Abstract
Background
The placement of posterior mesh during pelvic organ prolapse laparoscopic surgery has been incriminated as responsible for postoperative adverse outcomes such as digestive symptoms, chronic pelvic pain, and sexual dysfunction. These complications may be related to neural injuries that occur during the fixation of the posterior mesh on the levator ani muscle.
Objectives
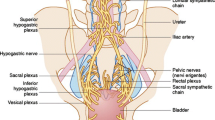
The aim of our study was to describe the course of the autonomic nerves of the pararectal space and their anatomical relationship with the posterior mesh fixation zone on the levator ani muscle.
Study design
Twenty hemi-pelvis specimens from 10 fresh female cadavers were dissected. We measured the distance between the posterior mesh fixation zone on the levator ani, and the nearest point of adjacent structures: the hypogastric nerve, inferior hypogastric plexus, uterosacral ligament, uterine artery, and ureter. Measurements were repeated starting from the inferior hypogastric plexus.
Results
Nerve fibers of the inferior hypogastric plexus spread out systematically above the superior aspect of the levator ani muscle. Median distance from the posterior mesh fixation zone and the inferior hypogastric plexus was around 2.8 (range 2.1–3.5) cm.
Conclusions
The inferior hypogastric plexus lies above the superior aspect of the levator ani muscle. A short distance between the posterior mesh fixation zone on the levator ani muscle and inferior hypogastric plexus could explain in part postoperative digestive symptoms. These observations support the development of nerve-sparing procedures for posterior mesh placement in the context of pelvic organ prolapse repair and suggest that postoperative complications could be improved by changing the fixation zone.




Similar content being viewed by others
References
Acsinte OM, Rabischong B, Bourdel N, Canis M, Botchorishvili R (2018) Laparoscopic promontofixation in 10 steps. J Minim Invasive Gynecol 25:767. https://doi.org/10.1016/j.jmig.2017.10.020
Allen RE, Hosker GL, Smith AR, Warrell DW (1990) Pelvic floor damage and childbirth: a neurophysiological study. Br J Obstet Gynaecol 97:770–779. https://doi.org/10.1111/j.1471-0528.1990.tb02570.x
Baader B, Herrmann M (2003) Topography of the pelvic autonomic nervous system and its potential impact on surgical intervention in the pelvis. Clin Anat 16:119–130. https://doi.org/10.1002/ca.10105
Balaya V, Ngo C, Rossi L, Cornou C, Bensaid C, Douard R, Bats AS, Lecuru F (2016) Bases anatomiques et principe du nerve-sparing au cours de l’hystérectomie radicale pour cancer du col utérin. Gynecol Obstet Fertil 44:517–525. https://doi.org/10.1016/j.gyobfe.2016.07.009
Borgmann H, Rodríguez Socarrás M, Salem J, Tsaur I, Gomez Rivas J, Barret E, Tortolero L (2017) Feasibility and safety of augmented reality-assisted urological surgery using smartglass. World J Urol 35:967–972. https://doi.org/10.1007/s00345-016-1956-6
Bui C, Ballester M, Chéreau E, Guillo E, Daraï E (2010) Functional results and quality of life of laparoscopic promontofixation in the cure of genital prolapse. Gynecol Obstet Fertil 38:563–568. https://doi.org/10.1016/j.gyobfe.2010.06.001
Butler-Manuel SA, Buttery LDK, A’Hern RP, Polak JM, Barton DPJ (2002) Pelvic nerve plexus trauma at radical and simple hysterectomy: a quantitative study of nerve types in the uterine supporting ligaments. J Soc Gynecol Investig 9:47–56
Ceccaroni M, Clarizia R, Roviglione G, Ruffo G (2013) Neuro-anatomy of the posterior parametrium and surgical considerations for a nerve-sparing approach in radical pelvic surgery. Surg Endosc 27:4386–4394. https://doi.org/10.1007/s00464-013-3043-z
Chong GO, Lee YH, Hong DG, Cho YL, Park IS, Lee YS (2013) Robot versus laparoscopic nerve-sparing radical hysterectomy for cervical cancer: a comparison of the intraoperative and perioperative results of a single surgeon’s initial experience. Int J Gynecol Cancer 23:1145–1149. https://doi.org/10.1097/IGC.0b013e31829a5db0
Christmann-Schmid C, Koerting I, Ruess E, Faehnle I, Krebs J (2018) Functional outcome after laparoscopic nerve-sparing sacrocolpopexy: a prospective cohort study. Acta Obstet Gynecol Scand 97:744–750. https://doi.org/10.1111/aogs.13337
Coolen A-LWM, van IJsselmuiden MN, van Oudheusden AMJ, Veen J, van Eijndhoven HWF, Mol BWJ, Roovers JP, Bongers MY (2017) Laparoscopic sacrocolpopexy versus vaginal sacrospinous fixation for vaginal vault prolapse, a randomized controlled trial: SALTO-2 trial, study protocol. BMC Womens Health 17:52. https://doi.org/10.1186/s12905-017-0402-2
Cosma S, Petruzzelli P, Danese S, Benedetto C (2017) Nerve preserving vs standard laparoscopic sacropexy: postoperative bowel function. WJGE 9:211. https://doi.org/10.4253/wjge.v9.i5.211
DeLancey JOL (2016) What’s new in the functional anatomy of pelvic organ prolapse? Curr Opin Obstet Gynecol 28:420–429. https://doi.org/10.1097/GCO.0000000000000312
DeLancey JOL, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, Hussain H, Umek W, Hsu Y, Ashton-Miller JA (2007) Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol 109:295–302. https://doi.org/10.1097/01.AOG.0000250901.57095.ba
Ercoli A, Campagna G, Delmas V, Ferrari S, Morciano A, Scambia G, Cervigni M (2016) Anatomical insights into sacrocolpopexy for multicompartment pelvic organ prolapse: anatomical insights into sacrocolpopexy. Neurourol Urodyn 35:813–818. https://doi.org/10.1002/nau.22806
Faucheron J-L (2005) Pelvic anatomy for colorectal surgeons. Acta Chir Belg 105:471–474. https://doi.org/10.1080/00015458.2005.11679762
Fermaut M, Nyangoh Timoh K, Lebacle C, Moszkowicz D, Benoit G, Bessede T (2016) Identification des sites anatomiques à risque de lésion nerveuse lors de chirurgie pour endométriose pelvienne profonde. Gynecol Obstet Fertil 44:302–308. https://doi.org/10.1016/j.gyobfe.2016.03.007
Florian-Rodriguez ME, Hamner JJ, Corton MM (2017) First sacral nerve and anterior longitudinal ligament anatomy: clinical applications during sacrocolpopexy. Am J Obstet Gynecol 217:607.e1-607.e4. https://doi.org/10.1016/j.ajog.2017.07.008
Frankenhäuser F (1867) Die Nerven der Gebaermutter und ihre Endigung in den glatten Muskelfasern
Giraudet G, Protat A, Cosson M (2018) The anatomy of the sacral promontory. Am J Obstet Gynecol 218:457.e1-457.e3. https://doi.org/10.1016/j.ajog.2017.12.236
Gluck O, Blaganje M, Veit-Rubin N, Phillips C, Deprest J, O’reilly B, But I, Moore R, Jeffery S, Haddad JM, Deval B (2019) Laparoscopic sacrocolpopexy: a comprehensive literature review on current practice. Eur J Obstet Gynecol Reprod Biol 245:94–101. https://doi.org/10.1016/j.ejogrb.2019.12.029
Good MM, Abele TA, Balgobin S, Montoya TI, McIntire D, Corton MM (2013) Vascular and ureteral anatomy relative to the midsacral promontory. Am J Obstet Gynecol 208:486.e1-486.e7. https://doi.org/10.1016/j.ajog.2013.02.039
Kamina P (2008) Anatomie Clinique Pierre Kamina Tome 4: organes urinaires et génitaux—pelvis—Coupes du tronc, 2nd edn. Maloine, Paris
Le Normand L, Cosson M, Cour F, Deffieux X, Donon L, Ferry P, Fatton B, Hermieu J-F, Marret H, Meurette G, Cortesse A, Wagner L, Fritel X (2017) Clinical practice guidelines: synthesis of the guidelines for the surgical treatment of primary pelvic organ prolapse in women by the AFU, CNGOF, SIFUD-PP, SNFCP, and SCGP. J Gynecol Obstet Hum Reprod 46:387–391. https://doi.org/10.1016/j.jogoh.2017.05.001
Lee R (1978) On the nervous ganglia of the uterus, and an appendix to a paper on the nervous ganglia of the uterus, with a further account of the nervous structures of that organ. Robert Lee. Philosophical Transactions of the Royal Society of London, part I, pp. 269-275, 1841, and part II, pp. 173-179, 1842. Am J Obstet Gynecol 131:217–218. https://doi.org/10.1016/0002-9378(78)90668-3
Lefranc J-P, Benhaim Y, Lauratet B, Vincens E, Hoff J (2009) Techniques de traitement chirurgical des prolapsus génitaux par voie abdominale. Elsevier Masson, Paris
Li L, Bi Y, Wang L, Mao X, Kraemer B, Lang J, Cui Q, Wu M (2019) Identification and injury to the inferior hypogastric plexus in nerve-sparing radical hysterectomy. Sci Rep 9:13260. https://doi.org/10.1038/s41598-019-49856-w
Lousquy R, Costa P, Delmas V, Haab F (2009) État des lieux de l’épidémiologie des prolapsus génitaux. Prog Urol 19:907–915. https://doi.org/10.1016/j.purol.2009.09.011
Maas CP, Kenter GG, Trimbos JB, Deruiter MC (2005) Anatomical basis for nerve-sparing radical hysterectomy: immunohistochemical study of the pelvic autonomic nerves. Acta Obstet Gynecol Scand 84(9):868–874
Mage G (2013) Chirurgie Coelioscopique en Gynécologie, 2eme edn. Masson
Moroni RM, Juliato CRT, Cosson M, Giraudet G, Brito LGO (2018) Does sacrocolpopexy present heterogeneity in its surgical technique? A systematic review. Neurourol Urodyn 37:2335–2345. https://doi.org/10.1002/nau.23764
Moszkowicz D, Rougier G, Julié C, Nyangoh Timoh K, Beauchet A, Vychnevskaia K, Malafosse R, Nordlinger B, Peschaud F (2016) Total mesorectal excision for cancer: histological and immunohistochemical evidence of nerve removal and risk-factor analysis. Colorectal Dis 18:O367–O375. https://doi.org/10.1111/codi.13501
Neto JS, Siufi DF, Magrina JF (2015) Robotic nerve-sparing radical hysterectomy. Minerva Ginecol 67:281–287
Nyangoh Timoh K, Moszkowicz D, Zaitouna M, Lebacle C, Martinovic J, Diallo D, Creze M, Lavoue V, Darai E, Benoit G, Bessede T (2018) Detailed muscular structure and neural control anatomy of the levator ani muscle: a study based on female human fetuses. Am J Obstet Gynecol 218:121.e1-121.e12. https://doi.org/10.1016/j.ajog.2017.09.021
Paek J, Kang E, Lim PC (2019) Comparative analysis of genitourinary function after type C1 robotic nerve-sparing radical hysterectomy versus type C2 robotic radical hysterectomy. Surg Oncol 30:58–62. https://doi.org/10.1016/j.suronc.2019.05.003
Peschaud F, Moszkowicz D, Alsaid B, Bessede T, Penna C, Benoit G (2012) Preservation of genital innervation in women during total mesorectal excision: which anterior plane? World J Surg 36:201–207. https://doi.org/10.1007/s00268-011-1313-2
Ripperda CM, Jackson LA, Phelan JN, Carrick KS, Corton MM (2017) Anatomic relationships of the pelvic autonomic nervous system in female cadavers: clinical applications to pelvic surgery. Am J Obstet Gynecol 216:388.e1-388.e7. https://doi.org/10.1016/j.ajog.2016.12.002
Schaub M, Lecointre L, Faller E, Boisramé T, Baldauf J-J, Wattiez A, Akladios CY (2017) Laparoscopic sacral colpopexy: the “6-points” technique. J Minim Invasive Gynecol 24:1081–1082. https://doi.org/10.1016/j.jmig.2017.04.003
Schneider A, Pezold S, Saner A, Ebbing J, Wyler S, Rosenthal R, Cattin PC (2014) Augmented reality assisted laparoscopic partial nephrectomy. Med Image Comput Comput Assist Interv 17:357–364. https://doi.org/10.1007/978-3-319-10470-6_45
Spackman R, Wrigley B, Roberts A, Quinn M (2007) The inferior hypogastric plexus: a different view. J Obstet Gynaecol 27:130–133. https://doi.org/10.1080/01443610601113839
Villot A, Pizzoferrato A-C, Longie A, Paniel B-J, Fauconnier A (2020) Technical considerations and mid-term follow-up after vaginal hysterocolpectomy with colpocleisis for pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol 247:73–79. https://doi.org/10.1016/j.ejogrb.2020.02.001
Zhang J, Feng L, Lu Y, Guo D, Xi T, Wang X (2013) Distribution of lymphatic tissues and autonomic nerves in supporting ligaments around the cervix uteri. Mol Med Rep 7:1458–1464. https://doi.org/10.3892/mmr.2013.1360
Author information
Authors and Affiliations
Contributions
Manuscript writing: RG, CG. Revisions: AH, UC, CM, MG, LV, MX, NTK, CG. Dissections work: RG, AH, FA, TK, CG. Figure 3: CM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
Pr Geoffroy Canlorbe, Pr Vincent Lavoué and Dr Gaby Moawad: Proctor for Intuitive Surgical.
Condensation
We studied relationships between the inferior hypogastric plexus and the mesh fixation zone on the Levator ani muscle used for posterior sacrocolpopexy.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Table 1.
Rights and permissions
About this article
Cite this article
Rocher, G., Azaïs, H., Favier, A. et al. Relationships between pelvic nerves and levator ani muscle for posterior sacrocolpopexy: an anatomic study. Surg Radiol Anat 44, 891–898 (2022). https://doi.org/10.1007/s00276-022-02955-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-022-02955-2