Abstract
Purpose
Hypnosis is useful for diminishing distress during medical procedures. This study investigated the efficacy of virtually augmented self-hypnosis as an adjunctive non-pharmacological method for procedural pain and anxiety relief during endovascular interventions (EVI).
Methods
We compared an immersive distraction experience (clinicaltrials.gov identifier NCT04561596) featuring virtual reality (VR) using a head-mounted display versus treatment as usual (TAU). Patients followed the “Aqua” module (Oncomfort™) consisting of a scuba dive and breathing exercises. They experienced a self-induced dissociative state similar to clinical hypnosis without direct intervention of a professional. Enrollment followed a 1:1 randomized open study (VR or TAU). Patients’ feelings were evaluated just before and after the procedure, and 3 months following intervention. Anxiety was evaluated using the State Trait Anxiety Inventory (STAI) and pain (sensory, emotional, and memory) with a visual analogue scale (VAS).
Results
This study included 100 patients. Mean anxiety (pre-post) was significantly reduced within groups and between groups (difference of 4.2 points, p = 0.016). The percentage of responders to anxiety lowering were 76 and 46% for VR and TAU, respectively (p = 0.004). The two groups did not significantly differ in mean sensory-intensity and affective emotional pain (pre-post) using VAS, in negative memories concerning remembered pain at 3 months (difference > 1 from immediate post-procedural reported pain intensity), mean procedural time, or the need for analgesic or sedative drugs.
Conclusions
VR self-hypnosis has the potential to improve the management of patients’ distress during radiological procedures. It is safe and effective for reducing anxiety during EVI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the development of catheter-based techniques, endovascular interventions (EVI) are frequently considered as first-line treatment instead of open surgery [1]. The cost containment of interventional radiology (IR) technology also contributes to the success of EVI and enables procedures of increasing number and complexity [2]. This results in higher demand for sedation facilities, as EVI procedures are principally performed with level 1–2 sedation and analgesia [2]. With a large number of interventions conducted under local anesthesia, pain and anxiety management is highly important [3].
Among patients needing cardiovascular surgery, 30% report high anxiety levels [4, 5]. Considering the setting of radiological facilities, increased anxiety due to the machines must also be considered [6]. Medical anxiety and pain management carry some risks and may present with a range of associated side effects [2, 7]. Additionally, drugs (e.g., lorazepam) are also fallible in terms of anxiety reduction [8].
Therefore, the management of pain and anxiety through non-pharmacological media has been explored—with hypnosis being of particular interest [9]. Nowadays, hypnoanalgesia is available in all French teaching hospitals [10]. Hypnotic suggestion aims to capture attention through a dissociation mechanism of prefrontal and cingulate cortex [11]. In the operating model of the interruptive function of pain, pain is considered information. One may need to select the pain information by giving it some attention. Since attention is considered a limited resource dividable between tasks, exceeding this limit may result in slowed, stopped, or flawed thought and behavior [12].
In persons who have difficulties with imagination and absorption, the use of 3D virtual reality (VR) is helpful [13]. VR brings the illusion of being in and of the virtual environment—a concept called immersion [14]. The first work on VR was in 1968, within a military context [15]. Sutherland presents the basis of a head-mounted display (HMD) displaying 3D information around the user. In the following decades, the HMD was further developed by the Air Force [16] and NASA [17]. In 1989, the first commercial HMD was manufactured [18]. This popularization brought the use of virtual environments in medicine during the 1990s, especially oriented toward surgical simulations [19,20,21,22].
In the late 1990s, immersiveness through an HMD was considered for use in anxiety [23]. Oyama et al. [24] addressed the possibility of using a virtual reality approach for support against anxiety in palliative medicine. VR has also been considered for treatment of phobia [25]. VR is especially interesting in the context of limited resources. While tailored patient management through clinical hypnosis specialists is restricted, VR may allow a substantial number of patients to benefit from hypnosis [13]. However, only scarce data are available from clinical practice, especially in the IR setting.
In the present study, we aimed to determine the potential benefits of virtually augmented self-hypnosis (VA-HYPO) to manage pain and anxiety in the context of EVI.
Materials and Methods
Patients
The Swiss Association of Research Ethics Committees approved the study protocol (BASEC-ID 2020–00728) and it was registered on ClinicalTrials.gov (identifier NCT04561596).
For enrollment, we considered all consecutive patients over 18 years old and referred to the radiology department for peripheral endovascular interventions (EVI) under local anesthesia (angiography, phlebography, arterial intervention, and venous intervention). Candidates were excluded if they had limited language comprehension, important visual impairment, or were deaf. We also excluded those with a history of motion sickness or psychiatric disease (paranoia, schizophrenia, deep water phobia, dementia), or if they required sedative medication. As the study was conducted during the COVID-19 pandemic, we also excluded all patients with severe acute respiratory syndrome.
Procedure
Beforehand written informed consent was obtained from each patient. Both groups received an identical consent process comprising a treatment explanation given some days before the procedure or the day of the procedure.
The day of the intervention, the investigator introduced the patient to the pre-operative anxiety and pain questionnaire (anxiety, pain intensity, and pain pleasantness). Upon the patient’s arrival in the operating room, the VR mask was installed on the patient’s head and they were trained in how to use the autohypnosis software.
The EVI procedure was performed as usual, except that the autohypnosis software ran during the whole intervention. If needed, medication was provided during the intervention. All interventional procedures were performed following the standard of care. The operators were the same in both groups.
After the intervention, the patient filled out the post-operative questionnaire. Patients were instructed to report anxiety and pain felt during the intervention (anxiety, pain intensity and pleasantness).
At 3 month post-operation, during a clinical visit or through a phone conversation, patients were asked to complete a third questionnaire concerning their remembered anxiety and pain during the intervention (anxiety, pain intensity and pleasantness).
The control intervention was usual patient care for participants in the TAU group. The questionnaires were given the same manner as in VA-HYPO group.
Materials
The self-hypnosis device used was the OnComfort-Sedakit™ (Oncomfort, Wavre, Brabant-Wallon, Belgique). This medical device comprises an HMD mask Samsung Gear VR powered by Oculus with a Samsung S7 mobile phone (Samsung Electronics, Seoul, South-Korea) or Pico G2 (PICO-interactive, Qingdao, Shandong, China), and headphones for tone and noise reduction.
The virtual reality software displays an underwater world. A whale swims in front of the user, inviting him to breathe at the frequency of its tail. A prerecorded discourse guides the patient through autohypnosis. To maximize the effects of VR, it is important to let the patient concentrate on the session. Thus, verbal communication is avoided, although people can freely speak if necessary. Throughout the experience, the patients can move their head freely to explore the virtual environment. A relaxed state is facilitated by binaural beats [26], and breath exercises based on cardiac coherence [27].
The operator can select the duration beforehand, this determines the length of the different hypnotic phases (i.e., induction, deepening, suggestion, and return). The duration may also be shortened or prolonged per-procedure [28].
Data Collection
We recorded demographic and procedural data (age, sex, anxiety, pain, duration and type), and security and satisfaction aspects (administration of drugs for pain and anxiety, per-procedure need to remove the mask, readiness to renew the VR experiment, and cybersickness events (claustrophobia, disorientation, dizziness, sweating, or sleepiness)).
Anxiety was measured using the Spielberger Anxiety State Inventory (STAI) [29], comprising 20 items, with a total ranging from 20–80 (higher score indicates higher anxiety level). Pain was measured using a visual analogue scale, ranging from 0 (no pain) to 10 (highest pain). Three different scales were evaluated: sensory discriminative (intensity), affective motivational (pleasantness), and cognitive evaluative (memory) [30].
The minimal clinical difference (MCD) regarding anxiety on STAI was a change > 0.5 standard deviation, a cut-off allowing binary differentiation of responders and non-responders [31]. The MCD regarding pain on VAS was defined as a change > 1.9 point [32]. Pain intensiveness MCD responders were dichotomized following this criteria. The MCD regarding negative memories (i.e., the relationship between a stressful event and subsequently increased distress linked to reminders of the event) on VAS was a change ≥ 1 point between interventional (intensiveness) pain and accuracy of its recall during follow-up survey [33]. Responders were dichotomized accordingly.
Statistical Analysis and Randomization
A recent RCT in the setting of breast cancer treatment [34] found that VR yielded a 9% decrease of anxiety. Assuming a higher standard deviation and lower anxiety reduction due to the higher variability of the vascular procedures, we conducted a power analysis to identify a sample size that could determine a significant decrease of 5% in anxiety. Thirty-two patients per group was sufficient, to avoid loss of power due to missing information, we included 50 patients per group.
Statistical analyses were conducted using STATA v.16.1 (Stata Corp., Texas, USA), including the Wilcoxon Mann–Whitney rank sum test and Wilcoxon matched-pairs signed-rank, after verifying the distribution of continuous variables. Fisher’s exact or chi-squared tests were used for categorical variables.
Open-label randomization was performed using a 1:1 allocation ratio to interventions with a computer random number generator and allocation concealment through sequentially numbered opaque sealed envelopes.
Results
From October 2020 to August 2022, 1752 patients were screened, of whom 100 consecutive patients were assigned to the TAU group or VA-HYPO group (Fig. 1). The high number of patients screened was due to the reduced number of procedures performed during the COVID-19 pandemic, with more morbid patients than usual. The procedure was successful in all patients: 50 men and 50 women, with a mean age of 47.4 years (SD: 16.8 years; range: 18–84 years).
The two study groups did not significantly differ in baseline demographics (Table 1). Indications for EVI included venous interventions, such as implanted port stripping, peripherally inserted central catheters, and cava filters (97%); and arterial interventions, such as embolization and angioplasty (3%) (Table 1).
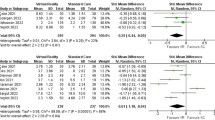
Anxiety was significantly lower after the procedure than before. The intragroup difference between pre- and post-procedural scores was 11.2 for VA-HYPO and 7 for TAU (p < 0.001). The intergroup difference (between the intragroup differences) was 4.2 (p = 0.016), equivalent to an effect size of 0.44 (small effect) [35]. MCD responders comprised 46% of TAU and 76% of VA-HYPO (p = 0.004) (Table 2).
Pain (VAS) scores did not reach significance. For TAU and VA-HYPO, respectively, procedural pain was 2.6 and 2.0 for pain intensity, and 2.6 and 2.5 for pain pleasantness. Table 1 presents details.
The proportion of MCD responders did not significantly differ between TAU and VA-HYPO for clinically relevant intensity during the procedure (30%) (Table 2), for negative memories (assessed at the 3-month time-point) (47% TAU vs 40% VA-HYPO) (Table 2).
The two groups also did not significantly differ in mean procedural time (43 min), or need for analgesic or sedative drugs (3 vs. 1 for TAU vs. VA-HYPO) (Table 3). The amount of local anesthesia given in each procedure varied between 5 and 10 ml of 1% lidocaine.
The VA-HYPO group experienced two cybersickness events: dizziness and face sweating. Among the patients, 90% were ready to renew the experiment (Table 3).
Discussion
Several prior studies have assessed the efficacy of VR over TAU, especially for burn wound care, thus using VR with a scope directed toward distraction without a hypnosis state. Two reviews highlight VR-associated reductions of pain and anxiety [30, 36].
In terms of pain, episiotomy repair procedures have demonstrated significant differences between VR and standard care [37] while cystoscopy procedures did not yield differences [38].
In the fields of venipuncture or port access procedures, prior studies presented equivocal results when comparing VR and TAU. Two studies reported significant pain reduction [39, 40] while two had non-significant diminution [41, 42], as our study showed.
As previously described [41], we found a low degree of pain during the venous procedure. Moreover, the item regarding procedural drug administration provided little additional information in our study. No sedation was given in almost all patients meaning that the procedures were simple ones. Thus, there remains a need for more distressing studies focusing on more complex interventional procedures (i.e., more prolonged and/or with potentially higher risk).
Professional VR users may also try to enhance the efficiency of hypnotic analgesia. Selecting only patients with high hypnotic susceptibility, using a scale such as the Harvard Group Scale of Hypnotic Susceptibility [43], would enable the identification of patients who will benefit the most from technology. Another way to improve adhesion would be to allow patients to self-select the VA-HYPO program [44], although this effect has not been tested due to our rigid protocol using a unique program.
In terms of anxiety, as in our study, a large study of venipuncture found a significant reduction of anxiety between VR and standard of care groups using VAS (1.9 vs. 2.48) [39]. In contrast, some authors have not demonstrated significant differences between VR and standard care. These studies have included groups of around 20 participants for port access procedures and cystoscopy [38, 41]. Thus, the difference from our results may be due to their underpowered sampling.
Negative memories linked to prior traumatizing procedures may lead to difficulties in patient management. Although our results did not demonstrate an effect on painful memories (which could be linked to the low procedural pain), lowering anxiety represents a cardinal management point, since higher anxiety levels are a unique factor generating negative pain memories [45].
Immersive reality may lead to cybersickness due to sensory mismatch, postural instability, and gravity discrepancy [46]. It has effects similar to motion sickness but without physical movements. Its frequency is highly variable depending on the virtual environment, settings, and display systems [46, 47]. Two previous studies mention cybersickness rates of ~ 10% [39, 48]. Our low sickness rate may be explained by technological improvements rather than short duration of HMD use (20', around half of procedure time), since cybersickness mostly occurs during the first twenty minutes [48].
Qualitatively, the participants tolerated the HMD, as there was no need to remove it during any procedure. Similar to previous findings [49], the readiness to reuse virtual reality in future interventions exceeded 90%, showing the patients’ high degree of satisfaction.
There was no difference in procedure time, but all procedures performed under VA-HYPO led to patient dissociation from the intervenient (the patient was focused on the virtual session with minimal external interactions). This may contribute to the facilitation and securing of the operator’s work, by eliminating micro-interpersonal interruptions during the procedure [30].
Within the context of interventional radiology, our results support the use of VA-HYPO. As previously mentioned [50], VA-HYPO use is an interesting alternative for multiple reasons. First, eliminating the need of a physically present hypnotist. Second, hypnosis may be delivered on demand, targeting the patient’s expectations, in a standardized way, without prior professional training. Nevertheless, its use remains limited for patients presenting head wounds or bandages, and those suffering from motion sickness or claustrophobia. Finally, it largely empowers the patient in the self-management of pain and anxiety.
This study has several limitations. First, the “case mix” of procedures that have been performed is not fully representative of the range of endovascular interventions realized in interventional radiology. Second, the STAI questionnaire has some limitations in the discrimination between anxiety and depression, and may have poor discriminant validity regarding anxiety in elderly persons [51]. Third, the use of quantitative measures of stress with a biological marker, such as salivary cortisol [52], may be less subjective and provide more robust data. Finally, a Hawthorne effect [53] may not be totally excluded in the VR group, although it seems unlikely due to the significance of anxiety results but not pain results. As well this study is one of the largest in the field with a rigorous RCT design [54, 55], overcoming potential confounding factors of quasi-experimental design.
Conclusion
These trial findings are related to simple endovascular procedures. By significantly reducing per-procedural anxiety, VR self-hypnosis has the potential to improve the management of patient’s distress. It is safe and effective for reducing anxiety during EVI. There remains a need for more powerful studies focusing on more complex procedures.
References
Akopian G, Katz SG. Peripheral angioplasty with same-day discharge in patients with intermittent claudication. J Vasc Surg. 2006;44:115–8.
Romagnoli S, Fanelli F, Barbani F, Uberoi R, Esteban E, Lee MJ, et al. CIRSE standards of practice on analgesia and sedation for interventional radiology in adults. Cardiovasc Intervent Radiol. 2020;43:1251–60.
Oh J, Sohn J-H, Shin CS, Na SH, Yoon H-J, Kim J-J, et al. Mutual relationship between anxiety and pain in the intensive care unit and its effect on medications. J Crit Care. 2015;30:1043–8.
Gonçalves KKN, da Silva JI, Gomes ET, de Pinheiro LLS, Figueiredo TR, da Bezerra SMMS. Anxiety in the preoperative period of heart surgery. Rev Bras Enferm Associação Brasileira de Enfermagem. 2016;69:397–403.
Hernández-Palazón J, Fuentes-García D, Falcón-Araña L, Roca-Calvo MJ, Burguillos-López S, Doménech-Asensi P, et al. Assessment of preoperative anxiety in cardiac surgery patients lacking a history of anxiety: contributing factors and postoperative morbidity. J Cardiothorac Vasc Anesth. 2018;32:236–44.
Qanadli SD, Gudmundsson L, Gullo G, Ponti A, Saltiel S, Jouannic A-M, et al. Virtually augmented self-hypnosis applied to endovascular interventions (VA-HYPO): randomized controlled trial protocol. PLOS ONE. 2022;17:e0263002.
Lang EV, Hamilton D. Anodyne imagery: an alternative to i.v. sedation in interventional radiology. AJR Am J Roentgenol. 1994;162:1221–6.
Stamenkovic DM, Rancic NK, Latas MB, Neskovic V, Rondovic GM, Wu JD, et al. Preoperative anxiety and implications on postoperative recovery: what can we do to change our history. Minerva Anestesiol. 2018;84:1307–17.
Lang EV, Benotsch EG, Fick LJ, Lutgendorf S, Berbaum ML, Berbaum KS, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures: a randomised trial. The Lancet. 2000;355:1486–90.
Chabridon G, Nekrouf N, Bioy A. État des lieux des pratiques actuelles de l’hypnose au sein des centres hospitaliers universitaires français. /data/revues/00137006/unassign/S0013700616301798/ [Internet]. 2016 [cited 2020 Jan 30]; Available from: https://www.em-consulte.com/en/article/1080325
Jamieson GA, Sheehan PW. An empirical test of Woody and Bowers’s dissociated-control theory of hypnosis. Int J Clin Exp Hypn Routledge. 2004;52:232–49.
Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol Bull. 1999;125:356–66.
Askay SW, Patterson DR, Sharar SR. Virtual reality hypnosis. Contemp Hypn. 2009;26:40–7.
Zeltzer D. Autonomy, interaction, and presence. Presence Teleoperators Virtual Environ. 1992;1:127–32.
Sutherland IE. A head-mounted three dimensional display. Proc Dec 9–11 1968 Fall Jt Comput Conf Part I [Internet]. New York, NY, USA: Association for Computing Machinery; 1968 [cited 2022 Jul 16]. p. 757–64. Available from: https://doi.org/10.1145/1476589.1476686
Furness TA. The super cockpit and its human factors challenges. Proc Hum Factors Soc Annu Meet SAGE Publications. 1986;30:48–52.
Fisher SS, McGreevy M, Humphries J, Robinett W. Virtual environment display system. Proc 1986 Workshop Interact 3D Graph [Internet]. New York, NY, USA: Association for Computing Machinery; 1987 [cited 2022 Jul 17]. p. 77–87. Available from: https://doi.org/10.1145/319120.319127
Virtual BF, Technology R. Virtual reality technology. A Tutorial J Commun. 1992;42:23–72.
Dumay AC, Jense GJ. Endoscopic surgery simulation in a virtual environment. Comput Biol Med. 1995;25:139–48.
O’Toole RV, Playter RR, Krummel TM, Blank WC, Cornelius NH, Roberts WR, et al. Measuring and developing suturing technique with a virtual reality surgical simulator11All authors, except Krummel, have an affiliation with Boston dynamics Inc., an organization that has a financial interest in the editorial content discussed in the manuscript. J Am Coll Surg. 1999;189:114–27.
Pieper SD, Delp S, Rosen J, Fisher SS. Virtual environment system for simulation of leg surgery. Stereosc Disp Appl II [Internet]. SPIE; 1991 [cited 2022 Jul 18]. p. 188–97. Available from: https://www.spiedigitallibrary.org/conference-proceedings-of-spie/1457/0000/Virtual-environment-system-for-simulation-of-leg-surgery/https://doi.org/10.1117/12.46307.full
Satava RM. Virtual reality surgical simulator. The First Steps Surg Endosc. 1993;7:203–5.
Wiederhold BK, Davis R, Wiederhold MD. The effects of immersiveness on physiology. Stud Health Technol Inform. 1998;58:52–60.
Oyama H, Wakao F, Okamura H. Virtual reality support system in palliative medicine. Stud Health Technol Inform. 1997;39:60–3.
Garcia-Palacios A, Hoffman H, Carlin A, Furness TA, Botella C. Virtual reality in the treatment of spider phobia: a controlled study. Behav Res Ther. 2002;40:983–93.
Wahbeh H, Calabrese C, Zwickey H. Binaural beat technology in humans: a pilot study to assess psychologic and physiologic effects. J Altern Complement Med. 2007;13:25–32.
De Jonckheere J, Ibarissene I, Flocteil M, Logier R. A smartphone based cardiac coherence biofeedback system. Annu Int Conf IEEE Eng Med Biol Soc. 2014;2014:4791–4.
Otte JL, Carpenter JS, Roberts L, Elkins GR. Self-hypnosis for sleep disturbances in menopausal women. J Womens Health. 2020;29:461–3.
Gauthier J, Bouchard S. Adaptation canadienne-française de la forme révisée du state-trait anxiety inventory de Spielberger [a French-Canadian adaptation of the revised version of Spielberger’s state-trait anxiety inventory.]. Can J Behav Sci Rev Can Sci Comport. 1993;25:559–78.
Scapin S, Echevarría-Guanilo ME, Boeira Fuculo PR, Gonçalves N, Rocha PK, Coimbra R. Virtual reality in the treatment of burn patients: a systematic review. Burns J Int Soc Burn Inj. 2018;44:1403–16.
Tashjian VC, Mosadeghi S, Howard AR, Lopez M, Dupuy T, Reid M, et al. Virtual Reality for Management of Pain in Hospitalized Patients: Results of a Controlled Trial. JMIR Ment Health [Internet]. 2017 [cited 2020 Jan 30];4. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5390112/
Bird SB, Dickson EW. Clinically significant changes in pain along the visual analog scale. Ann Emerg Med. 2001;38:639–43.
Chen E, Zeltzer LK, Craske MG, Katz ER. Children’s memories for painful cancer treatment procedures: implications for distress. Child Dev. 2000;71:933–47.
Chirico A, Maiorano P, Indovina P, Milanese C, Giordano GG, Alivernini F, et al. Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J Cell Physiol [Internet]. 2020 [cited 2020 Feb 7];n/a. Available from: https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1002/jcp.29422
Sawilowsky S. New effect size rules of thumb. J Mod Appl Stat Methods. 2009;8:597–9.
Scheffler M, Koranyi S, Meissner W, Strauß B, Rosendahl J. Efficacy of non-pharmacological interventions for procedural pain relief in adults undergoing burn wound care: a systematic review and meta-analysis of randomized controlled trials. Burns. 2018;44:1709–20.
JahaniShoorab N, Ebrahimzadeh Zagami S, Nahvi A, Mazluom SR, Golmakani N, Talebi M, et al. The effect of virtual reality on pain in primiparity women during episiotomy repair: a randomize clinical trial. Iran J Med Sci. 2015;40:219–24.
Walker MR, Kallingal GJS, Musser JE, Folen R, Stetz MC, Clark JY. Treatment efficacy of virtual reality distraction in the reduction of pain and anxiety during cystoscopy. Mil Med. 2014;179:891–6.
Gold JI, Mahrer NE. Is virtual reality ready for prime time in the medical space? a randomized control trial of pediatric virtual reality for acute procedural pain management. J Pediatr Psychol. 2018;43:266–75.
Wolitzky K, Fivush R, Zimand E, Hodges L, Rothbaum BO. Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychol Health Routledge. 2005;20:817–24.
Gershon J, Zimand E, Pickering M, Rothbaum BO, Hodges L. A pilot and feasibility study of virtual reality as a distraction for children with cancer. J Am Acad Child Adolesc Psychiatry. 2004;43:1243–9.
Nilsson S, Finnström B, Kokinsky E, Enskär K. The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. Eur J Oncol Nurs. 2009;13:102–9.
Enea V, Dafinoiu I, Opriş D, David D. Effects of hypnotic analgesia and virtual reality on the reduction of experimental pain among high and low hypnotizables. Int J Clin Exp Hypn. 2014;62:360–77.
Windich-Biermeier A, Sjoberg I, Dale JC, Eshelman D, Guzzetta CE. Effects of distraction on pain, fear, and distress during venous port access and venipuncture in children and adolescents with cancer. J Pediatr Oncol Nurs Off J Assoc Pediatr Oncol Nurses. 2007;24:8–19.
Noel M, Chambers CT, McGrath PJ, Klein RM, Stewart SH. The role of state anxiety in children’s memories for pain. J Pediatr Psychol. 2012;37:567–79.
Rebenitsch L, Owen C. Review on cybersickness in applications and visual displays. Virtual Real. 2016;20:101–25.
Nichols S, Patel H. Health and safety implications of virtual reality: a review of empirical evidence. Appl Ergon. 2002;33:251–71.
Stanney KM, Lanham DS, Kennedy RS, Breaux R. Virtual environment exposure drop-out thresholds. Proc Hum Factors Ergon Soc Annu Meet. 1999;43:1223–7.
Sander Wint S, Eshelman D, Steele J, Guzzetta CE. Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer. Oncol Nurs Forum. 2002;29:E8-15.
Cornelis FH, Najdawi M, Ben Ammar M, Nouri-Neuville M, Lombart B, Lotz J-P, et al Integrative Medicine in Interventional Oncology: A Virtuous Alliance. Medicina (Mex) [Internet]. 2020 [cited 2021 May 18];56. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7022725/
Julian LJ. Measures of anxiety: state-trait anxiety inventory (STAI), beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res. 2011;63:S467–72.
Bozovic D, Racic M, Ivkovic N. Salivary cortisol levels as a biological marker of stress reaction. Med Arch Sarajevo Bosnia Herzeg. 2013;67:374–7.
Spiegel B, Fuller G, Lopez M, Dupuy T, Noah B, Howard A, et al Virtual reality for management of pain in hospitalized patients: A randomized comparative effectiveness trial. PLoS ONE [Internet]. 2019 [cited 2020 Jan 30];14. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6693733/
Chan E, Foster S, Sambell R, Leong P. Clinical efficacy of virtual reality for acute procedural pain management: a systematic review and meta-analysis. PLOS ONE. 2018;13:0200987.
Pourmand A, Davis S, Lee D, Barber S, Sikka N. Emerging utility of virtual reality as a multidisciplinary tool in clinical medicine. Games Health J. 2017;6:263–70.
Funding
Open access funding provided by University of Lausanne.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors of this manuscript declare that there are no secondary (competing) interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Institutional Review Board (IRB) approval was obtained. The study protocol was approved by national ethical committee (BASEC 2020–00728) and is registered in ClinicalTrials.gov (NCT04561596).
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gullo, G., Rotzinger, D.C., Colin, A. et al. Virtually Augmented Self-Hypnosis in Peripheral Vascular Intervention: A Randomized Controlled Trial. Cardiovasc Intervent Radiol 46, 786–793 (2023). https://doi.org/10.1007/s00270-023-03394-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03394-1