Abstract
Background
The fragility index (FI) is defined as the minimum number of patients or subjects needed to switch experimental groups for statistical significance to be lost in a randomized control trial (RCT). This index is used to determine the robustness of a study’s findings and recently as a measure of evaluating RCT quality. The objective of this review was to identify and describe published systematic reviews utilizing FI to evaluate surgical RCTs and to determine if there were common factors associated with higher FI values.
Methods
Three databases (PubMed, MEDLINE [Ovid], Embase) were searched, followed by a subsequent abstract/title and full-text screening to yield 50 reviews of surgical RCTs. Authors, year of publication, name of journal, study design, number of RCTs, subspecialty, sample size, median FI, patients lost to follow-up, and associations between variables and FI scores were collected.
Results
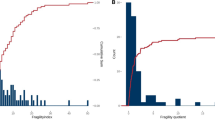
Among 1007 of 2214 RCTs in 50 reviews reporting FI (median sample size 100), the pooled median FI was 3 (IQR: 1–7). Most reviews investigated orthopaedic surgery RCTs (n = 32). There was a moderate correlation between FI and p value (r = 0.-413), a mild correlation between FI and sample size (r = 0.188), and a mild correlation between FI and event number (r = 0.129).
Conclusion
Based on a limited sample of systematic reviews, surgical RCT FI values are still low (2–5). Future RCTs in surgery require improvement to study design in order to increase the robustness of statistically significant findings.

Similar content being viewed by others
References
Maldonado DR, Go CC, Huang BH et al (2021) The fragility index of hip arthroscopy randomized controlled trials: a systematic survey. Arthrosc Tech 37(6):1983–1989
Khormaee S, Choe J, Ruzbarsky JJ et al (2018) The fragility of statistically significant results in pediatric orthopaedic randomized controlled trials as quantified by the fragility index: a systematic review. J Pediatr Orthop 38(8):e418–e423
Herndon CL, McCormick KL, Gazgalis A et al (2021) Fragility Index as a measure of randomized clinical trial quality in adult reconstruction: a systematic review. Arthroplast Today 11:239–251
Walsh M, Srinathan SK, McAuley DF et al (2014) The statistical significance of randomized controlled trial results is frequently fragile: a case for a fragility Index. J Clin Epidemiol 67(6):622–628
Hegazy MA, El Nahas W, Roshdy S (2011) Surgical outcome of modified versus conventional parotidectomy in treatment of benign parotid tumors. J Surg Oncol 103(2):163–168
Marasco D, Russo J, Izzo A et al (2021) Static versus dynamic fixation of distal tibiofibular syndesmosis: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc 29(11):3534–3542
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Kung J, Chiappelli F, Cajulis OO et al (2010) From systematic reviews to clinical recommendations for evidence-based health care: validation of revised assessment of multiple systematic reviews (R-AMSTAR) for grading of clinical relevance. Open Dent J 4:84–91
Anand S, Kainth D (2021) Fragility index of recently published meta-analyses in pediatric urology: a striking observation. Cureus 13(7):e16225
Bowers A, Meyer C, Tritz D et al (2018) Assessing quality of randomized trials supporting guidelines for laparoscopic and endoscopic surgery. J Surg Res 224:233–239
Budhiraja P, Kaplan B, Kalot M et al (2022) Current state of evidence on kidney transplantation: how fragile are the results. Transplantation 106(2):248–256
Carroll AH, Rigor P, Wright MA et al (2022) Fragility of randomized controlled trials on treatment of proximal humeral fracture. J Shoulder Elbow Surg 31(8):1610–1616
Checketts JX, Scott JT, Meyer C et al (2018) The robustness of trials that guide evidence-based orthopaedic surgery. J Bone Joint Surg Am 100(12):e85
Chertin L, Burman I, Haifler M (2021) Urologic oncology randomized controlled trials are frequently fragile—A review of the urology literature. Urol Oncol 39(10):735.e1-735.e8
Chin B, Copeland A, Gallo L et al (2019) The fragility of statistically significant randomized controlled trials in plastic surgery. Plast Reconstr Surg 144(5):1238–1245
Constant M, Trofa DP, Saltzman BM et al (2021) The fragility of statistical significance in patellofemoral instability research: a systematic review. Am J Sports Med. https://doi.org/10.1177/03635465211039202
Davey MS, Hurley ET, Doyle TR et al (2022) The fragility index of statistically significant findings from randomized controlled trials comparing the management strategies of anterior shoulder instability. Am J Sports Med. https://doi.org/10.1177/03635465221077268
Ehlers CB, Curley AJ, Fackler NP et al (2021) The statistical fragility of hamstring versus patellar tendon autografts for anterior cruciate ligament reconstruction: a systematic review of comparative studies. Am J Sports Med 49(10):2827–2833
Ehlers CB, Curley AJ, Fackler NP et al (2021) The statistical fragility of single-bundle vs double-bundle autografts for ACL reconstruction: a systematic review of comparative studies. Orthop J Sports Med 9(12):23259671211064624
Ekhtiari S, Gazendam AM, Nucci NW et al (2021) The fragility of statistically significant findings from randomized controlled trials in hip and knee arthroplasty. J Arthroplast 36(6):2211-2218.e1
Evaniew N, Files C, Smith C et al (2015) The fragility of statistically significant findings from randomized trials in spine surgery: a systematic survey. Spine J 15(10):2188–2197
Forrester LA, Jang E, Lawson MM et al (2020) Statistical fragility of surgical and procedural clinical trials in orthopaedic oncology. J Am Acad Orthop Surg Glob Res Rev 4(6):e19.00152
Forrester LA, McCormick KL, Bonsignore-Opp L et al (2021) Statistical fragility of surgical clinical trials in orthopaedic trauma. J Am Acad Orthop Surg Glob Res Rev 5(11):e20.00197
Gnech M, Lovatt CA, McGrath M et al (2019) Quality of reporting and fragility index for randomized controlled trials in the vesicoureteral reflux literature: Where do we stand? J Pediatr Urol 15(3):204–212
Go CC, Maldonado DR, Go BC et al (2022) The fragility index of total hip arthroplasty randomized control trials: a systematic review. J Am Acad Orthop Surg 30(9):e741–e750
Khan M, Evaniew N, Gichuru M et al (2017) The fragility of statistically significant findings from randomized trials in sports surgery: a systematic survey. Am J Sports Med 45(9):2164–2170
Kyriakides PW, Schultz BJ, Egol K et al (2021) The fragility and reverse fragility indices of proximal humerus fracture randomized controlled trials: a systematic review. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-021-01684-2
Li B, Kong I, McGrath M et al (2021) Evaluating the literature on preoperative androgen stimulation for hypospadias repair using the fragility index - can we trust observational studies. J Pediatr Urol 17(5):661–669
McCormick KL, Tedesco LJ, Swindell HW et al (2021) Statistical fragility of randomized clinical trials in shoulder arthroplasty. J Shoulder Elbow Surg 30(8):1787–1793
Megafu M, Megafu E (2022) The fragility of statistical findings in distal radius fractures: a systematic review of randomized controlled trials. Injury 53(10):3352–3356
Morris SC, Gowd AK, Agarwalla A et al (2022) Fragility of statistically significant findings from randomized clinical trials of surgical treatment of humeral shaft fractures: a systematic review. World J Orthop 13(9):825–836
Muthu S, Ramakrishnan E (2021) Fragility analysis of statistically significant outcomes of randomized control trials in spine surgery: a systematic review. Spine (Phila Pa 1976) 46(3):198–208
Narayan VM, Gandhi S, Chrouser K et al (2018) The fragility of statistically significant findings from randomized controlled trials in the urological literature. BJU Int 122(1):160–166
Nelms DW, Vargas HD, Bedi RS et al (2022) When the p value doesn’t cut it: the fragility index applied to randomized controlled trials in colorectal surgery. Dis Colon Rectum 65(2):276–283
Noel CW, McMullen C, Yao C et al (2018) The fragility of statistically significant findings from randomized trials in head and neck surgery. Laryngoscope 128(9):2094–2100
Parisien RL, Dashe J, Cronin PK et al (2019) Statistical significance in trauma research: too unstable to trust. J Orthop Trauma 33(12):e466–e470
Parisien RL, Trofa DP, Dashe J et al (2019) Statistical fragility and the role of p values in the sports medicine literature. J Am Acad Orthop Surg 27(7):e324–e329
Parisien RL, Ehlers C, Cusano A et al (2021) The statistical fragility of platelet-rich plasma in rotator cuff surgery: a systematic review and meta-analysis. Am J Sports Med 49(12):3437–3442
Parisien RL, Danford NC, Jarin IJ et al (2021) The fragility of statistical findings in achilles tendon injury research: a systematic review. J Am Acad Orthop Surg Glob Res Rev 5(9):e21.00018
Parisien RL, Constant M, Saltzman BM, et al (2021) The fragility of statistical significance in cartilage restoration of the knee: a systematic review of randomized controlled trials. Cartilage 13(1_suppl):147S-155S.
Parisien RL, Trofa DP, O’Connor M et al (2021) The fragility of significance in the hip arthroscopy literature: a systematic review. JBJS Open Access 6(4):e21.00035
Parisien RL, Trofa DP, Cronin PK et al (2021) Comparative studies in the shoulder literature lack statistical robustness: a fragility analysis. Arthrosc Sports Med Rehabil 3(6):e1899–e1904
Pascoal E, Liu M, Lin L et al (2022) The fragility of statistically significant results in gynaecologic surgery: a systematic review. J Obstet Gynaecol Can 44(5):508–514
Rickard M, Lorenzo AJ, Hannick JH et al (2019) Over-reliance on p values in urology: fragility of findings in the hydronephrosis literature calls for systematic reporting of robustness indicators. Urology 133:204–210
Robinson T, Al-Shahwani N, Easterbrook B et al (2020) The fragility of statistically significant findings from randomized controlled trials in pediatric appendicitis: a systematic review. J Pediatr Surg 55(5):800–804
Robinson NB, Fremes S, Hameed I et al (2021) Characteristics of Randomized clinical trials in surgery from 2008 to 2020: a systematic review. JAMA Netw Open 4(6):e2114494
Ruzbarsky JJ, Khormaee S, Rauck RC et al (2019) Fragility of randomized clinical trials of treatment of clavicular fractures. J Shoulder Elbow Surg 28(3):415–422
Ruzbarsky JJ, Rauck RC, Manzi J et al (2019) The fragility of findings of randomized controlled trials in shoulder and elbow surgery. J Shoulder Elbow Surg 28(12):2409–2417
Ruzbarsky JJ, Khormaee S, Daluiski A (2019) The fragility index in hand surgery randomized controlled trials. J Hand Surg Am 44(8):698.e1-698.e7
Schröder A, Muensterer OJ, Oetzmann VC (2021) Meta-analyses in paediatric surgery are often fragile: implications and consequences. Pediatr Surg Int 37(3):363–367
Shen C, Shamsudeen I, Farrokhyar F et al (2018) Fragility of results in ophthalmology randomized controlled trials: a systematic review. Ophthalmology 125(5):642–648
Skinner M, Tritz D, Farahani C et al (2019) The fragility of statistically significant results in otolaryngology randomized trials. Am J Otolaryngol 40(1):61–66
Svantesson E, Hamrin SE, Danielsson A et al (2020) Strength in numbers? The fragility index of studies from the Scandinavian knee ligament registries. Knee Surg Sports Traumatol Arthrosc 28(2):339–352
Tignanelli CJ, Napolitano LM (2019) The fragility index in randomized clinical trials as a means of optimizing patient Care. JAMA Surg 154(1):74–79
Shochet LR, Kerr PG, Polkinghorne KR (2017) The fragility of significant results underscores the need of larger randomized controlled trials in nephrology. Kidney Int 92(6):1469–1475
Docherty KF, Campbell RT, Jhund PS et al (2017) How robust are clinical trials in heart failure. Eur Heart J 38(5):338–345
Chase KB, Matt VB (2017) Unbreakable? An analysis of the fragility of randomized trials that support diabetes treatment guidelines. Diabetes Res Clin Pract 134:91–105
Adie S, Harris IA, Naylor JM et al (2017) The quality of surgical versus non-surgical randomized controlled trials. Contemp Clin Trials Commun 5:63–66
Maggard MA, O’Connell JB, Liu JH et al (2003) Sample size calculations in surgery: are they done correctly? Surgery 134(2):275–279
Ioannidis JPA (2018) The proposal to lower p value thresholds to 005. JAMA 319(14):1429–1430
Lydersen S, Pradhan V, Senchaudhuri P et al (2007) Choice of test for association in small sample unordered r x c tables. Stat Med 26(23):4328–4343
Yusuf S, Peto R, Lewis J et al (1985) Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 27(5):335–371
Bomze D, Asher N, Hasan AO et al (2020) Survival-inferred fragility index of phase 3 clinical trials evaluating immune checkpoint inhibitors. JAMA Netw Open 3(10):e2017675
ESCP EAGLE Safe Anastomosis Collaborative. (2021) ESCP Safe Anastomosis ProGramme in CoLorectal SurgEry (EAGLE): study protocol for an international cluster randomised trial of a quality improvement intervention to reduce anastomotic leak following right colectomy. Colorectal Dis 23(10):2761-2771. doi:https://doi.org/10.1111/codi.15806
Andrade C (2020) The use and limitations of the fragility index in the interpretation of clinical trial findings. J Clin Psychiatr 81(2):20f13334
Acknowledgements
This work was not supported by a federal or commercial grant, and there were no other authors who were of direct help in the reported work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No financial support was received for this manuscript preparation and submission, and there are no relevant conflicts of interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vivekanantha, P., Shah, A., Hoit, G. et al. Predictors of Increased Fragility Index Scores in Surgical Randomized Controlled Trials: An Umbrella Review. World J Surg 47, 1163–1173 (2023). https://doi.org/10.1007/s00268-023-06928-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-06928-3