Abstract
Patients with myeloproliferative neoplasms (MPNs) experience burdensome symptoms that negatively affect their quality of life. How MPN symptoms relate with medical disability leave (MDL) among patients with the disease has not been previously examined. Using data collected from the Living with MPNs patient survey, symptom burden and functional status were compared in patients who reported taking MDL due to their MPN versus patients who reported no changes in employment status. Among 592 patients who were employed full- or part-time at diagnosis, 24.8% reported taking ≥ 1 MDL and 49.4% reported no change in employment status as a result of their MPN. Of the patients who took MDL, 29.9% took ≥ 2 MDLs, and most patients (62.6%) did not return to work. All 10 symptoms comprising the MPN Symptom Assessment Form were significantly more frequent and severe in patients who took MDL compared with those who had no employment change. Furthermore, functional impairments were also significantly more frequent among patients who went on MDL versus those with no employment change. Effective management of MPN-related symptoms may reduce disability leave among patients with high symptom burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with chronic Philadelphia chromosome-negative myeloproliferative neoplasms (MPNs), including myelofibrosis (MF), polycythemia vera (PV), and essential thrombocythemia (ET), have reduced survival compared with the general population [1, 2] and may experience substantial symptom burden during the course of their disease [3, 4]. Commonly reported symptoms include fatigue (45–99%), early satiety (21–77%), inactivity (19–77%), night sweats (25–63%), bone pain (23–55%), and problems with concentration (19–73%) [3,4,5,6]. These common symptoms may be severe based on MPN Symptom Assessment Form (MPN-SAF) scores (fatigue, 2.9–6.7; early satiety, 1.0–3.2; inactivity, 1.0–6.7; night sweats, 1.9–2.6; bone pain, 1.2–2.2; and problems with concentration, 1.5–6.1) [3,4,5,6]. In the MPN Landmark survey of patients with MF, PV, or ET, many patients reported a decrease in quality of life (MF, 81%; PV, 66%; ET, 57%), and interference with activities of daily living (MF, 53%; PV, 48%; ET, 37%) as a result of their disease [4]. Additionally, several studies have reported that a significant proportion of patients with MPNs require support of a caregiver (40–55%) and many employed patients experience an overall work impairment (31–36%) [6,7,8].
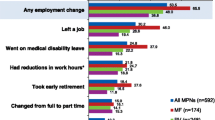
The effects of MPN symptom burden on patients’ ability to work or employment status were reported in two studies to date. Among employed respondents of the MPN Landmark survey, many reported reduced work hours because of their MPN (MF, 59%; PV, 37%; ET, 30%) [4], suggesting that symptom burden may have a significant impact on employment status. In a previous analysis of the Living with MPNs survey, approximately half (51%) of all employed respondents reported at least one change in employment status (e.g., left job, took early retirement, took disability leave, reduced work hours) as a result of their MPN [7]. Furthermore, more severe symptom burden as assessed by the MPN-SAF total symptom score (TSS) was highly correlated with reduced work productivity as measured with the Work Productivity and Activity Impairment Specific Health Problem questionnaire (correlation coefficients: absenteeism, 0.37; presenteeism, 0.70; work impairment, 0.70; activity impairment, 0.70 [all P < 0.001]) [7]. In this analysis, the characteristics of medical disability leave (MDL) among patients with MPNs and the relationship between MDL and MPN symptom burden were examined using data from the Living with MPNs survey.
Patients and methods
Study design and participants
The Living with MPNs survey was a cross-sectional online questionnaire conducted between April and November 2016. The study received approval from the Quorum Review Institutional Review Board. Respondents were recruited through emails; online posts on MPN-focused social media and patient advocacy websites; banner advertisements on medical websites, Google, and Facebook; and postcards distributed to the offices of hematologists and oncologists. Survey participants were offered $25 in compensation for completing the survey and provided informed consent electronically before responding to the survey. Respondents were 18 to 70 years of age with a diagnosis of MF, PV, or ET in the USA [7]. The survey was designed to be completed in approximately 30 min and included approximately 100 questions related to patient demographics; MPN diagnosis and disease-related medical history; changes in employment status, work productivity, and daily activities; MPN-related symptoms; functional status; and quality-of-life measures [7]. For those patients who reported being employed full-time or part-time at the time of diagnosis with MF, PV, or ET, a series of questions was asked about various types of employment changes (e.g., left job, took early retirement, took MDL, had reduced work hours, and changed from full-time to part-time job) due to MPN disease and the specifics of those changes. Based on these questions, patients who took MDL after diagnosis because of their MPN disease were identified. For those who indicated that they took any MDL because of their MPN disease, the number of MDLs, most recent MDL start and end year, type (i.e., long-term or short-term), receipt of social security benefits, and whether patients returned to work following the most recent MDL were reported.
The MPN-SAF was used to assess the severity of the 10 most clinically relevant and characteristic MPN symptoms (abdominal discomfort, bone pain, early satiety, fatigue, fever, inactivity, itching, night sweats, problems with concentration, and unintentional weight loss) on a scale from 0 (absent) to 10 (worst) [3]. Symptoms were further categorized by severity based on MPN-SAF score (none, 0; mild, 1–3; moderate, 4–6; severe, ≥ 7). The MPN-SAF TSS, the sum of the 10 individual symptom scores, was also calculated, with maximum TSS of 100 [3]. Additionally, 15 questions on functional status in physical, mental, and social domains were assessed with a five-scale response (“not at all,” “a little bit,” “somewhat,” “quite a bit,” or “a great deal”).
Statistical analyses
Symptoms were compared between patients who reported taking MDL because of their MPN and patients who reported no employment change using a regression model adjusting for the type of MPN. The association between functional status and having taken MDL versus having no employment change due to MPN was assessed using a Cochran-Mantel-Haenszel test stratified by type of MPN. All other data, including patient demographics and disease characteristics, were summarized using descriptive statistics as appropriate.
Results
Patient demographics and disease characteristics
Out of 904 patients who participated in the Living with MPNs survey, 592 were employed at the time of MPN diagnosis. Among employed patients, 147 (24.8%) reported going on ≥ 1 MDL because of their MPN (MF, 37.9%; PV, 22.2%; ET, 15.3%) and 293 (49.5%) reported no employment changes resulting from their MPN. The remaining 152 employed patients (25.7%) reported other non-MDL changes in employment status (e.g., early retirement, work hour reduction) and were excluded from this analysis. Patients who took MDL had a mean (range) age of 52.3 (24–70) years. Most patients (84.4%) who took MDL were employed full-time at the time of MPN diagnosis. Patient demographics and MPN characteristics, including disease duration, were generally similar between patients who went on MDL because of their MPN and those who reported no changes in employment status, with the exception of history of thrombotic event (TE), in which patients who went on MDL were roughly twice as likely to have experienced ≥ 1 prior TE than those with no employment change (31.3% versus 15.4%, respectively; Table 1). Among patients with a history of TE, 46 patients (35.9%) reported taking MDL, whereas 101 patients (21.8%) without a history of TE took MDL.
Medical disability leave
Among the 147 patients who reported going on MDL because of their MPN, the mean duration from diagnosis to first leave was 2.3 years, with 44 patients (29.9%) taking ≥ 2 MDLs (Table 2). For nearly half of patients who went on MDL (48.3%), the most recent leave was long-term. Most patients who took MDL (62.6%) did not return to work; among patients who did return to work following MDL (37.4%), the mean duration of leave was 4.3 months. Among the three MPN diseases, patients with a diagnosis of MF had the highest rates of long-term leave for the most recent MDL (57.6%) and highest rates of not returning to work (77.3%). Nearly half of all patients who took MDL (46.3%) reported receiving social security while on MDL. Most patients (85.5%) who returned to work following MDL reported receiving a similar salary to that received before the leave; 10.9% reported a decrease in salary after returning to work.
Symptom burden
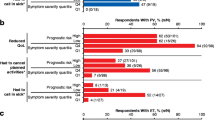
Patients who went on MDL because of their MPNs generally experienced higher frequency and a more severe degree of all 10 symptoms in the MPN-SAF compared with patients who reported no change in employment status (Fig. 1). Patients who took MDL had a mean MPN-SAF TSS more than double that of patients who had no employment change (42.9 versus 20.1, respectively; P < 0.001; Table 3). The mean MPN-SAF TSS in patients who took MDL was similar across MPN diagnoses. Among patients who took MDL, fatigue, inactivity, and bone pain were the most severe symptoms, with mean symptom scores of 7.1, 5.6, and 5.4, respectively, and were “severe” in 63.0%, 44.2%, and 43.7% of patients. In contrast, among patients who reported no employment change because of their MPN, the mean symptom scores for fatigue, inactivity, and bone pain were 4.4, 2.4, and 1.9, respectively, and these symptoms were severe in 30.4%, 10.6%, and 9.3% of patients. The mean MPN-SAF TSS as well as the scores for each of the 10 individual symptoms were significantly worse in patients who took MDL versus those who did not.
Functional impairment
All aspects of functional impairments assessed in this analysis were more common and more severe among patients who took MDL than those who reported no change in employment (Fig. 2). Prevalent functional impairments among patients who took MDL compared with those who reported no employment change included difficulty with strenuous physical activities (91.2% versus 64.8%; P < 0.001), difficulty remembering things (90.5% versus 60.8%; P < 0.001), difficulty doing work around the house (88.4% versus 51.2%; P < 0.001), difficulty sleeping (84.4% versus 58.7%; P < 0.001), feeling anxious or worried about the future (83.7% versus 67.9%; P = 0.002), and feeling depressed or sad (81.6% versus 52.6%; P < 0.001).
Discussion
In this analysis, approximately one in four patients who were employed at the time of MPN diagnosis went on MDL as a result of their MPN. Nearly half of these patients took long-term leave, with half receiving social security during leave. Most patients who went on MDL did not return to the workforce.
Patients with MPNs face a number of burdensome symptoms, which are associated with reductions in overall survival [9] and quality of life [3, 4, 6]. Physical and mental symptom burden can interfere with one’s ability to work across a wide spectrum of disorders and physiological states [10,11,12]. Studies of patients with various cancers demonstrate an inverse relationship between symptom burden and employment [13,14,15]. In the current study, the symptom burden of patients who reported no employment change was comparable to that of 1425 patients with MPNs in a prospective international survey (mean MPN-SAF TSS of 20.1 versus 21.2) [3]. However, symptoms were more frequent and severe in patients with MPNs who reported taking MDL (e.g., MPN-SAF TSS, 42.9) versus those with no change in employment status. Findings from a separate analysis of the effects of MPNs on work productivity in respondents of the Living with MPNs survey demonstrated a significant negative correlation between symptom burden and work productivity [7]. Studies in other symptomatic diseases, such as arthritis, psychiatric disorders, and gastrointestinal diseases, also show significantly higher numbers of sickness absences compared with the general population [16, 17]. These findings underscore the prominent role that symptoms play in affecting the functional ability for everyday life and work among patients with MPNs. As fatigue is consistently reported as having the highest symptom burden in patients with MPNs and was worse among patients taking MDL, fatigue symptom burden could be useful in identifying patients at risk of taking MDL and for implementing treatments and navigating management strategies.
Consistent with the increased symptom burden, patients who took MDL were more likely than those who did not to report functional impairment across physical, mental, and social domains, such as difficulty sleeping, feeling depressed, difficulty remembering, difficulty with self-care, and difficulty attending major social events. Functional impairments reported by patients with MPNs may interfere with work ability as well as activities of daily living. For instance, 55.1% of respondents in a separate analysis of the Living with MPNs survey reported receiving help from a caregiver, and among those who received assistance, 23.9% reported receiving caregiver help “often” [8]. The most common types of caregiver assistance provided to patients were homemaking (77.7%), companionship (57.4%), and transportation (55.2%). Symptom burden and functional impairments experienced by patients with MPNs can also have a negative impact on social domains. Results of the MPN Landmark survey demonstrated that many patients with MPNs reported interference with family or social life and canceling planned activities due to their disease [4]. In the current study, patients who took MDL were generally more likely to report limited ability to socialize, feeling isolated, difficulty in attending major social events, and problems with sex life versus those who did not take MDL.
In this study, 63% of patients who took MDL did not return to work, with the highest rates observed among patients with MF (77%). This rate may have been influenced by early retirement status, as patients with MF were generally older (mean age at diagnosis, 51 years) compared with patients with PV (42 years) or ET (39 years). Measures to improve patients’ ability to return to work—such as flexible work hours, temporary work-hour reductions, and options for remote access—may increase the rate of return to work following MDL among patients with MPNs. The rate of return to work in patients with MPNs in the current study (37%) was within the range reported in a literature review of patients with various cancers (mean across all studies, 62%; range, 30–93%) [14]. However, it is important to note that a variety of factors play a role in determining whether or not a patient with cancer is able to return to work, making it difficult to compare between studies and cancer settings. Longitudinal examination of other chronic illnesses reported substantial rates of “not working” status in patients diagnosed with several diseases, including heart disease (61%), arthritis (45%), diabetes (44%), back pain (37%), and hypertension (30%) [18]. High rates of MDL and the inability of many patients with chronic illnesses to return to the workforce may have significant societal implications. For instance, employers are faced with work interruption and lost productivity [6, 7], and patients and their families may experience financial hardship due to limitations in wages or salaries and reduced income while on MDL [7]. Analyses of claims data demonstrated that patients with select cancers faced increased indirect personal costs compared with controls resulting from absenteeism and short-term disability [19]. Additionally, a longitudinal study of income loss among cancer survivors demonstrated that labor market earnings were reduced by up to 40% and total family income reduced by 20% at 2 years following a cancer diagnosis, with more pronounced losses observed among men [20]. Finally, society as a whole is affected by the increased burden placed on social safety net programs such as social security.
Limitations to this study included those inherent to self-reported patient surveys. For example, these patient-reported findings were not validated with data from medical records or feedback from treating physicians. Limited data on clinical characteristics of the disease, including risk level and disease stage, were available for this analysis. Although not assessed in depth in this analysis, history of TE was more prevalent among patients who took MDL versus those with no employment change, and may have contributed to the need for MDL. Furthermore, selection bias regarding participation in the online survey as well as recall bias of the respondents may have impacted results of this study. Finally, financial hardship resulting from taking disability leave and not returning to work was not assessed in this analysis and should be addressed in future studies.
Conclusion
Approximately one in four employed patients took at least one MDL due to their MPN disease. Patients with a history of TE were over 50% more likely to have taken MDL compared to patients without a history of TE. Patients with MPNs who reported taking MDL because of their MPN had more frequent and severe MPN-related symptoms and greater functional impairments compared with patients who reported no employment change. Most patients who went on MDL did not return to the workforce. Future studies should explore whether effective prevention of TE and management of MPN-related symptoms influences the need for forced medical leave among patients with high symptom burden.
References
Price GL, Davis KL, Karve S, Pohl G, Walgren RA (2014) Survival patterns in United States (US) Medicare enrollees with non-CML myeloproliferative neoplasms (MPN). PLoS One 9(3):e90299
Hultcrantz M, Kristinsson SY, Andersson TM, Landgren O, Eloranta S, Derolf AR, Dickman PW, Bjorkholm M (2012) Patterns of survival among patients with myeloproliferative neoplasms diagnosed in Sweden from 1973 to 2008: a population-based study. J Clin Oncol 30(24):2995–3001. https://doi.org/10.1200/JCO.2012.42.1925
Emanuel RM, Dueck AC, Geyer HL, Kiladjian JJ, Slot S, Zweegman S, te Boekhorst PAW, Commandeur S, Schouten HC, Sackmann F, Kerguelen Fuentes A, Hernández-Maraver D, Pahl HL, Griesshammer M, Stegelmann F, Doehner K, Lehmann T, Bonatz K, Reiter A, Boyer F, Etienne G, Ianotto JC, Ranta D, Roy L, Cahn JY, Harrison CN, Radia D, Muxi P, Maldonado N, Besses C, Cervantes F, Johansson PL, Barbui T, Barosi G, Vannucchi AM, Passamonti F, Andreasson B, Ferarri ML, Rambaldi A, Samuelsson J, Birgegard G, Tefferi A, Mesa RA (2012) Myeloproliferative neoplasm (MPN) symptom assessment form Total symptom score: prospective international assessment of an abbreviated symptom burden scoring system among patients with MPNs. J Clin Oncol 30(33):4098–4103. https://doi.org/10.1200/JCO.2012.42.3863
Mesa R, Miller CB, Thyne M, Mangan J, Goldberger S, Fazal S, Ma X, Wilson W, Paranagama DC, Dubinski DG, Boyle J, Mascarenhas JO (2016) Myeloproliferative neoplasms (MPNs) have a significant impact on patients’ overall health and productivity: the MPN landmark survey. BMC Cancer 16:167. https://doi.org/10.1186/s12885-016-2208-2
Scherber R, Dueck AC, Johansson P, Barbui T, Barosi G, Vannucchi AM, Passamonti F, Andreasson B, Ferarri ML, Rambaldi A, Samuelsson J, Birgegard G, Tefferi A, Harrison CN, Radia D, Mesa RA (2011) The myeloproliferative neoplasm symptom assessment form (MPN-SAF): international prospective validation and reliability trial in 402 patients. Blood 118(2):401–408. https://doi.org/10.1182/blood-2011-01-328955
Harrison CN, Koschmieder S, Foltz L, Guglielmelli P, Flindt T, Koehler M, Mathias J, Komatsu N, Boothroyd RN, Spierer A, Perez Ronco J, Taylor-Stokes G, Waller J, Mesa RA (2017) The impact of myeloproliferative neoplasms (MPNs) on patient quality of life and productivity: results from the international MPN landmark survey. Ann Hematol 96(10):1653–1665
Yu J, Parasuraman S, Paranagama D, Bai A, Naim A, Dubinski D, Mesa R (2018) Impact of myeloproliferative neoplasms on patients' employment status and work productivity in the United States: results from the Living with MPNs survey. BMC Cancer 18(1):420. https://doi.org/10.1186/s12885-018-4322-9
Paranagama D, Parasuraman S, Bai A, Yu J, Mesa R. Impact on caregivers of patients with myeloproliferative neoplasms (MPNs) in the United States: results from the Living With MPNs survey. Presented at: Eighth Annual Academy of Oncology Nurse & Patient Navigators Conference, November 16–19, 2017; Orlando, FL
Cervantes F, Dupriez B, Pereira A, Passamonti F, Reilly JT, Morra E, Vannucchi AM, Mesa RA, Demory JL, Barosi G, Rumi E, Tefferi A (2009) New prognostic scoring system for primary myelofibrosis based on a study of the international working Group for Myelofibrosis Research and Treatment. Blood 113(13):2895–2901. https://doi.org/10.1182/blood-2008-07-170449
Hengstebeck E, Roskos S, Breejen K, Arnetz B, Arnetz J (2017) Chronic pain disrupts ability to work by interfering with social function: a cross-sectional study. Scand J Pain 17:397–402
Katon W (2009) The impact of depression on workplace functioning and disability costs. Am J Manag Care 15(11 suppl):S322–S327
Woods NF, Mitchell ES (2011) Symptom interference with work and relationships during the menopausal transition and early postmenopause: observations from the Seattle midlife Women's health study. Menopause 18(6):654–661
Tevaarwerk AJ, Lee JW, Terhaar A, Sesto ME, Smith ML, Cleeland CS, Fisch MJ (2016) Working after a metastatic cancer diagnosis: factors affecting employment in the metastatic setting from ECOG-ACRIN's symptom outcomes and practice patterns study. Cancer 122(3):438–446
Spelten ER, Sprangers MA, Verbeek JH (2002) Factors reported to influence the return to work of cancer survivors: a literature review. Psychooncology 11(2):124–131
Wolvers MDJ, Leensen MCJ, Groeneveld IF, Frings-Dresen MHW, De Boer A (2018) Predictors for earlier return to work of cancer patients. J Cancer Surviv 12(2):169–177
Zirkzee EJM, Sneep AC, de Buck PD, Allaart CF, Peeters AJ, Ronday HK, Westedt ML, le Cessie S, Vliet Vlieland TP (2008) Sick leave and work disability in patients with early arthritis. Clin Rheumatol 27(1):11–19
Casimirri E, Vaccari A, Schito M, Bonci M, Stendardo M, Stefanati A, Nardini M, Boschetto P (2014) Chronic diseases are strongly associated with sickness absences in a sample of Italian public employees. Int J Occup Med Environ Health 27(3):343–354
Jetha A, Chen C, Mustard C, Ibrahim S, Bielecky A, Beaton D, Smith P (2017) Longitudinal examination of temporality in the association between chronic disease diagnosis and changes in work status and hours worked. Occup Environ Med 74(3):184–191
Chang S, Long SR, Kutikova L, Bowman L, Finley D, Crown WH, Bennett CL (2004) Estimating the cost of cancer: results on the basis of claims data analyses for cancer patients diagnosed with seven types of cancer during 1999 to 2000. J Clin Oncol 22(17):3524–3530
Zajacova A, Dowd JB, Schoeni RF, Wallace RB (2015) Employment and income losses among cancer survivors: estimates from a national longitudinal survey of American families. Cancer 121(24):4425–4432
Acknowledgments
Medical writing assistance was provided by Jane Kovalevich, PhD (Complete Healthcare Communications, LLC, North Wales, PA, a CHC Group company) and was funded by Incyte Corporation.
Funding
This work was funded by Incyte Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JY, DP, and SP are employees and shareholders of Incyte Corporation. RM received research funding from Celgene, CTI, Gilead, Incyte Corporation, and Promedior and served as a consultant for Ariad, Galena, and Novartis. HLG has no conflicts to disclose.
Ethical approval
The study was approved by the Quorum Review Institutional Review Board and all procedures were conducted in accordance with the 1964 Declaration of Helsinki and all of its subsequent revisions. Informed consent was obtained from all patients prior to survey completion.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclosure of previous presentation
This work was previously presented, in part, at the 59th American Society of Hematology Annual Meeting & Exposition, December 9–12, 2017, Atlanta, GA.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Yu, J., Paranagama, D., Geyer, H.L. et al. Relationship between symptom burden and disability leave among patients with myeloproliferative neoplasms (MPNs): findings from the Living with MPN patient survey. Ann Hematol 98, 1119–1125 (2019). https://doi.org/10.1007/s00277-019-03610-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03610-4