Abstract
Philadelphia chromosome-like (Ph-like) ALL is a recent subtype of acute lymphoblastic leukemia. Although it does not express the BCR-ABL fusion gene, it has a behavior like true BCR/ABL1–positive cases. This subtype harbors different molecular alterations most commonly CRLF2 rearrangements. Most cases of Ph-like ALL are associated with high white blood cell count, high minimal residual disease level after induction therapy, and high relapse rate. Efforts should be encouraged for early recognition of Ph-like ALL to enhance therapeutic strategies. Recently, many trials are investigating the possibility of adding the tyrosine kinase inhibitor (TKI) to chemotherapy to improve clinical outcomes. The role and best timing of allogeneic bone marrow transplant in those cases are still unclear. Precision medicine should be implemented in the treatment of such cases. Here in this review, we summarize the available data on Ph-like ALL
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute lymphoblastic leukemia (ALL) is a common pediatric malignancy, associated with a good prognosis and a high cure rate. In contrast, adult ALL has a more dismal prognosis. That has been attributed to patients’ comorbidities, poor performance status, poor compliance, and higher frequency of poor-risk genomic subgroups [1].
Philadelphia (Ph)-positive chromosome is a genetic translocation between chromosomes 9 and 22 that causes the production of a BCR-ABL1 aberrant fusion gene (BCR, breakpoint cluster region gene; ABL, Abelson proto-oncogene; BCR/ABL. chimeric gene of BCR and ABL) [2] which was reported to be present in 11–30%, and 1–5% of adult and children respectively. This translocation was considered one of the worst prognostic factors before the era of tyrosine kinase inhibitors (TKI) [3]. Rearrangement involving the minor breakpoint in the BCR gene encodes a 190-kDa protein which is more prevalent in both adult and pediatric cases than the major one which encodes a 210-kDa protein [4, 5].
The term “Philadelphia–like” or “BCR/ABL1–like” ALL was defined in 2009 by Boer et al. In their study, they described a subset of ALL with negative (BCR/ABL1, histone-lysine methyltransferase 2 [KMT2A], and transcription factor 3 [TCF3], and pre-B-cell-leukemia transcription factor 1 [PBX1]) but had behavior like “true BCR/ABL1–positive cases” [6]. This was the same observation of Haferlach et al., in 2005 [7]. Later in 2016, the World Health Organization included Ph-like ALL as a novel provisional entity under ALL with known cytogenetic abnormalities and updated in the International Consensus Classification (ICC) of myeloid neoplasms and acute leukemias 2022 [8, 9].
Ph-like ALL may harbor different molecular alterations including (i) rearrangements of CRLF2 (cytokine receptor-like factor 2 receptor), which is the most common; (ii) ABL-class rearrangements; (iii) JAK2, and/or EPOR rearrangements; (iv) other mutation in JAK/STAT signaling; (v) other kinase mutations such as FLT3, NTRK3, PTK2B, and BLNK genes; and (vi) RAS mutations [10, 11]. Notably, all the previously mentioned genes are known to be involved in B cell proliferation, differentiation, and cell cycle regulation. When mutations occur in those genes, constitutive kinase activation would occur through the activation of JAK-STAT, RAS, and ABL1 pathways [12].
The former classification is based upon the similarity of functions of these gene fusions and their potential sensitivity to tyrosine kinase inhibitors (TKI) (e.g., SRC/ABL/PDGFR inhibitors for ABL class fusions and JAK inhibitors for CRLF2, EPOR, and JAK2 rearrangements) [13]. However, JAK inhibitor ruxolitinib could be used in SH2B3 deletions, and TRK (tropomyosin receptor kinase) inhibitors crizotinib and larotrectinib could be used in cases with NTRK fusions [13]. The frequency of the previously mentioned alterations is different according to different age groups; CRLF2 rearrangements are the most common genetic alterations across all age groups. Among children, ABL-class gene rearrangements are more frequent, while among young adults, there is an increase in the frequency of JAK2 rearrangements (Fig. 1) [14].
Relative frequency of Ph-like ALL alterations in children, adolescents, and adults, adopted from Tran et al. [14]
Molecular abnormalities in Ph-like ALL
CRLF2-rearrangements
CRLF2 rearrangements are the most common rearrangements in Ph-like ALL patients, present in approximately 50% of those patients [15]. The CRLF2 protein is a cytokine receptor that dimerizes with the interleukin-7 receptor (IL7R)-α—located in the sex chromosomes at Xp22.3/Yp11.3. Upon its binding to its ligand, cellular proliferation without differentiation would be provoked through activation of the JAK/STAT and PI3K/AKT/mTOR pathways [16, 17].
Overexpression of CRLF2 is a predictor for poor prognosis in ALL patients [18]. This overexpression in CRLF2 might be due to (i) chromosomal translocation with immunoglobulin heavy-chain locus (IGH)-CRLF2 fusion, (ii) a cryptic interstitial deletion which results in a P2Y receptor family member 8 (P2RY8)-CRLF2 fusion, and rarely (iii) CRLF2 point mutations provoking uncontrolled receptor activation, but sometimes, this may also represent a secondary aberration or a co-occurrence with an established primary lesion, such as the iAMP21, or with high hyper-diploidy [15, 17, 19]. Notably, patients with IGH-CRLF2 have higher CRLF2 expression than those with P2RY8-CRLF2 and, consequently, have a higher risk of relapse rate [20]. CRLF2 deregulation alone is not sufficient to start leukemogenesis; usually, those patients have additional drive mutations like JAK/STAT pathway [21].
Interestingly, it was reported that half the cases of CRLF2-R rearrangements had concomitant JAK2 mutations (most commonly R683G); this entity is named (JAK2 mutant type/CRLF2 rearranged). While (JAK2 wild-type/CRLF2-rearranged) cases show frequent mutations in JAK1, JAK3, FLT3, and the coreceptor IL7R; deletion of the JAK2 negative regulator SH2B3; and translocation IQGAP2-TSLP resulting in CRLF2 ligand overexpression [15, 22]. Notably, the CRLF2-R Ph-like ALL patients with concomitant JAK mutation are mutually exclusive with those who harbor concomitant IL7R rearrangements [13]. This group is associated with a worse prognosis [23]. Moreover, IKAROS family zinc finger 1 (IKZF1) is an epigenetic regulator of CRLF2, and the presence of a mutation in IKZF1 leads to overexpression of CRLF2, and this group of patients has a more favorable prognosis [24]. Unfunctionally, IKZF1 alterations are usually accompanied by PAX5 (paired-box 5) alterations, which make the outcome worse [25]. Furthermore, the GATA3 rs3824662 gene risk allele was identified as a susceptibility locus for Ph-like ALL according to the observation of Perez Andreu et al., and others that the ALL patients who harbored GATA3 rs3824662 gene risk allele were associated with CRLF2 overexpression, JAK mutation, IKZF1 rearrangement, and those patients had a higher risk of relapse [26, 27]. This observation was confirmed in a cohort of Egyptian children that patients with the GATA3 rs3824662 genotype had poor prognosis with a higher incidence of relapse and short disease-free survival [28].
ABL-rearrangements
The second common rearrangement in Ph-like ALL is ABL class fusions or translocations which represent nearly 15% of all Ph-like patients with a higher incidence in children than adults [29]. These rearrangements involve the following fusions genes, ABL1, ABL2, CSF1R, PDGFRA, PDGFRB, and FGFR. The presence of any of these translocations is enough to diagnose Ph-like ALL [30]. Notably, these translocations are mutually exclusive with CRLF2 and JAKS/TAT mutations but usually associated with IKZF1 mutations/deletions [17]. The presence of EBF1-PDGFRB (platelet-derived growth factor B) rearrangement has a higher rate of induction failure and measurable minimal residual disease (MRD) [31]. Furthermore, it was reported that acquiring AGGF1-PDGFRB mutation in PDGFRBC843G might be the underlying mechanism of resistance to the ABL TKIs, e.g., imatinib, dasatinib, but could be responsive to multi-target kinase inhibitor like (type II JAK2 inhibitors) CHZ868 [32].
JAK2 and/or EPOR translocations
Erythropoietin receptor rearrangements (EPOR) and JAK2 rearrangements are nearly present in 7–5% of Ph-like ALL cases; these rearrangements activate JAK-STAT signaling without concomitant CRLF2 alterations [15, 33]. This class comprises JAK2 rearrangements and rearrangements of the EPOR with the immunoglobulin-heavy (IGH) or kappa (IGK) loci that deregulate EPOR expression [34]. This group of patients has the worst prognosis [29]. EPOR rearrangements are 2-fold more common in young adult patients than in children and adolescents [33]. This type of Ph-like ALL usually associated with IKZF1 rearrangement [29, 35].
Other JAK/STAT pathways and RAS mutation
This subgroup represents 15–20% of Ph-like ALL; this group includes alteration of IL7R, SH2B3, JAK1, JAK3, IL2B, FLT3, TYK2, and mutation in RAS pathway (KRAS, NRAS, NF1, PTPN11) [17]. IKZF1 is less common in this subtype of Ph-like ALL than in other subgroups [36]. This subgroup has a better prognosis than other subgroups. RAS pathway mutations may arise in the other subtypes of ALL [17]. Moreover, there were rare rearrangements that had been identified like NTRK3, B-cell linker (BLNK), PTK2B, and TYK2 in Ph-like ALL [25]. These mutations are amenable to being targeted with different types of TKI [37]. A summary of the molecular and genetic pathways is illustrated in (Fig. 2).
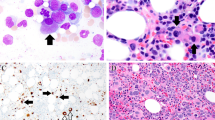
Summary of deregulated molecular pathways regulated in Ph-Like ALL. Caption: CRLF2 with IL-7Rα form heterodimeric receptor complex binds with its ligand TSLP. The signaling pathways observed in Ph-Like ALL including JAK/STAT pathway (involving CRLF2 overexpression with or without JAK2 mutation, IL-7Rα mutation, or EPOR rearrangements) might associate with IKZF1 deletion, ABL fusion signaling pathways, and RAS pathway or involve other kinases
Clinical presentation and outcomes of Ph-like ALL
BCR-ABL-like ALL belongs to the high-risk group of B-ALL in addition to KMT2A (MLL) translocations, low hypodiploidy (30–39 chromosomes), near haploidy (<30 chromosomes), BCR-ABL1, intrachromosomal amplification of chromosome 21 (iAMP21), t(17;19)/TCF3-HLF fusion, and complex karyotype [38, 39]. These groups have dismal prognoses despite modern chemotherapy regimens [22, 40].
The Ph-like ALL represents 10–15%, 20%, and 25–30% of childhood, adults (≥40 years), and adolescents and young adults (AYAs) (age 16–39 years) respectively; the frequency of each kinase subgroup varies with age [41, 42]. Many studies reported that this subtype, Ph-like ALL is usually associated with high white blood cell count (WBC), chemo-resistant, high minimal residual disease (MRD) level after induction therapy, high relapse rate, and short event-free (EFS) and overall survival (OS) [22, 41, 43, 44]. On the contrary, Herold et al. reported no significant differences in baseline patients’ characteristics, including age, sex, WBC count, hemoglobin, or platelet count between the BCR-ABL-like and other subtypes of B-ALL [45]. Also, Saleh LM et al. reported no significant difference in WBC, hemoglobin, platelet count, and sex in patients with higher CRLF2 expression compared to those with low CRLF2 expression [46]. Also, it has been observed that there is a higher incidence of Ph-like ALL in patients with Down syndrome (DS) than in non-Ph-like disease [47, 48].
Diagnostic approaches to Ph-like ALL
The National Comprehensive Cancer Network (NCCN) guideline version 2.2020 for ALL recommends the evaluation of recurrent genetic and molecular characterization of ALL by using karyotyping of G-banded chromosome analysis, FISH studies for the major recurrent genetic abnormalities, and RT-PCR for BCR-ABL1 (p190 and p210) [38]. In cases of BCR-ABL negative, additional testing is needed for gene fusions and other mutations associated with Ph-like ALL for better risk stratification and management [38]. Array comparative genomic hybridization (array CGH) may be needed if karyotyping failed or aneuploidy is detected [38]. Other methods for genetic characterization include low-density arrays (LDA), next-generation sequencing (NGS)–based assays, and multiplex RT-PCR which are typically used to detect signature or cryptic rearrangements and mutations characteristic of Ph-like ALL [49]. Although the evolution in the techniques of molecular and genetic analysis, there is still debate about the most appropriate approach for the diagnosis and screening of BCR-ABL like ALL. Identification of Ph-like ALL is challenging and usually diagnosed late after completion of induction protocol; major efforts should be done for early recognition of Ph-like ALL by the implementation of CRFL2 immunophenotyping tests and routine application of wide-spectrum, rapid FISH panels, and LDA to enhance therapeutic strategies by involving patients in a clinical trial to add target therapy to the treatment protocol [50].
LDA screening for all ALL patients allows rapid (within 48–72 h) identifying Ph-like ALL patients, those with LDA positive need further genetic testing by FISH or fusion analysis, and/or PCR. TSLPR (CRLF2) flow cytometry is highly cost-effective and can identify the patients within 24 h of specimen acquisition. As CRLF2 (TSLPR) is overexpressed in approximately half of Ph-like ALL cases, the TSLPR flow cytometry is now routinely included in the diagnostic workup of ALL patients. PCR mutation analysis to assess for JAK2, EPOR, IL-7Rα, and ABL class rearrangements and other rare Ph-like–associated alterations could be further tested [13, 25].
Recently, a predictive and statistical model based on Q-RT-PCR has evolved for the identification of Ph-like ALL cases [51, 52]. A stepwise simple diagnostic algorithm adopted from Yadav V et al. summarized the current Ph-like ALL genetic testing, illustrated in (Fig. 3) [53].
Current Ph-like ALL genetic testing algorithm. Adopted from Yadav et al. LDA screening for all B-ALL patients to rapidly identify those Ph-like ALL from those non-Ph-like ALL; these results are confirmed by FISH testing to rule out those with BCR-ABL1 and ETV6 RUNX1 rearrangements due to similarities in expression signatures; TSLPR flow cytometry immunophenotyping identify patients with overexpression CRLF2-R B-ALL. Confirmatory genetic testing by FISH, fusion analysis, and/or RT-PCR should be performed to characterize the specific CRLF2 alterations, JAK, IL-7Rα, EPOR, and ABL class rearrangements. Abbreviations: ALL, acute lymphoblastic leukemia ; FISH , fluorescence in situ hybridization; LDA, low-density array; Ph-like ALL, Philadelphia-like acute lymphoblastic leukemia; Ph-ve, Philadelphia-negative; Ph+ve, Philadelphia positive; RT-PCR, real-time polymerase chain reaction
Treatment approaches to Ph-like ALL
The poor outcome of patients with Ph-like ALL and the identification of actionable lesions have opened the way to the treatment of patients with genetic-driven approaches [37]. The NCCN panel recommends that pediatric and AYA patients with Ph-like ALL could be treated in a clinical trial when possible. In the absence of an appropriate clinical trial, the induction therapy consists of multiagent chemotherapy. Patients who have MRD negative after induction will continue risk-stratified therapy, while those with positive MRD after induction may undergo intensified consolidation therapy. If MRD remains persistent, other options include blinatumomab or chimeric antigen receptor (CAR) T-cell therapy tisagenlecleucel. In all cases, an allogeneic hematopoietic stem cell transplant (Allo-HSCT) may be considered part of consolidation or maintenance therapy [38]. A summary of clinical trials conducted on Ph-like ALL patients is illustrated in (Table 1).
Induction therapy and the significance of MRD
The induction of remission protocols in ALL usually involves the combination of 4 or 5 of the following drugs: anthracyclines, vincristine, cyclophosphamide, L/PEG-asparaginase, and steroids [17]. Differences between the protocols are in either dosing intensity, schedule, or the addition of 6-mercaptopurine, cytarabine, and rituximab [54, 55]. Based on the success of combining TKI with chemotherapy in cases of Ph + ALL, it raises the question about the validity of using the same approach in the ph like-ALL patients [33], especially since Ph-like ALL is 73 times more resistant to asparaginase and 1.6 times more resistant to daunorubicin and has poor sensitivity to glucocorticoids [6, 56]. In vitro and ex vivo data have reported sensitivity of ABL-class fusions to imatinib or dasatinib, while EPOR, JAK rearrangements, and other activating mutations of the JAK-STAT pathway can be effectively inhibited by JAK inhibitors such as ruxolitinib [57]. Other rare kinase alterations in Ph-like ALL can also be targeted by crizotinib, FAK inhibitors for NTRK3, PTK2B fusions, and TYK2 inhibitors for TYK2 fusions [29, 33].
However, among 148 adult B-ALL patients (including Ph-like, Ph-positive, and other B-ALL) treated with hyper-CVAD or augmented BFM (Berlin-Frankfurt-Munich) protocols with no specific intensification or modification for their high-risk ALL, in spite that CR rate was similar in the three studied groups, but MRD negativity was less achieved in the Ph-like ALL patients and translated to significantly worse overall survival (OS) and event-free survival compared to other B-ALL with a 5-year survival of 23% versus 59% for other B-ALL [23]. A new comprehensive study from the UK has suggested that the cutoff level for clinically relevant MRD is different for various genetic subtypes of ALL. Thus, it is reasonable to consider all Ph-like ALL patients as high risk, regardless of their MRD status [58]. Some data from 344 pediatric patients suggest that therapy intensification for Ph-like MRD+ patients can lead to MRD eradication and improve outcomes. However, confirmation from additional large studies is needed to adopt the best induction chemotherapy protocol to be used in those patients [10].
Although it is not specifically tested in the Ph-like ALL, the addition of rituximab if leukemic cells are CD20+ and the use of L- or PEG-asparaginase, known to be active in high-risk ALL, may be recommended [17]. At the same time, the risk of asparaginase-related complications at this age needs to be considered [59].
Blinatumomab, a bispecific antibody targeting CD19 and CD3, has not yet been tested as an agent for Ph-like ALL treatment intensification. However, it has been proven to be effective in MRD eradication and is currently being incorporated in clinical trials as part of front-line treatment for other high-risk ALL patients [60]. Furthermore, Meyer et al. observed that ALL with CRLF2 overexpression demonstrated suboptimal response to glucocorticoid in vitro, and this sensitivity might be augmented when MEK inhibitor trametinib and Akt inhibitor MK2206 combined with glucocorticoid but not the JAK inhibitor ruxolitinib [56]. Achieving MRD negativity is less likely in patients with Ph-like ALL, but the impact of persistent MRD and the intensification of therapy (including the use of Allo-HSCT) to deal with persistent MRD is not clear [44].
Role of target therapy
Targeting activated JAK-STAT signaling
The JAK1/2 inhibitor ruxolitinib is currently being studied in clinical trials for Ph-like ALL patients who have CRLF2 rearrangements or other JAK pathway alterations. Early-phase clinical trials have reported the safety and tolerability of combining JAK inhibitors with chemotherapy [37].
Koppikar et al. reported resistance to type 1 JAK inhibitors in CRLF2 rearranged B-ALL cells due to paradoxical hyperphosphorylation of JAK2 which produces a state of persistent JAK2 signaling. However, in contrast to JAK I inhibitors, type JAK II inhibitors stabilize JAK2 in the inactive conformation and overcome the JAK2 hyperphosphorylation observed with type I inhibitors, suggesting that type II JAK2 inhibition may be a more effective strategy to target CRLF2-rearranged B-ALLs. But high ruxolitinib doses of at least 50 mg twice daily might be needed to achieve clinical benefit [61, 62].
Meanwhile, the clinical benefit of the addition of ruxolitinib to chemotherapy in ALL is still questionable [33]; however, in the COG ADVL1011 phase 1 trial, the safety and tolerability of ruxolitinib monotherapy were demonstrated in children with multiply-relapsed/refractory cancers, and a recommended phase 2 dose of 50 mg/m2 twice daily for 28 days/cycle was identified [63]. Maude et al. reported poor response to single-agent ruxolitinib in preclinical sitting [64], but in further studies conducted by Bӧhm et al., ruxolitinib enhanced the in vivo efficacy of an induction regimen consisting of vincristine, dexamethasone, and L-asparaginase in CRLF2-rearranged Ph-like ALL xenografts [57].
Phase II studies exploring the role of incorporating ruxolitinib in induction regimens for Ph-like ALL are still ongoing (NCT03117751, NCT03571321, NCT02723994, and NCT02420717) [65,66,67]. CHZ868 is a type 2 JAK inhibitor molecule, investigated in mouse models of CRLF2-rearranged B-ALL; it could induce apoptosis and improve survival in those models [68].
In addition, recent studies showed strong effects of combinatorial treatment with JAK1/JAK2 and PI3K/mTOR inhibitors. In patient-derived Ph-like ALL murine xenograft models, cotreatment with PI3K/mTOR inhibitor gedatolisib and ruxolitinib and gedatolisib and dasatinib had superior efficacy than any of the agents alone [37]. Similarly, the combination of next-generation inhibitors such as type II JAK inhibitor (NVP-BBT594) and second-generation mTOR inhibitor (AZD2014) induced robust anti-leukemic effects in Ph-like ALL cell lines and PDX models harboring CRLF2 rearrangements ±JAK mutations [69].
The cell surface expression of CRLF2/TSLPR, which forms a functional heterodimeric complex with IL7R, is also being exploited for immunotherapeutic targeting with the development of anti-CRLF2/TSLPR antibodies and TSLPR-directed CAR-T cell therapy [70].
Targeting ABL-class fusions
For the Ph-like patients presenting with ABL rearrangements, data are suggesting that inhibition by BCR/ABL-specific TKI may be beneficial [17, 32]. It had been reported a sustained response of Ph-like ALL patients with ABL-class fusions to imatinib or dasatinib, particularly those harboring rearrangements of PDGFRB, which is associated with induction failure and a dismal outcome [71].
In the COG AALL1131 (NCT02883049) trial, dasatinib was tested in patients with confirmed ABL-class alteration, daily dasatinib was added to augmented BFM-based chemotherapy at the start of consolidation and continued until the end of maintenance therapy, and the results are still awaited [49]. Moreover, interim data analysis of phase 1/2 study conducted at MDACC reported the safety and efficacy of adding dasatinib to hyper-CVAD chemotherapy in adolescents and adults with relapsed/refractory Ph-like ALL and ABL class fusions (NCT02420717 ) without identified dose-limiting toxicity [13, 72].
Although there is no high-level evidence regarding the value of TKI in patients who have ABL rearrangement, given the established safety and efficacy of these drugs in Ph-positive ALL patients, off-label TKI use could be considered in the treatment of Ph-like ALL than the use of JAK inhibitors in patients harbor JAK rearrangements [17].
Targeting NTKR3 fusions
One uncommon but recurrent alteration identified in approximately 1% of Ph-like ALL is ETV6-NTRK3. TRK fusions have been identified in breast carcinoma, infantile sarcoma, acute myeloid leukemia, and more recently pediatric glioma [73]. In vitro and in vivo treatment with the TRK inhibitor larotrectinib demonstrated specific and durable reduction of leukemic burden below detectable levels [74]. Larotrectinib received Food and Drug Administration (FDA) approval in 2018 for the treatment of adult and pediatric patients with solid tumors that have an NTRK gene fusion [75]. Nardi et al. reported a substantial response by using larotrectinib in a refractory Ph-like ALL patients harboring NRAS mutation and ETV6-NTRK3 rearrangement after the failure of CAR T cell therapy [76]. Thus, screening for ETV6- NTRK3 in newly diagnosed ALL and testing the clinical efficacy of TRK inhibition should be considered [77, 78].
Targeting Ras/MAPK pathway alterations
Up to 6% of patients with Ph-like ALL have mutations in the Ras/MAPK signaling pathway as their main abnormality [29]. For Ph-like ALL with Ras mutations, Ras inhibition failed, as it is impossible to inhibit Ras directly, but targeting the Ras pathway downstream effectors such as MEK inhibitors represents a new therapeutic strategy [33].
Targeting SMAC (apoptotic regulator)
Birinapant, a small molecule mimetic of the apoptotic regulator (SMAC), acts as a mitochondria-derived activator of caspase (SMAC) mimetics targeting inhibitor of apoptosis proteins which activates cell death pathways [79]. Birinapant enhanced the antileukemic activity both as a single agent or in combination with an induction-type regimen of vincristine, dexamethasone, and L-asparaginase against Ph-like ALL xenografts; it was found that chemo-resistant Ph-like leukemic cells were acutely sensitive to Birinapant [80].
Role of hematopoietic stem cell transplantation based on MRD status
The benefit of allogeneic hematopoietic stem cell transplantation (Allo-HSCT) is outbalanced by the high therapy-related mortality associated with the procedure. So, the appropriate selection of patients with high relapse risk and the lowest risk of transplant-related complications is important. As such, because Ph-like patients are associated with a high risk of relapse, Allo-HSCT might be of value as a consolidation modality for these patients, especially in patients who expected to have a low risk of transplant-related complications. However, there is insufficient data on the outcomes of Allo-HSCT for Ph-like ALL, and it remains debatable whether all adult Ph-like ALL patients should receive an allogeneic HSCT in the first CR, irrespective of other indications So far, no recommendations on the use Allo- HSCT have been established in Ph-like ALL patients in the CR1 [44, 81].
Robert et al. reported no difference in the outcome of Ph-like patients treated with intensified consolidation (including Allo-HSCT) and non–Ph-like pediatric or adult patients [10, 41]. Cho H et.al. reported that Ph-like ALL patients who received Allo-HSCT after CR1 were not inferior in relapse rate, DFS, and OS compared to standard risk ALL but had better relapse rate, DFS, and OS compared to other poor risk cytogenetics ALL [82]. However, in a more recent Chinese retrospective study, the overall response rate of Allo-HSCT after 1 month of TKI was 100% compared to 62% and 73% after 1 month of TKI treatment combined with chemotherapy, and CAR-T cell therapy respectively. Moreover, Allo-HSCT is associated with better DFS and OS compared to CAR-T cell therapy in univariate analysis [83].
MRD positivity after the induction therapy is associated with worse survival and a high risk of relapse in patients with Ph-like ALL as well as other types of ALL [84]. Allogeneic SCT is strongly recommended in this setting [85]. Furthermore, no difference in overall survival in ALL patients who achieved MRD negativity at the end of the induction protocol whatever its type (i.e., in Ph-positive, Ph-like, Ph-negative ALL); also, there were no statistically significant differences in outcomes between the three previous groups after Allo-HCT in CR1 [84, 86] that endorse the significance of MRD negativity exceed the cytogenetic risk group [86, 87].
However, since the results of Allo-HSCT are superior in patients who are MRD-negative before the transplant, intensification of therapy aiming to eradicate the residual disease is logical even before allogeneic HSCT [88]. Remarkably, patients with Ph-like ALL are more likely to still be MRD-positive at the end of the induction protocol [84, 86]. FDA specifically approved the use of blinatumomab for high-risk B-ALL patients who achieve remission but remain MRD positive. In a prospective trial, MRD was eliminated in 78% of patients following blinatumomab. Poor outcome was reported in ALL patients above 15 years old, who were MRD positive after the initial therapy and receive no blinatumomab before allogeneic HSCT, which was confirmed in a large European retrospective analysis [89]. Despite that the previous trials did not screen for Ph-like ALL, it is assumed that blinatumomab could have similar efficacy in Ph-like ALL [90].
Several reports demonstrated complete eradication or significant reduction of MRD at the time of Allo HSCT resulting from pre-transplant intensification with ruxolitinib [67]. However, the addition of targeted therapy, such as JAK or BCR/ABL inhibitors, should not substitute MRD eradication with blinatumomab or intensive chemotherapy before transplantation. Currently, no data are available to support maintenance with JAK2 inhibitors following allogeneic SCT in Ph-like ALL patients [67]. For patients with Ph-like ALL who carry an ABL rearrangement, the addition of post-transplant TKI maintenance is still questionable because of the rarity of this condition. However, safety data of post-transplant TKI maintenance can be extrapolated from the Ph-positive ALL, and its use could be encouraged [91]. This is in agreement with what was reported by Niswander et al., as they reported a substantial response to the addition of ruxolitinib or ponatinib to post-induction chemotherapy; one patient achieved MRD-negative remission by adding ponatinib to blinatumomab and then underwent Allo-HSCT followed by 2 years of maintenance ponatinib posttransplant [66].
Persistence of MRD even after allogeneic SCT or failure to eradicate it before transplantation is a poor prognostic marker and a sign of impending relapse. In these circumstances, patients should be aggressively treated with intensive therapy, and CAR T-cell therapy should be considered. A clinical trial with focal adhesion kinase (FAK) inhibitors could be an appropriate option for patients with IKZF1 mutations or deletions [92].
However, due to the lack of evidence supporting routine assignment to allogeneic SCT, a recent expert review and recommendations from the European Working Group for Adult Acute Lymphoblastic Leukemia (EWALL) and the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation (EBMT) recommended the use of allogeneic SCT during first complete remission only in MRD-positive pediatric and adult patients with Ph-like ALL [93].
Notably, a higher rate of relapse is observed in adult Ph-like ALL patients even in MRD-negative cases than in pediatric patients with identical MRD kinetics of eradication. Therefore, Allo-HSCT should be considered in adult Ph-like ALL patients especially those with IKZF1 alteration or other high-risk alterations even if they achieve molecular remission [94].
EL Fakih et al. suggested an algorithm on when to consider Allo-HSCT for Ph-like ALL patients, illustrated in (Fig. 4) [44].
Proposed algorithm by El Fakih et al. to address the role of allogenic bone marrow transplant in the Ph-like ALL patient. Adopted with his permission from El Fakih et al. [44]
Management of relapsed patients
In CD19+ ALL, blinatumomab is an acceptable option for both adult and pediatric patients. Inotuzumab ozogamicin (InO) is a humanized anti-CD22 monoclonal antibody also an accepted option for adult patients. CAR T-cell therapy is a powerful strategy to be used in such high-risk patients followed by Allo-HSCT [95]. Combining blinatumomab with inotuzumab is also a good option but should be evaluated against the risk of developing the veno-occlusive disease during subsequent Allo-HSCT [96]. A phase I study by Pullarkat et al. used venetoclax (selective BCL2 inhibitor), with low-dose navitoclax, a BCL-XL/BCL2 inhibitor, in combination with chemotherapy in relapsed/refractory ALL patients, and reported promising outcomes within all genomic subtypes, although in Ph-like and Ph-positive ALL, responses were fewer. The complete remission rate was 60%, including responses in patients who had previously undergone Allo-HSCT or received immunotherapy [97]. A recently published trial conducted by Dai et al. investigated CAR T-cell therapy followed by allogeneic stem cell transplantation, and they reported that the response rate was 94.1%; MRD negative CR was achieved in 11 out of 17 patients, with estimated rates of 3-year overall survival (65.9%±16.5%); the results were comparable in among the included Ph-like, Ph+, and other B-ALL groups [98].
Management of old age patients
Although Ph-like ALL was reported in 24% of ALL patients over the age of 65 in the USA, no prospective studies have included these patients. On the other hand, Herold et al. showed that the incidence of Ph-like ALL decreased significantly with more advanced age [99].
Unfortunately, for most patients with advanced age, prolonged intensive chemotherapy followed by Allo-HSCT is not feasible [100].
In a study conducted at MD Anderson Cancer Center on a group of 52 patients with a median age of 68 years, inotuzumab ozogamicin was used instead of a significant portion of chemotherapy, creating a less toxic first-line regimen. The 2-year progression-free survival (PFS) was 59% [101].
Conclusion
Ph-like ALL is one of the high-risk ALL, characterized by a high relapse rate, short event-free, and overall survival. Accurate and rapid identification of these patients is critical to determine the treatment plan. The inclusion of those patients in clinical trials should be encouraged to better understand the benefit of the addition of TKI to the induction treatment protocol. The role of allogeneic bone marrow transplant in Ph-like All in CR1 is still unclear; however, this decision should be tailored according to MRD status.
Data availability
This is a comprehensive review, extensive electronic search on google scholar, Pubmed, Medline, and Egyptian Knowledge Bank done using the keywords and all the available data in the literature.
Abbreviations
- ALL :
-
acute lymphoblastic leukemia
- Ph-like :
-
Philadelphia chromosome-like
- TKI :
-
tyrosine kinase inhibitor
- BCR :
-
breakpoint cluster region gene
- ABL :
-
Abelson proto-oncogene
- Allo-HSCT :
-
allogenic hematopoietic stem cell transplant
- KMT2A :
-
histone-lysine methyltransferase 2
- TCF3 :
-
transcription factor 3
- TSLP :
-
thymic stromal lymphopoietin receptor
- PB X1 :
-
pre-B-cell-leukemia transcription factor 1
- CRLF2 :
-
cytokine receptor-like factor 2 receptor
- IKZF 1 :
-
IKAROS family zinc finger 1
- PDGFRB :
-
platelet-derived growth factor B
- MRD :
-
minimal residual disease
- EPOR :
-
erythropoietin receptor rearrangements
- JAK2 :
-
Janus kinase 2
- WBC :
-
white blood cell count
- EFS :
-
event-free survival
- OS :
-
overall survival
- DS :
-
Down syndrome
- NCCN :
-
National Comprehensive Cancer Network
- LDA :
-
low-density arrays
- NGS :
-
next-generation sequencing
- FISH :
-
fluorescence in situ hybridization
- RT-PCR :
-
real-time polymerase chain reaction
- CAR-T :
-
chimeric antigen receptor (CAR) T-cell therapy
References
Lee JW, Cho B (2017) Prognostic factors and treatment of pediatric acute lymphoblastic leukemia. Korean J Pediatr 60(5):129
Kang Z-J, Liu Y-F, Xu L-Z, Long Z-J, Huang D, Yang Y et al (2016) The Philadelphia chromosome in leukemogenesis. Chin J Cancer 35(1):48
Owattanapanich W, Rujirachun P, Ungprasert P, Buaboonnam J, Techavichit P (2020) Prevalence and clinical outcome of philadelphia-like acute lymphoblastic leukemia: systematic review and meta-analysis. Clin Lymphoma Myeloma Leuk 20(1):e22–ee9
van Rhee F, Hochhaus A, Lin F, Melo J, Goldman J, Cross N (1996) p190 BCR-ABL mRNA is expressed at low levels in p210-positive chronic myeloid and acute lymphoblastic leukemias. Blood 87(12):5213–5217
Melo J (1996) The diversity of BCR-ABL fusion proteins and their relationship to leukemia phenotype. Blood 88(7):2375–2384
Den Boer ML, van Slegtenhorst M, De Menezes RX, Cheok MH, Buijs-Gladdines JG, Peters ST et al (2009) A subtype of childhood acute lymphoblastic leukaemia with poor treatment outcome: a genome-wide classification study. Lancet Oncol 10(2):125–134
Haferlach T, Kohlmann A, Schnittger S, Dugas M, Hiddemann W, Kern W et al (2005) Global approach to the diagnosis of leukemia using gene expression profiling. Blood 106(4):1189–1198
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127(20):2391–2405
Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo KR, Kvasnicka H-M et al (2022) International consensus classification of myeloid neoplasms and acute leukemias: integrating morphologic, clinical, and genomic data. Blood, J Am Soc Hematol 140(11):1200–1228
Roberts KG, Pei D, Campana D, Payne-Turner D, Li Y, Cheng C et al (2014) Outcomes of children with BCR-ABL1–like acute lymphoblastic leukemia treated with risk-directed therapy based on the levels of minimal residual disease. J Clin Oncol 32(27):3012
Roberts KG, Morin RD, Zhang J, Hirst M, Zhao Y, Su X et al (2012) Genetic alterations activating kinase and cytokine receptor signaling in high-risk acute lymphoblastic leukemia. Cancer Cell 22(2):153–166
Roberts KG (2017) The biology of Philadelphia chromosome-like ALL. Best Pract Res Clin Haematol 30(3):212–221
Harvey RC, Tasian SK (2020) Clinical diagnostics and treatment strategies for Philadelphia chromosome–like acute lymphoblastic leukemia. Blood Adv 4(1):218–228
Tran TH, Loh ML (2016) Ph-like acute lymphoblastic leukemia. Hematology 2016(1):561–566
Jain S, Abraham A (2020) BCR-ABL1–like B-acute lymphoblastic leukemia/lymphoma: a comprehensive review. Arch Pathol Lab Med 144(2):150–155
Russell LJ, Capasso M, Vater I, Akasaka T, Bernard OA, Calasanz MJ et al (2009) Deregulated expression of cytokine receptor gene, CRLF2, is involved in lymphoid transformation in B-cell precursor acute lymphoblastic leukemia. Blood, J Am Soc Hematol 114(13):2688–2698
Frisch A, Ofran Y (2019) How I diagnose and manage Philadelphia chromosome-like acute lymphoblastic leukemia. Haematologica 104(11):2135
Chiaretti S, Brugnoletti F, Messina M, Paoloni F, Fedullo AL, Piciocchi A et al (2016) CRLF2 overexpression identifies an unfavourable subgroup of adult B-cell precursor acute lymphoblastic leukemia lacking recurrent genetic abnormalities. Leuk Res 41:36–42
Martínez-Anaya D, Moreno-Lorenzana D, Reyes-León A, Juárez-Figueroa U, Dean M, Aguilar-Hernández MM et al (2022) Characterization of Philadelphia-like pre-b acute lymphoblastic leukemia: experiences in Mexican pediatric patients. Int J Mol Sci 23(17):9587
Palmi C, Vendramini E, Silvestri D, Longinotti G, Frison D, Cario G et al (2012) Poor prognosis for P2RY8-CRLF2 fusion but not for CRLF2 over-expression in children with intermediate risk B-cell precursor acute lymphoblastic leukemia. Leukemia 26(10):2245–2253
Chiaretti S, Messina M, Foà R (2019) BCR/ABL1–like acute lymphoblastic leukemia: how to diagnose and treat? Cancer 125(2):194–204
Tasian SK, Loh ML, Hunger SP (2017) Philadelphia chromosome–like acute lymphoblastic leukemia. Blood, J Am Soc Hematol 130(19):2064–2072
Jain N, Roberts KG, Jabbour E, Patel K, Eterovic AK, Chen K et al (2017) Ph-like acute lymphoblastic leukemia: a high-risk subtype in adults. Blood, J Am Soc Hematol 129(5):572–581
Ge Z, Gu Y, Zhao G, Li J, Chen B, Han Q et al (2016) High CRLF2 expression associates with IKZF1 dysfunction in adult acute lymphoblastic leukemia without CRLF2 rearrangement. Oncotarget 7(31):49722
Shiraz P, Payne KJ, Muffly L (2020) The current genomic and molecular landscape of Philadelphia-like acute lymphoblastic leukemia. Int J Mol Sci 21(6):2193
Perez-Andreu V, Roberts KG, Harvey RC, Yang W, Cheng C, Pei D et al (2013) Inherited GATA3 variants are associated with Ph-like childhood acute lymphoblastic leukemia and risk of relapse. Nat Genet 45(12):1494
Jain N, Zhang H, Roberts KG, Qian M, Yang W, Jabbour EJ et al (2017) GATA3 rs3824662A allele is overrepresented in adult patients with Ph-like ALL, especially in patients with CRLF2 abnormalities. Blood 130:1430
Mosaad YM, Elashery R, Darwish A, Sharaf Eldein OA, Barakat T, Marouf S et al (2017) GATA3 rs3824662 gene polymorphism as possible risk factor in a cohort of Egyptian patients with pediatric acute lymphoblastic leukemia and its prognostic impact. Leuk Lymphoma 58(3):689–698
Roberts KG, Li Y, Payne-Turner D, Harvey RC, Yang Y-L, Pei D et al (2014) Targetable kinase-activating lesions in Ph-like acute lymphoblastic leukemia. N Engl J Med 371(11):1005–1015
Boer JM, Marchante J, Boeree A, Escherich G, de Groot-Kruseman H, Pieters R et al (2015) Tyrosine kinase fusion genes in pediatric BCR-ABL1-like acute lymphoblastic leukemia. Haematologica 100(Suppl 1):156
Schwab C, Enshaei A, Roberts KG, Russell LJ, Harvey RC, Chen I-ML et al (2016) The frequency and outcome of Ph-like ALL associated abnormalities in childhood acute lymphoblastic leukaemia treated on MRC UKALL2003. American Society of Hematology, Washington, DC
Zhang Y, Gao Y, Zhang H, Zhang J, He F, Hnízda A et al (2018) PDGFRB mutation and tyrosine kinase inhibitor resistance in Ph-like acute lymphoblastic leukemia. Blood, J Am Soc Hematol 131(20):2256–2261
Khan M, Siddiqi R, Tran TH (eds) (2018) Philadelphia chromosome-like acute lymphoblastic leukemia: a review of the genetic basis, clinical features, and therapeutic options. Seminars in Hematology 55(4):235–241. WB Saunders
Mullighan CG (2014) The genomic landscape of acute lymphoblastic leukemia in children and young adults. Hematology 2014(1):174–180
van der Veer A, Waanders E, Pieters R, Willemse ME, Van Reijmersdal SV, Russell LJ et al (2013) Independent prognostic value of BCR-ABL1-like signature and IKZF1 deletion, but not high CRLF2 expression, in children with B-cell precursor ALL. Blood, J Am Soc Hematol 122(15):2622–2629
Boer JM, Steeghs EM, Marchante JR, Boeree A, Beaudoin JJ, Beverloo HB et al (2017) Tyrosine kinase fusion genes in pediatric BCR-ABL1-like acute lymphoblastic leukemia. Oncotarget 8(3):4618
Tasian SK, Teachey DT, Li Y, Shen F, Harvey RC, Chen I-M et al (2017) Potent efficacy of combined PI3K/mTOR and JAK or ABL inhibition in murine xenograft models of Ph-like acute lymphoblastic leukemia. Blood, J Am Soc Hematol 129(2):177–187
Brown P, Inaba H, Annesley C, Beck J, Colace S, Dallas M et al (2020) Pediatric acute lymphoblastic leukemia, version 2.2020, nccn clinical practice guidelines in oncology. J Natl Compr Cancer Netw 18(1):81–112
Carobolante F, Chiaretti S, Skert C, Bassan R (2020) Practical guidance for the management of acute lymphoblastic leukemia in the adolescent and young adult population. Ther Adv Hematol 11:2040620720903531
Mullighan CG (2013) Genomic characterization of childhood acute lymphoblastic leukemia. Seminars in hematology 50(4):314–324. WB Saunders
Roberts KG, Gu Z, Payne-Turner D, McCastlain K, Harvey RC, Chen I-M et al (2017) High frequency and poor outcome of Philadelphia chromosome–like acute lymphoblastic leukemia in adults. J Clin Oncol 35(4):394
Roberts KG, Reshmi SC, Harvey RC, Chen I-M, Patel K, Stonerock E et al (2018) Genomic and outcome analyses of Ph-like ALL in NCI standard-risk patients: a report from the Children’s Oncology Group. Blood, J Am Soc Hematol 132(8):815–824
Roberts KG, Yang Y-L, Payne-Turner D, Lin W, Files JK, Dickerson K et al (2017) Oncogenic role and therapeutic targeting of ABL-class and JAK-STAT activating kinase alterations in Ph-like ALL. Blood Adv 1(20):1657–1671
El Fakih R, Savani B, Mohty M, Aljurf M (2020) Hematopoietic cell transplant consideration for Philadelphia chromosome–like acute lymphoblastic leukemia patients. Biol Blood Marrow Transplant 26(1):e16–e20
Herold T, Schneider S, Metzeler KH, Neumann M, Hartmann L, Roberts KG et al (2017) Adults with Philadelphia chromosome–like acute lymphoblastic leukemia frequently have IGH-CRLF2 and JAK2 mutations, persistence of minimal residual disease and poor prognosis. Haematologica 102(1):130–138
Saleh LM, Darwish N, Abdel-Aziz S, Salem D, Eisa N, Abd El Mabood S et al (2021) High CRLF2 expression could identify acute lymphoblastic leukemia patients with poor outcome but not IKZF1. Res Oncol 17(1):23–30
Imamura T, Kiyokawa N, Kato M, Imai C, Okamoto Y, Yano M et al (2016) Characterization of pediatric Philadelphia-negative B-cell precursor acute lymphoblastic leukemia with kinase fusions in Japan. Blood Cancer J 6(5):e419
Loh ML, Zhang J, Harvey RC, Roberts K, Payne-Turner D, Kang H et al (2013) Tyrosine kinome sequencing of pediatric acute lymphoblastic leukemia: a report from the Children’s Oncology Group TARGET Project. Blood, J Am Soc Hematol 121(3):485–488
Inaba H, Azzato EM, Mullighan CG (2017) Integration of next-generation sequencing to treat acute lymphoblastic leukemia with targetable lesions: the St Jude children’s research hospital approach. Front Pediatr 5:258
Ribera J-M (2021) Philadelphia chromosome-like acute lymphoblastic leukemia still a pending matter. Haematologica 106(6):1514
Chiaretti S, Messina M, Grammatico S, Piciocchi A, Fedullo AL, Di Giacomo F et al (2018) Rapid identification of BCR/ABL 1-like acute lymphoblastic leukaemia patients using a predictive statistical model based on quantitative real time-polymerase chain reaction: clinical, prognostic and therapeutic implications. Br J Haematol 181(5):642–652
Cardinali D, Della Starza I, Bellomarino V, Beldinanzi M, Di Trani M, Ferrara F et al (2022) Dissecting Ph-like ALL: the role of genomic lesion and minimal residual disease in refining outcome. Blood 140(Supplement 1):6350–6351
Yadav V, Ganesan P, Veeramani R, Kumar D (2021) Philadelphia-like acute lymphoblastic leukemia: a systematic review. Clin Lymphoma Myeloma Leuk 21(1):e57–e65
El-Cheikh J, El Dika I, Massoud R, Charafeddine M, Mahfouz R, Kharfan-Dabaja MA et al (2017) Hyper-CVAD compared with BFM-like chemotherapy for the treatment of adult acute lymphoblastic leukemia. A retrospective single-center analysis. Clin Lymphoma Myeloma Leuk 17(3):179–185
Erkut N, Akidan O, Batur DS, Karabacak V, Sonmez M (2018) Comparison between Hyper-CVAD and PETHEMA ALL-93 in adult acute lymphoblastic leukemia: a single-center study. Chemotherapy 63(4):207–213
Meyer LK, Delgado-Martin C, Maude SL, Shannon KM, Teachey DT, Hermiston ML (2019) CRLF2 rearrangement in Ph-like acute lymphoblastic leukemia predicts relative glucocorticoid resistance that is overcome with MEK or Akt inhibition. PLoS One 14(7):e0220026
Bӧhm JW, Sia K, Jones C, Evans K, Mariana A, Pang I et al (2021) Combination efficacy of ruxolitinib with standard-of-care drugs in CRLF2-rearranged Ph-like acute lymphoblastic leukemia. Leukemia 35(11):3101–3112
O’Connor D, Enshaei A, Bartram J, Hancock J, Harrison CJ, Hough R et al (2018) Genotype-specific minimal residual disease interpretation improves stratification in pediatric acute lymphoblastic leukemia. J Clin Oncol 36(1):34
Maury S, Chevret S, Thomas X, Heim D, Leguay T, Huguet F et al (2016) Rituximab in B-lineage adult acute lymphoblastic leukemia. N Engl J Med 375(11):1044–1053
Kantarjian H, Jabbour E, Topp MS (2017) Blinatumomab for acute lymphoblastic leukemia. N Engl J Med 376(23):e49
Koppikar P, Bhagwat N, Kilpivaara O, Manshouri T, Adli M, Hricik T et al (2012) Heterodimeric JAK–STAT activation as a mechanism of persistence to JAK2 inhibitor therapy. Nature 489(7414):155–159
Tasian SK, Assad A, Hunter DS, Du Y, Loh ML (2018) A phase 2 study of ruxolitinib with chemotherapy in children with Philadelphia chromosome-like acute lymphoblastic leukemia (INCB18424-269/AALL1521): dose-finding results from the part 1 safety phase. Blood 132:555
Loh ML, Tasian SK, Rabin KR, Brown P, Magoon D, Reid JM et al (2015) A phase 1 dosing study of ruxolitinib in children with relapsed or refractory solid tumors, leukemias, or myeloproliferative neoplasms: a Children’s Oncology Group phase 1 consortium study (ADVL1011). Pediatr Blood Cancer 62(10):1717–1724
Maude SL, Tasian SK, Vincent T, Hall JW, Sheen C, Roberts KG et al (2012) Targeting JAK1/2 and mTOR in murine xenograft models of Ph-like acute lymphoblastic leukemia. Blood, J Am Soc Hematol 120(17):3510–3518
Mayfield JR, Czuchlewski DR, Gale JM, Matlawska-Wasowska K, Vasef MA, Nickl C et al (2017) Integration of ruxolitinib into dose-intensified therapy targeted against a novel JAK2 F694L mutation in B-precursor acute lymphoblastic leukemia. Pediatr Blood Cancer 64(5):e26328
Niswander LM, Loftus JP, Lainey É, Caye-Eude A, Pondrom M, Hottman DA et al (2021) Therapeutic potential of ruxolitinib and ponatinib in patients with EPOR-rearranged Philadelphia chromosome-like acute lymphoblastic leukemia. Haematologica 106(10):2763
Ding YY, Stern JW, Jubelirer TF, Wertheim GB, Lin F, Chang F et al (2018) Clinical efficacy of ruxolitinib and chemotherapy in a child with Philadelphia chromosome-like acute lymphoblastic leukemia with GOLGA5-JAK2 fusion and induction failure. Haematologica 103(9):e427
Wu S-C, Li LS, Kopp N, Montero J, Chapuy B, Yoda A et al (2015) Activity of the type II JAK2 inhibitor CHZ868 in B cell acute lymphoblastic leukemia. Cancer Cell 28(1):29–41
Zhang Q, Shi C, Han L, Jain N, Roberts KG, Ma H et al (2018) Inhibition of mTORC1/C2 signaling improves anti-leukemia efficacy of JAK/STAT blockade in CRLF2 rearranged and/or JAK driven Philadelphia chromosome–like acute B-cell lymphoblastic leukemia. Oncotarget 9(8):8027
Verstraete K, Peelman F, Braun H, Lopez J, Van Rompaey D, Dansercoer A et al (2017) Structure and antagonism of the receptor complex mediated by human TSLP in allergy and asthma. Nat Commun 8(1):1–17
Schwab C, Ryan SL, Chilton L, Elliott A, Murray J, Richardson S et al (2016) EBF1-PDGFRB fusion in pediatric B-cell precursor acute lymphoblastic leukemia (BCP-ALL): genetic profile and clinical implications. Blood, J Am Soc Hematol 127(18):2214–2218
Jain N, Jabbour EJ, McKay PZ, Ravandi F, Takahashi K, Kadia T et al (2017) Ruxolitinib or dasatinib in combination with chemotherapy for patients with relapsed/refractory Philadelphia (Ph)-like acute lymphoblastic leukemia: a phase I-II trial. Blood 130:1322
Penault-Llorca F, Rudzinski ER, Sepulveda AR (2019) Testing algorithm for identification of patients with TRK fusion cancer. J Clin Pathol 72(7):460–467
Joshi SK, Davare MA, Druker BJ, Tognon CE (2019) Revisiting NTRKs as an emerging oncogene in hematological malignancies. Leukemia 33(11):2563–2574
Scott LJ (2019) Larotrectinib: first global approval. Drugs 79(2):201–206
Nardi V, Ku N, Frigault MJ, Dubuc AM, Tsai HK, Amrein PC et al (2020) Clinical response to larotrectinib in adult Philadelphia chromosome–like ALL with cryptic ETV6-NTRK3 rearrangement. Blood Adv 4(1):106–111
Roberts KG, Janke LJ, Zhao Y, Seth A, Ma J, Finkelstein D et al (2018) ETV6-NTRK3 induces aggressive acute lymphoblastic leukemia highly sensitive to selective TRK inhibition. Blood, J Am Soc Hematol 132(8):861–865
Hsiao SJ, Zehir A, Sireci AN, Aisner DL (2019) Detection of tumor NTRK gene fusions to identify patients who may benefit from tyrosine kinase (TRK) inhibitor therapy. J Mol Diagn 21(4):553–571
Krepler C, Chunduru SK, Halloran MB, He X, Xiao M, Vultur A et al (2013) The novel SMAC mimetic birinapant exhibits potent activity against human melanoma cells The SMAC Mimetic Birinapant Exhibits Potent Antimelanoma Activity. Clin Cancer Res 19(7):1784–1794
Richmond J, Robbins A, Evans K, Beck D, Kurmasheva RT, Billups CA et al (2016) Acute sensitivity of Ph-like acute lymphoblastic leukemia to the SMAC-mimetic birinapant. Cancer Res 76(15):4579–4591
Płotka A, Lewandowski K (2022) BCR/ABL1-like acute lymphoblastic leukemia: from diagnostic approaches to molecularly targeted therapy. Acta Haematol 145(2):122–131
Cho H, Kim Y, Yoon J-H, Lee J, Lee GD, Son J et al (2021) Non-inferior long-term outcomes of adults with Philadelphia chromosome-like acute lymphoblastic leukemia. Bone Marrow Transplant 56(8):1953–1963
Xu G-f, Liu L-m, Wang M, Zhang Z-b, Xie J-d, Qiu H-y et al (2022) Treatments of Ph-like acute lymphoblastic leukemia: a real-world retrospective analysis from a single large center in China. Leuk Lymphoma 63:1–11
Abdel-Rahman ZH, Heckman MG, Anagnostou T, White LJ, Kloft-Nelson SM, Knudson RA et al (2021) Identification of adult Philadelphia-like acute lymphoblastic leukemia using a FISH-based algorithm distinguishes prognostic groups and outcomes. Blood Cancer J 11(9):1–4
Anagnostou T, Maloy MA, Patnaik MM, Arcila ME, Arteaga AG, Cho C et al (2020) Transplant characteristics and outcomes of Philadelphia (Ph)-like acute lymphoblastic leukemia (ALL). Biol Blood Marrow Transplant 26(3):S114–S1S5
Chiaretti S, Messina M, Della Starza I, Piciocchi A, Cafforio L, Cavalli M et al (2021) Philadelphia-like acute lymphoblastic leukemia is associated with minimal residual disease persistence and poor outcome first report of the minimal residual disease-oriented GIMEMA LAL1913. Haematologica 106(6):1559
Della Starza I, Chiaretti S, De Propris MS, Elia L, Cavalli M, De Novi LA et al (2019) Minimal residual disease in acute lymphoblastic leukemia: technical and clinical advances. Front Oncol 9:726
Seibel NL, Steinherz PG, Sather HN, Nachman JB, DeLaat C, Ettinger LJ et al (2008) Early postinduction intensification therapy improves survival for children and adolescents with high-risk acute lymphoblastic leukemia: a report from the Children’s Oncology Group. Blood, J Am Soc Hematol 111(5):2548–2555
Gökbuget N, Dombret H, Giebel S, Bruggemann M, Doubek M, Foà R et al (2019) Minimal residual disease level predicts outcome in adults with Ph-negative B-precursor acute lymphoblastic leukemia. Hematology 24(1):337–348
Tran TH, Tasian SK (2022) Treatment of Ph-like acute lymphoblastic leukemia. Clinical Management of Acute Lymphoblastic Leukemia. Springer, pp 209–234
Zhang G, Zhang Y, Wu J, Chen Y, Ma Z (2017) Acute lymphoblastic leukemia patient with variant ATF7IP/PDGFRB fusion and favorable response to tyrosine kinase inhibitor treatment: a case report. Am J Case Rep 18:1204
Kurmasheva RT, Gorlick R, Kolb EA, Keir ST, Maris JM, Lock RB et al (2017) Initial testing of VS-4718, a novel inhibitor of focal adhesion kinase (FAK), against pediatric tumor models by the Pediatric Preclinical Testing Program. Pediatr Blood Cancer 64(4):e26304
Giebel S, Marks DI, Boissel N, Baron F, Chiaretti S, Ciceri F et al (2019) Hematopoietic stem cell transplantation for adults with Philadelphia chromosome-negative acute lymphoblastic leukemia in first remission: a position statement of the European Working Group for Adult Acute Lymphoblastic Leukemia (EWALL) and the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant 54(6):798–809
Li J-F, Dai Y-T, Lilljebjörn H, Shen S-H, Cui B-W, Bai L et al (2018) Transcriptional landscape of B cell precursor acute lymphoblastic leukemia based on an international study of 1,223 cases. Proc Natl Acad Sci 115(50):E11711–E11E20
Park JH, Rivière I, Gonen M, Wang X, Sénéchal B, Curran KJ et al (2018) Long-term follow-up of CD19 CAR therapy in acute lymphoblastic leukemia. N Engl J Med 378(5):449–459
Jabbour EJ, Sasaki K, Ravandi F, Short NJ, Garcia-Manero G, Daver N et al (2019) Inotuzumab ozogamicin in combination with low-intensity chemotherapy (mini-HCVD) with or without blinatumomab versus standard intensive chemotherapy (HCVAD) as frontline therapy for older patients with Philadelphia chromosome-negative acute lymphoblastic leukemia: a propensity score analysis. Cancer 125(15):2579–2586
Pullarkat VA, Lacayo NJ, Jabbour E, Rubnitz JE, Bajel A, Laetsch TW et al (2021) Venetoclax and navitoclax in combination with chemotherapy in patients with relapsed or refractory acute lymphoblastic leukemia and lymphoblastic lymphoma. Cancer Discov 11(6):1440–1453
Dai H-p, Kong D-q, Shen H-j, Cui W, Wang Q, Li Z et al (2023) CAR-T cell therapy followed by allogenic hematopoietic stem cell transplantation yielded comparable outcome between Ph like ALL and other high-risk ALL. Biomark Res 11(1):19
Herold T, Baldus CD, Gökbuget N (2014) Ph-like acute lymphoblastic leukemia in older adults. N Engl J Med 371(23):2235
Miller KC, Al-Kali A, Shah MV, Hogan WJ, Elliott MA, Begna KH et al (2019) Elderly acute lymphoblastic leukemia: a Mayo Clinic study of 124 patients. Leuk Lymphoma 60(4):990–999
Kantarjian H, Ravandi F, Short NJ, Huang X, Jain N, Sasaki K et al (2018) Inotuzumab ozogamicin in combination with low-intensity chemotherapy for older patients with Philadelphia chromosome-negative acute lymphoblastic leukaemia: a single-arm, phase 2 study. Lancet Oncol 19(2):240–248
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors equally contributed to this research by collecting the available data, analysis, writing, and revision the final article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alghandour, R., Sakr, D.H. & Shaaban, Y. Philadelphia-like acute lymphoblastic leukemia: the journey from molecular background to the role of bone marrow transplant—review article. Ann Hematol 102, 1287–1300 (2023). https://doi.org/10.1007/s00277-023-05241-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05241-2