Abstract
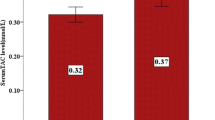
Oxidative stress is a major contributor to the pathophysiology of sickle cell disease (SCD) including hemolysis and vaso-occlusive crisis (VOC). L-glutamine is a conditionally essential amino acid with important roles, including the synthesis of antioxidants, such as reduced glutathione and the cofactors NAD(H) and NADP(H), as well as nitric oxide. Given the increased levels of oxidative stress and lower (NADH):(NAD + + NADH) ratio in sickle erythrocytes that adversely affects the blood rheology compared to normal red blood cells, L-glutamine was investigated for its therapeutic potential to reduce VOC. While L-glutamine was approved by the United States (US) Food and Drug Administration to treat SCD, its impact on the redox environment in sickle erythrocytes is not fully understood. The mechanism through which L-glutamine reduces VOC in SCD is also not clear. In this paper, we will summarize the results of the Phase 3 study that led to the approval of L-glutamine for treating SCD and discuss its assumed mechanisms of action. We will examine the role of L-glutamine in health and propose how the extra-erythrocytic functions of L-glutamine might contribute to its beneficial effects in SCD. Further research into the role of L-glutamine on extra-erythrocyte functions might help the development of an improved formulation with more efficacy.



Similar content being viewed by others
References
Sundd P, Gladwin MT, Novelli EM (2019) Pathophysiology of sickle cell disease. Annu Rev Pathol 14:263–292. https://doi.org/10.1146/annurev-pathmechdis-012418-012838
Jang T, Poplawska M, Cimpeanu E, Mo G, Dutta D, Lim SH (2012) Vaso-occlusive crisis in sickle cell disease: a vicious cycle of secondary events. J Transl Med 19:397. https://doi.org/10.1186/s12967-021-03074-z
Jang T, Mo G, Stewart C, Khoury L, Ferguson N, Egini O, Muthu J, Dutta D, Salifu M, Lim SH (2021) Hematopoietic stem cell transplant for sickle cell disease: patient selection and timing based on sickle cell-related multiple chronic conditions. Cell Transplant 30:09636897211046559. https://doi.org/10.1177/09636897211046559
Lanzkron S, Carroll CP, Haywood C Jr (2013) Mortality rates and age at death from sickle cell disease: U.S., 1979–2005. Public Health Rep 128:110–116. https://doi.org/10.1177/003335491312800206
Arias E, Rostron BL, Tejada-Vera B (2010) United States life tables, 2005. Natl Vital Stat Rep 58:1–132
Charache S, Barton FB, Moore RD, Terrin ML, Steinberg MH, Dover GJ, Ballas SK, McMahon RP, Castro O, Orringer EP (1996) Hydroxyurea and sickle cell anemia. Clinical utility of a myelosuppressive “switching” agent. The Multicenter Study of Hydroxyurea in Sickle Cell Anemia. Medicine (Baltimore) 75:300–326. https://doi.org/10.1097/00005792-199611000-00002
Buckner TW, Ataga KI (2014) Does hydroxyurea prevent pulmonary complications of sickle cell disease? Hematol Am Soc Hematol Educ Program 2014:432–437
Centers for Disease Control and Prevention (CDC). Sickle cell data collection data brief: hydroxyurea use among Medicaid beneficiaries with sickle cell disease in California and Georgia, 2006–2016. <https://www.cdc.gov/ncbddd/hemoglobinopathies/scdc-hydruxyurea-data-brief.html>. Accessed 24 December 2021.
Niihara Y, Miller ST, Kanter J, Lanzkron S, Smith WR, Hsu LL, Gordeuk VR, Viswanathan K, Sarnaik S, Osunkwo I, Guillaume E (2018) A phase 3 trial of L-glutamine in sickle cell disease. N Engl J Med 379:226–235. https://doi.org/10.1056/NEJMoa1715971
Quinn CT (2018) L-Glutamine for sickle cell anemia: more questions than answers. Blood 132:689–693. https://doi.org/10.1182/blood-2018-03-834440
Morris CR, Suh JH, Hagar W, Larkin S, Bland DA, Steinberg MH, Vichinsky EP, Shigenaga M, Ames B, Kuypers FA, Klings ES (2008) Erythrocyte glutamine depletion, altered redox environment, and pulmonary hypertension in sickle cell disease. Blood 111:402–410. https://doi.org/10.1182/blood-2007-04-081703
Zerez CR, Lachant NA, Lee SJ, Tanaka KR (1988) Decreased erythrocyte nicotinamide adenine dinucleotide redox potential and abnormal pyridine nucleotide content in sickle cell disease. Blood 71:512–515. https://doi.org/10.1182/blood.V71.2.512.512
Al-Ali AK (2002) Pyridine nucleotide redox potential in erythrocytes of Saudi subjects with sickle cell disease. Acta Haematol 108:19–22. https://doi.org/10.1159/000063062
Alayash AI (2018) Oxidative pathways in the sickle cell and beyond. Blood Cells Mol Dis 70:78–86. https://doi.org/10.1016/j.bcmd.2017.05.009
Niihara Y, Matsui NM, Shen YM, Akiyama DA, Johnson CS, Sunga MA, Magpayo J, Embury SH, Kalra VK, Cho SH, Tanaka KR (2005) L-glutamine therapy reduces endothelial adhesion of sickle red blood cells to human umbilical vein endothelial cells. BMC Blood Dis 5:4. https://doi.org/10.1186/1471-2326-5-4
Cruzat V, Rogero MM, Keane KN, Curi R, Newsholme P (2018) Glutamine: metabolism and immune function, supplementation and clinical translation. Nutrients 10:1564. https://doi.org/10.3390/nu10111564
Curi R, Newsholme P, Marzuca-Nassr GN, Takahashi HK, Hirabara SM, Cruzat V, Krause M, de Bittencourt Jr PI (2016) Regulatory principles in metabolism-then and now. Biochem J 473:1845–1857. https://doi.org/10.1042/BCJ20160103
Souba WW (1991) Glutamine: a key substrate for the splanchnic bed. Annu Rev Nutr 11:285–308. https://doi.org/10.1146/annurev.nu.11.070191.001441
Wessner B, Strasser EM, Spittler A, Roth E (2003) Effect of single and combined supply of glutamine, glycine, N-acetylcysteine, and R, S-alpha-lipoic acid on glutathione content of myelomonocytic cells. Clin Nutr 22:515–522. https://doi.org/10.1016/S0261-5614(03)00053-0
Huang Y, Shao XM, Neu J (2003) Immunonutrients and neonates. Eur J Pediatr 162:122–128. https://doi.org/10.1007/s00431-002-1128-0
Cruzat VF, Krause M, Newsholme P (2014) Amino acid supplementation and impact on immune function in the context of exercise. J Int Soc Sports Nutr 11:61. https://doi.org/10.1186/s12970-014-0061-8
Coëffier M, Miralles-Barrachina O, Le Pessot F, Lalaude O, Daveau M, Lavoinne A, Lerebours E, Déchelotte P (2001) Influence of glutamine on cytokine production by human gut in vitro. Cytokine 13:148–154. https://doi.org/10.1006/cyto.2000.0813
Ko TC, Beauchamp RD, Townsend CM Jr, Thompson JC (1993) Glutamine is essential for epidermal growth factor-stimulated intestinal cell proliferation. Surgery 114:147–153
Rhoads JM, Argenzio RA, Chen WU, Rippe RA, Westwick JK, Cox AD, Berschneider HM, Brenner DA (1997) L-glutamine stimulates intestinal cell proliferation and activates mitogen-activated protein kinases. Am J Physiol 272:G943–G953. https://doi.org/10.1152/ajpgi.1997.272.5.G943
Ziegler TR, Mantell MP, Chow JC, Rombeau JL, Smith RJ (1996) Gut adaptation and the insulin-like growth factor system: regulation by glutamine and IGF-I administration. Am J Physiol 271:G866–G875. https://doi.org/10.1152/ajpgi.1996.271.5.G866
Blikslager AT, Rhoads JM, Bristol DG, Roberts MC, Argenzio RA (1999) Glutamine and transforming growth factor-a stimulate extracellular regulated kinases and enhance recovery of villous surface area in porcine ischemic-injured intestine. Surgery 125:186–194. https://doi.org/10.1016/S0039-6060(99)70264-3
Lacey JM, Wilmore DW (1990) Is glutamine a conditionally essential amino acid? Nutr Rev 48:297–309. https://doi.org/10.1111/j.1753-4887.1990.tb02967.x
Rhoads JM, Wu G (2009) Glutamine, arginine, and leucine signaling in the intestine. Amino Acids 37:111–122. https://doi.org/10.1007/s00726-008-0225-4
Circu ML, Aw TY (2012) Glutathione and modulation of cell apoptosis. Biochim Biophys Acta 1823:1767–1777. https://doi.org/10.1016/j.bbamcr.2012.06.019
Schafer FQ, Buettner GR (2001) Redox environment of the cell as viewed through the redox state of the glutathione disulfide/glutathione couple. Free Radic Biol Med 30:1191–1212. https://doi.org/10.1016/S0891-5849(01)00480-4
Griffith OW (1999) Biologic and pharmacologic regulation of mammalian glutathione synthesis. Free Radic Biol Med 27:922–935. https://doi.org/10.1016/S0891-5849(99)00176-8
Nur E, Verwijs M, de Waart DR, Schnog JJ, Otten HM, Brandjes DP, Biemond BJ, Elferink RP, CURAMA Study Group (2011) Increased efflux of oxidized glutathione (GSSG) causes glutathione depletion and potentially diminishes antioxidant defense in sickle erythrocytes. Biochim Biophys Acta 1812:1412–1417. https://doi.org/10.1016/j.bbadis.2011.04.011
Hall A (1999) The role of glutathione in the regulation of apoptosis. Eur J Clin Invest 29:238–245. https://doi.org/10.1046/j.1365-2362.1999.00447.x
Hou YC, Chu CC, Ko TL, Yeh CL, Yeh SL (2013) Effects of alanyl-glutamine dipeptide on the expression of colon-inflammatory mediators during the recovery phase of colitis induced by dextran sulfate sodium. Eur J Nutr 52:1089–1098. https://doi.org/10.1007/s00394-012-0416-3
Xue H, Sufit AJ, Wischmeyer PE (2011) Glutamine therapy improves outcome of in vitro and in vivo experimental colitis models. JPEN J Parenter Enteral Nutr 35:188–197. https://doi.org/10.1177/0148607110381407
Haynes TE, Li P, Li X, Shimotori K, Sato H, Flynn NE, Wang J, Knabe DA, Wu G (2009) L-Glutamine or L-alanyl-L-glutamine prevents oxidant- or endotoxin-induced death of neonatal enterocytes. Amino Acids 37:131–142. https://doi.org/10.1007/s00726-009-0243-x
Karin M (2009) NF-kB as a critical link between inflammation and cancer. Cold Spring Harb Perspect Biol 1:a000141. https://doi.org/10.1101/cshperspect.a000141
Ganeshan K, Chawla A (2014) Metabolic regulation of immune responses. Annu Rev Immunol 32:609–634. https://doi.org/10.1146/annurev-immunol-032713-120236
Malhotra V, Eaves-Pyles T, Odoms K, Quaid G, Shanley TP, Wong HR (2002) Heat shock inhibits activation of NF-κB in the absence of heat shock factor-1. Biochem Biophys Res Commun 291:453–457. https://doi.org/10.1006/bbrc.2002.6470
Dutta D, Methé B, Amar S, Morris A, Lim SH (2019) Intestinal injury and gut permeability in sickle cell disease. J Transl Med 17:183. https://doi.org/10.1186/s12967-019-1938-8
Poplawska M, Dutta D, Jayaram M, Salifu M, Chong NS, Lim SH (2021) Intestinal pathophysiological abnormalities in steady state and after vaso-occlusive crisis in murine sickle cell disease. Br J Haematol 196:777–780. https://doi.org/10.1111/bjh.17889
Lim SH, Methé BA, Knoll BM, Morris A, Obaro SK (2018) Invasive non-typhoidal Salmonella in sickle cell disease in Africa: is increased gut permeability the missing link? J Transl Med 16:239. https://doi.org/10.1186/s12967-018-1622-4
Anderson JM, Van Itallie CM (1995) Tight junctions and the molecular basis for regulation of paracellular permeability. Am J Physiol 269:G467–G475. https://doi.org/10.1152/ajpgi.1995.269.4.G467
Van Itallie CM, Anderson JM (2006) Claudins and epithelial paracellular transport. Annu Rev Physiol 68:403–429. https://doi.org/10.1146/annurev.physiol.68.040104.131404
Gonzalez-Mariscal L, Betanzos A, Nava P, Jaramillo B (2003) Tight junction proteins. Prog Biophys Mol Biol 81:1–44. https://doi.org/10.1016/S0079-6107(02)00037-8
Zihni C, Mills C, Matter K, Balda MS (2016) Tight junctions: from simple barriers to multifunctional molecular gates. Nat Rev Mol Cell Biol 17:564–580. https://doi.org/10.1038/nrm.2016.80
Mitic LL, Anderson JM (1998) Molecular architecture of tight junctions. Annu Rev Physiol 60:121–142. https://doi.org/10.1146/annurev.physiol.60.1.121
Cunningham KE, Turner JR (2012) Myosin light chain kinase: pulling the strings of epithelial tight junction function. Ann N Y Acad Sci 1258:34–42. https://doi.org/10.1111/j.1749-6632.2012.06526.x
Rao R (2008) Oxidative stress-induced disruption of epithelial and endothelial tight junctions. Front Biosci 13:7210–7226. https://doi.org/10.2741/3223
Gonzalez-Mariscal L, Tapia R, Chamorro D (2008) Crosstalk of tight junction components with signaling pathways. Biochim Biophys Acta 1778:729–756. https://doi.org/10.1016/j.bbamem.2007.08.018
Li N, Neu J (2009) Glutamine deprivation alters intestinal tight junctions via a PI3-K/Akt mediated pathway in Caco-2 cells. J Nutr 139:710–714. https://doi.org/10.3945/jn.108.101485
Wang B, Wu Z, Ji Y, Sun K, Dai Z, Wu G (2016) L-glutamine enhances tight junction integrity by activating CaMK kinase 2–AMP-activated protein kinase signaling in intestinal porcine epithelial cells. J Nutr 146:501–508. https://doi.org/10.3945/jn.115.224857
Chanez-Paredes SD, Abtahi S, Kuo W-T, Turner JR (2021) Differentiating between tight junction-dependent and tight junction-independent intestinal barrier loss in vivo. In: Turksen K. (eds) Permeability Barrier. Methods in Molecular Biology, vol 2367. Humana, New York. https://doi.org/10.1007/7651_2021_389
Lee SH (2015) Intestinal permeability regulation by tight junction: Implication on inflammatory bowel diseases. Intest Res 13:11–18. https://doi.org/10.5217/ir.2015.13.1.11
Liu R, Hong J, Xu X et al (2017) Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Nat Med 23:859–868. https://doi.org/10.1038/nm.4358
Jegatheesan P, Beutheu S, Ventura G, Sarfati G, Nubret E, Kapel N, Waligora-Dupriet AJ, Bergheim I, Cynober L, De-Bandt JP (2016) Effect of specific amino acids on hepatic lipid metabolism in fructose-induced non-alcoholic fatty liver disease. Clin Nutr 35:175–182. https://doi.org/10.1016/j.clnu.2015.01.021
Chamorro S, de Blas C, Grant G, Badiola I, Menoyo D, Carabaño R (2010) Effect of dietary supplementation with glutamine and a combination of glutamine-arginine on intestinal health in twenty-five-day-old weaned rabbits. J Anim Sci 88:170–180. https://doi.org/10.2527/jas.2008-1698
Zhang Y, Lu T, Han L, Zhao L, Niu Y, Chen H (2017) L-glutamine supplementation alleviates constipation during late gestation of mini sows by modifying the microbiota composition in feces. BioMed Res Int 2017:4862861. https://doi.org/10.1155/2017/4862861
Lim SH, Morris A, Li K, Fitch AC, Fast L, Goldberg L, Quesenberry M, Sprinz P, Methé B (2018) Intestinal microbiome analysis revealed dysbiosis in sickle cell disease. Am J Hematol 93:E91–E93. https://doi.org/10.1002/ajh.25019
Brim H, Taylor J, Abbas M, Vilmenay K, Daremipouran M, Varma S, Lee E, Pace B, Song-Naba WL, Gupta K, Nekhai S, O’Neil P, Ashktorab H (2021) The gut microbiome in sickle cell disease: characterization and potential implications. PLoS ONE 16:e0255956. https://doi.org/10.1371/journal.pone.0255956
Kretzmann NA, Fillmann H, Mauriz JL, Marroni CA, Marroni N, González-Gallego J, Tuñón MJ (2008) Effects of glutamine on proinflammatory gene expression and activation of nuclear factor kappa B and signal transducers and activators of transcription in TNBS-induced colitis. Inflamm Bowel Dis 14:1504–1513. https://doi.org/10.1002/ibd.20543
Liboni KC, Li N, Scumpia PO, Neu J (2005) Glutamine modulates LPS-induced IL-8 production through IκB/NF-κB in human fetal and adult intestinal epithelium. J Nutr 135:245–251. https://doi.org/10.1093/jn/135.2.245
Liboni K, Li N, Neu J (2004) Mechanism of glutamine-mediated amelioration of lipopolysaccharide-induced IL-8 production in Caco-2 cells. Cytokine 26:57–65. https://doi.org/10.1016/j.cyto.2003.12.008
Anyaegbu CC, Okpala IE, Akren’Ova YA, Salimonu LS (1998) Peripheral blood neutrophil count and candidacidal activity correlate with the clinical severity of sickle cell anaemia (SCA). Eur J Haematol 60:267–268. https://doi.org/10.1111/j.1600-0609.1998.tb01036.x
Lard LR, Mul FP, de Haas M, Roos D, Duits AJ (1999) Neutrophil activation in sickle cell disease. J Leukoc Biol 66:411–415. https://doi.org/10.1002/jlb.66.3.411
Lum AF, Wun T, Staunton D, Simon SI (2004) Inflammatory potential of neutrophils detected in sickle cell disease. Am J Hematol 76:126–133. https://doi.org/10.1002/ajh.20059
Turhan A, Weiss LA, Mohandas N, Coller BS, Frenette PS (2002) Primary role for adherent leukocytes in sickle cell vascular occlusion: a new paradigm. Proc Natl Acad Sci USA 99:3047–3051. https://doi.org/10.1073/pnas.052522799
Zhang D, Chen G, Manwani D, Mortha A, Xu C, Faith JJ, Burk RD, Kunisaki Y, Jang JE, Scheiermann C, Merad M, Frenette PS (2015) Neutrophil ageing is regulated by the microbiome. Nature 525:528–532. https://doi.org/10.1038/nature15367
Lim SH, Dutta D, Moore J (2019) Rifaximin for sickle cell disease. Am J Hematol 94:E325–E328. https://doi.org/10.1002/ajh.25637
Dutta D, Li K, Methé B, Lim SH (2020) Rifaximin on intestinally-related pathologic changes in sickle cell disease. Am J Hematol 95:E83–E86. https://doi.org/10.1002/ajh.25722
Bradt P, Spackman E, Synnott PG, Chapman R, Beinfeld M, Rind DM, and Pearson SD. Crizanlizumab, voxelotor, and L-glutamine for sickle cell disease: effectiveness and value. Institute for Clinical and Economic Review. 2020. https://icer.org/wp-content/uploads/2020/10/ICER_SCD_Evidence-Report_031220-FOR-PUBLICATION.pdf.
Steinberg MH (2020) Treating sickle cell anemia: a new era dawns. Am J Hematol 95:338–342. https://doi.org/10.1002/ajh.25724
Emmaus Life Sciences Reports Increase in Sales Volume in 2020. <https://www.prnewswire.com/news-releases/emmaus-life-sciences-reports-increase-in-sales-volume-in-2020-301216439.html>. Accessed 2 December 2021.
Ogu UO, Thomas M, Chan F, Vattappally L, Sebastian G, Crouch A, You S, Minniti CP (2021) L-glutamine use in adults with sickle cell disease: clinical trials where success meets reality. Am J Hematol 96:E38–E40. https://doi.org/10.1002/ajh.26021
Emmaus withdraws European application for sickle cell drug that got US approval. <https://medcitynews.com/2019/09/emmaus-withdraws-european-application-for-sickle-cell-drug-that-got-us-approval//>. Accessed 2 December 2021.
Xyndari: Withdrawal of the marketing authorization application (2019) https://www.ema.europa.eu/en/documents/withdrawal-report/withdrawal-assessment-report-xyndari_en.pdf. Access 6 April 2022.
Acknowledgements
Figures created with BioRender.com.
Author information
Authors and Affiliations
Contributions
FJ, GS, TJ, EC, and MP performed the literature search and wrote the first drafts of the manuscript. DD supervised the work and helped write the final draft. DD also designed the figures. SHL conceived the idea, provided supervision, and wrote the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Study highlights
Oxidative stress in sickle erythrocytes due to polymerization and auto-oxidation of HbS causes hemolysis and contributes to sickle cell pathophysiology. L-glutamine ameliorates the oxidative stress in sickle erythrocytes and reduces VOC. However, L-glutamine therapy did not change either the Hb or the reticulocyte counts significantly when compared to the placebo group. Thus, the exact mechanisms of L-glutamine in reducing the frequency of painful VOC is unknown and this is limiting the further development to improve the formulation for better efficacy of the agent. In this paper, we discussed the extra-erythrocytic functions of L-glutamine in SCD. It is known that SCD has intestinal dysbiosis and has defective intestinal barrier. Since L-glutamine has a major role in intestinal health, we discussed how L-glutamine might improve tight junction functions, gut microbiome, immunity, and inflammatory conditions in SCD to provide the benefits against VOC. Understanding of how L-glutamine works in reducing VOC, therefore, would help in its further development to improve clinical efficacy in SCD.
Firas Jafri, Gyuhee Seong, and Tim Jang are equal first authors.
Rights and permissions
About this article
Cite this article
Jafri, F., Seong, G., Jang, T. et al. L-glutamine for sickle cell disease: more than reducing redox. Ann Hematol 101, 1645–1654 (2022). https://doi.org/10.1007/s00277-022-04867-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-04867-y