Jiang EL, Jiang M et al (2021) The consensus from the Chinese society of hematology on indications, conditioning regimens and donor selection for allogeneic hematopoietic stem cell transplantation: 2021 update. J Hematol Oncol 14(1):145. https://doi.org/10.1186/s13045-021-01159-2
Zhao XF, Mao XF, Wan DM, Liu W (2014) Modified busulfan and cyclophosphamide conditioning regimen for allogeneic hematopoietic stem cell transplantation in the treatment of patients with hematologic malignancies. Transpl Proc 46(5):1531–1535. https://doi.org/10.1016/j.transproceed.2014.02.023
Suresh PS, Devaraj VC, Srinivas NR, Mullangi R (2017) Review of bioanalytical assays for the quantitation of various hdac inhibitors such as vorinostat, belinostat, panobinostat, romidepsin and chidamine. Biomed Chromatogr 31(1). https://doi.org/10.1002/bmc.3807
Shi Y, Jia B, Xu W, Li W, Liu T, Liu P et al (2017) Chidamide in relapsed or refractory peripheral t cell lymphoma: a multicenter real-world study in China. J Hematol Oncol 10(1):69. https://doi.org/10.1186/s13045-017-0439-6
Cao HY, Li L, Xue SL, Dai HP (2022) Chidamide: targeting epigenetic regulation in the treatment of hematological malignancy. Hematol Oncol. https://doi.org/10.1002/hon.3088
Gao S, Li X, Zang J, Xu W, Zhang Y (2017) Preclinical and clinical studies of chidamide (cs055/hbi-8000), an orally available subtype-selective hdac inhibitor for cancer therapy. Anticancer Agents Med Chem 17(6):802–812. https://doi.org/10.2174/1871520616666160901150427
Xi M, Guo S, Bayin C, Peng L, Chuffart F, Bourova-Flin E et al (2022) Chidamide inhibits the notch1-myc signaling axis in t-cell acute lymphoblastic leukemia. Front Med 16(3):442–458. https://doi.org/10.1007/s11684-021-0877-y
Ji J, Liu Z, Kuang P, Dong T, Chen X, Li J et al (2021) A new conditioning regimen with chidamide, cladribine, gemcitabine and busulfan significantly improve the outcome of high-risk or relapsed/refractory non-hodgkin’s lymphomas. Int J Cancer 149(12):2075–2082. https://doi.org/10.1002/ijc.33761
Tang X, Valdez BC, Ma Y, Zhang Q, Qu C, Dai H et al (2021) Low-dose decitabine as part of a modified bu-cy conditioning regimen improves survival in aml patients with active disease undergoing allogeneic hematopoietic stem cell transplantation. Bone Marrow Transpl 56(7):1674–1682. https://doi.org/10.1038/s41409-021-01238-5
Xu GF, Liu LM, Wang M, Zhang ZB, Xie JD, Qiu HY et al (2022) Treatments of ph-like acute lymphoblastic leukemia: a real-world retrospective analysis from a single large center in China. Leuk Lymphoma 63(11):2652–2662. https://doi.org/10.1080/10428194.2022.2090550
Liu S, Cui Q, Dai H, Song B, Cui W, Xue S et al (2021) Early t-cell precursor acute lymphoblastic leukemia and t/myeloid mixed phenotype acute leukemia possess overlapping characteristics and both benefit from cag-like regimens and allogeneic hematopoietic stem cell transplantation. Transpl Cell Ther 27(6):481. https://doi.org/10.1016/j.jtct.2021.02.032
Noronha EP, Marques L, Andrade FG, Sardou-Cezar I, Dos SF, Zampier C et al (2019) T-lymphoid/myeloid mixed phenotype acute leukemia and early t-cell precursor lymphoblastic leukemia similarities with notch1 mutation as a good prognostic factor. Cancer Manag Res 11:3933–3943. https://doi.org/10.2147/CMAR.S196574
Gong K, Xie J, Yi H, Li W (2012) Cs055 (chidamide/hbi-8000), a novel histone deacetylase inhibitor, induces g1 arrest, ros-dependent apoptosis and differentiation in human leukaemia cells. Biochem J 443(3):735–746. https://doi.org/10.1042/BJ20111685
Rosato RR, Grant S (2005) Histone deacetylase inhibitors: insights into mechanisms of lethality. Expert Opin Ther Targets 9(4):809–824. https://doi.org/10.1517/14728222.9.4.809
Secrist JP, Zhou X, Richon VM (2003) Hdac inhibitors for the treatment of cancer. Curr Opin Investig Drugs 4(12):1422–1427
Valdez BC, Murray D, Nieto Y, Li Y, Wang G, Champlin RE et al (2012) Synergistic cytotoxicity of the dna alkylating agent busulfan, nucleoside analogs and suberoylanilide hydroxamic acid in lymphoma cell lines. Leuk Lymphoma 53(5):973–981. https://doi.org/10.3109/10428194.2011.634043
Valdez BC, Nieto Y, Murray D, Li Y, Wang G, Champlin RE et al (2012) Epigenetic modifiers enhance the synergistic cytotoxicity of combined nucleoside analog-dna alkylating agents in lymphoma cell lines. Exp Hematol 40(10):800–810. https://doi.org/10.1016/j.exphem.2012.06.001
Xiao H, Wang S, Tang Y, Li S, Jiang Y, Yang Y et al (2023) Absence of terminal deoxynucleotidyl transferase expression in t-all/lbl accumulates chromosomal abnormalities to induce drug resistance. Int J Cancer 152(11):2383–2395. https://doi.org/10.1002/ijc.34465
Zhou Y, Fan X, Routbort M, Cameron YC, Singh R, Bueso-Ramos C et al (2013) Absence of terminal deoxynucleotidyl transferase expression identifies a subset of high-risk adult t-lymphoblastic leukemia/lymphoma. Mod Pathol 26(10):1338–1345. https://doi.org/10.1038/modpathol.2013.78
Niu J, Chen Z, Gao J, Qiu H, Wan L, Wang Y et al (2022) Total body irradiation-based conditioning regimen improved the survival of adult patients with t-cell lymphoblastic lymphoma after allogeneic peripheral blood stem cell transplantation. Cell Transpl 31:73800550. https://doi.org/10.1177/09636897221108890
Cahu X, Labopin M, Giebel S, Aljurf M, Kyrcz-Krzemien S, Socie G et al (2016) Impact of conditioning with tbi in adult patients with t-cell all who receive a myeloablative allogeneic stem cell transplantation: a report from the acute leukemia working party of ebmt. Bone Marrow Transpl 51(3):351–357. https://doi.org/10.1038/bmt.2015.278
Fu H, Xu L, Liu D, Liu K, Zhang X, Chen H et al (2014) Total body irradiation and cyclophosphamide plus antithymocyte globulin regimen is well tolerated and promotes stable engraftment as a preparative regimen before t cell-replete haploidentical transplantation for acute leukemia. Biol Blood Marrow Transpl 20(8):1176–1182. https://doi.org/10.1016/j.bbmt.2014.04.012
Kanda Y, Sakamaki H, Sao H, Okamoto S, Kodera Y, Tanosaki R et al (2005) Effect of conditioning regimen on the outcome of bone marrow transplantation from an unrelated donor. Biol Blood Marrow Transpl 11(11):881–889. https://doi.org/10.1016/j.bbmt.2005.07.005
Shi-Xia X, Xian-Hua T, Hai-Qin X, Bo F, Xiang-Feng T (2010) Total body irradiation plus cyclophosphamide versus busulphan with cyclophosphamide as conditioning regimen for patients with leukemia undergoing allogeneic stem cell transplantation: a meta-analysis. Leuk Lymphoma 51(1):50–60. https://doi.org/10.3109/10428190903419130
Zhang H, Fan Z, Huang F, Han L, Xu Y, Xu N et al (2023) Busulfan plus Cyclophosphamide versus total body irradiation plus cyclophosphamide for adults acute b lymphoblastic leukemia: an open-label, multicenter, phase iii trial. J Clin Oncol 41(2):343–353. https://doi.org/10.1200/JCO.22.00767
Xia Y, Wang L, Ding K, Wu J, Yin H, Hu M et al (2023) Chidamide-Beac plus autologous stem cell transplantation in high-risk non-hodgkin lymphoma: a phase ii clinical trial. Chin Med J (Engl) 136(12):1491–1493. https://doi.org/10.1097/CM9.0000000000002636
Acknowledgements
The authors would like to thank all members of the study team, the patients, and their families.
Funding
This work was supported by research grants from National Natural Science Foundation of China (82070162), Frontier Clinical Technical Project of Suzhou Science and Technology plan (SKY2022001), Bethune Charitable Foundation (BCF-IBW-XY-20220930-13), Suzhou diagnosis and treatment project of Clinical Key Diseases (LCZX202201), China International Medical Foundation (Z-2018-31-2102-4), Boxi clinical research project of The First Affiliated Hospital of Soochow University (BXLC005), the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Contributions
XWT, B.A. and DPW designed the study. XWT, HPD, ZL, YMZ, MYL, SFC, WC, JY, JC, ANS, HYQ, SNC, and XMZ selected and treated patients and contributed data. XQC and QYC analyzed the data and wrote the article. QYC, ZL, and YJM critically reviewed the article. All authors read and approved the final version of the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was obtained from all patients for being included in the study. This study was in accordance with the Helsinki Declaration and approved by the ethics committee of the First Affiliated Hospital of Soochow University (retrospective ethics review number:2023 − 339).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cao, X., Li, Z., Zhang, Y. et al. Chidamide combined with a modified Bu-Cy conditioning regimen improves survival in patients with T-cell acute lymphoblastic leukemia/lymphoma undergoing allogeneic hematopoietic stem cell transplantation. Ann Hematol (2024). https://doi.org/10.1007/s00277-024-05849-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-05849-y