Abstract
Background
The quality of evidence of the orthopedic literature has been often called into question. The fragility index (FI) has emerged as a means to evaluate the robustness of a significant result. Similarly, reverse fragility index (RFI) can be used for nonsignificant results to evaluate whether one can confidently conclude that there is no difference between groups. The analysis of FI and RFI in proximal humerus fracture (PHF) management is of particular interest, given ongoing controversy regarding optimal management and patient selection. The aim of this study was to report the FI, RFI and quality of the evidence in the proximal humerus fracture literature.
Methods
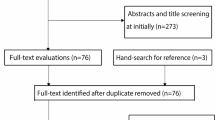
A systematic review was conducted based on the PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines, which utilized EMBASE, MEDLINE and Cochrane Library databases. Inclusion criteria included randomized controlled clinical trials related to the management of proximal humerus fractures, published from 2000 to 2020 with dichotomous outcome measures and 1:1 allocation. The FI and RFI were calculated by successively changing one nonevent to an event for each outcome measure until the result was made nonsignificant or significant, respectively. The fragility quotient, (FQ), calculated by dividing the FI by the total sample size, was calculated as well.
Results
There were 25 studies that met our criteria with 48 outcome measures recorded. A total of 21 studies had at least one fragile result, with ten studies including a fragile result in the conclusion of the abstract. A total of 31 outcome measures had nonsignificant results and the median RFI was found to be 4, with 71% greater than number of patients lost to follow up. Seventeen outcomes had significant results, with a median FI of 1, with 65% greater than or equal to the number patients lost to follow up. A total of 18 of 25 studies (72%) included a power analysis. In particular, ten studies reported a statistical analysis of complication rates, 90% of which were fragile. The median FQ was found to be 0.037.
Conclusions
The literature on PHF management is frequently fragile. Outcome measures are often fragile, particularly with regards to comparing complication rates and reoperation rates in treatment arms. Comparing to the studies in other subspecialties PHF RCTs are relatively more fragile and underpowered. Standardized reporting of FI, FQ and RFI can help the reader to reliably draw conclusions based on the fragility of outcome measures.
Similar content being viewed by others
Reference
Lefaivre KA, Slobogean GP. Understanding systematic reviews and meta-analyses in orthopaedics. J Am Acad Orthop Surg. 2013;21(4):245–55. Doi: https://search.datacite.org/works/https://doi.org/10.5435/jaaos-21-04-245. Accessed 18 Nov 2020
Walsh M, Srinathan SK, McAuley DF, et al. The statistical significance of randomized controlled trial results is frequently fragile: a case for a fragility index. J Clin Epidemiol. 2014;67(6):622–8. https://doi.org/10.1016/j.jclinepi.2013.10.019. Accessed 18 Nov 2020
Evaniew N, Files C, Smith C, et al. The fragility of statistically significant findings from randomized trials in spine surgery: a systematic survey. Spine J. 2015;15(10):2188–97. https://doi.org/10.1016/j.spinee.2015.06.004.
Schumaier A, Grawe B. Proximal humerus fractures: evaluation and management in the elderly patient. Geriatr Orthop Surg Rehabil. 2018;9. Doi: https://doi.org/10.1177/2151458517750516. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5788098/. Accessed 18 Nov 2020.
Ruzbarsky JJ, Rauck RC, Manzi J, Khormaee S, Jivanelli B, Warren RF. The fragility of findings of randomized controlled trials in shoulder and elbow surgery. J Shoulder Elbow Surg. 2019;28(12):2409–17. https://doi.org/10.1016/j.jse.2019.04.051.
Checketts JX, Scott JT, Meyer C, Horn J, Jones J, Vassar M. The robustness of trials that guide evidence-based orthopaedic surgery. J Bone Jt Surg Am. 2018;100(12):e85. https://doi.org/10.2106/JBJS.17.01039.
Khan MS, Fonarow GC, Friede T, et al. Application of the reverse fragility index to statistically nonsignificant randomized clinical trial results. JAMA Netw Open. 2020;3(8). Doi: https://doi.org/10.1001/jamanetworkopen.2020.12469. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7407075/. Accessed 19 Nov 2020.
Beks RB, Ochen Y, Frima H, et al. Operative versus nonoperative treatment of proximal humeral fractures: a systematic review, meta-analysis, and comparison of observational studies and randomized controlled trials. J Shoulder Elbow Surg. 2018;27(8):1526–34. https://doi.org/10.1016/j.jse.2018.03.009.
Soler-Peiro M, García-Martínez L, Aguilella L, Perez-Bermejo M. Conservative treatment of 3-part and 4-part proximal humeral fractures: a systematic review. J Orthop Surg Res. 2020;15(1):347. https://doi.org/10.1186/s13018-020-01880-7.
Ong CC, Kwon YW, Walsh M, Davidovitch R, Zuckerman JD, Egol KA. Outcomes of open reduction and internal fixation of proximal humerus fractures managed with locking plates. Am J Orthop (Belle Mead NJ). 2012;41(9):407–12.
Robinson CM, Stirling PHC, Goudie EB, MacDonald DJ, Strelzow JA. Complications and long-term outcomes of open reduction and plate fixation of proximal humeral fractures. J Bone Jt Surg Am. 2019;101(23):2129–39. https://doi.org/10.2106/JBJS.19.00595.
Lekic N, Montero N, Takemoto R, Davidovitch R, Egol K. Treatment of two-part proximal humerus fractures: intramedullary nail compared to locked plating. HSS J. 2012;8(2):86–91. Doi: https://doi.org/10.1007/s11420-012-9274-z. https://www.ncbi.nlm.nih.gov/pubmed/23874244. Accessed 18 Nov 2020
Hasty EK, Jernigan EW, Soo A, Varkey DT, Kamath GV. Trends in surgical management and costs for operative treatment of proximal humerus fractures in the elderly. Orthopedics. 2017;40(4):e641–7. https://doi.org/10.3928/01477447-20170411-03.
Khatib O, Onyekwelu I, Yu S, Zuckerman JD. Shoulder arthroplasty in New York state, 1991 to 2010: changing patterns of utilization. J Shoulder Elbow Surg. 2015;24(10):286. https://doi.org/10.1016/j.jse.2015.05.038.
Floyd SB, Campbell J, Chapman CG, Thigpen CA, Kissenberth MJ, Brooks JM. Geographic variation in the treatment of proximal humerus fracture: an update on surgery rates and treatment consensus. J Orthop Surg Res. 2019;14(1):22. https://doi.org/10.1186/s13018-018-1052-2.
Bomze D, Meirson T. A critique of the fragility index. Lancet Oncol. 2019;20(10):e551. https://doi.org/10.1016/S1470-2045(19)30582-0.
Rouleau DM, Balg F, Benoit B, et al. Deltopectoral vs. deltoid split approach for proximal HUmerus fracture fixation with locking plate: a prospective randomized study (HURA). J Shoulder Elbow Surg. 2020;29(11):2190–9. https://doi.org/10.1016/j.jse.2020.06.020.
Buecking B, Mohr J, Bockmann B, Zettl R, Ruchholtz S. Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures? Clin Orthop Relat Res. 2014;472(5):1576–85. https://doi.org/10.1007/s11999-013-3415-7.
Agorastides I, Sinopidis C, El Meligy M, Yin Q, Brownson P, Frostick SP. Early versus late mobilization after hemiarthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2007;16(3 Suppl):33. https://doi.org/10.1016/j.jse.2006.07.004.
Lefevre-Colau MM, Babinet A, Fayad F, et al. Immediate mobilization compared with conventional immobilization for the impacted nonoperatively treated proximal humeral fracture. A randomized controlled trial. J Bone Jt Surg Am. 2007;89(12):2582–90. https://doi.org/10.2106/JBJS.F.01419.
Carbone S, Razzano C, Albino P, Mezzoprete R. Immediate intensive mobilization compared with immediate conventional mobilization for the impacted osteoporotic conservatively treated proximal humeral fracture: a randomized controlled trial. Musculoskelet Surg. 2017;101(Suppl 2):137–43. https://doi.org/10.1007/s12306-017-0483-y.
Chen X, Yu Z, Wang H, et al. Proximal humeral internal locking plate combined with a custom neutral-position shoulder and elbow sling for proximal humerus fractures: a randomized study. Medicine (Baltimore). 2019;98(17):e15271. https://doi.org/10.1097/MD.0000000000015271.
Hengg C, Nijs S, Klopfer T, et al. Cement augmentation of the proximal humerus internal locking system in elderly patients: a multicenter randomized controlled trial. Arch Orthop Trauma Surg. 2019;139(7):927–42. https://doi.org/10.1007/s00402-019-03142-6.
Peng C, Wang H, Yan J, Song T. Locking system strengthened by biomimetic mineralized collagen putty for the treatment of osteoporotic proximal humeral fractures. Regen Biomater. 2017;4(5):289–94. https://doi.org/10.1093/rb/rbx016.
Biermann N, Schirren M, Siebenbürger G, et al. Glenohumeral joint lavage does not affect clinical outcomes in open reduction and internal fixation of displaced intracapsular proximal humeral fractures: a prospective, randomized, double-blinded trial. J Shoulder Elbow Surg. 2020;29(9):1758–64. https://doi.org/10.1016/j.jse.2020.04.026.
Jin L, Guo J, Guo J, Yin Y, Hou Z, Zhang Y. Clinical effects of the probing method with depth gauge for determining the screw depth of locking proximal humeral plate. Biomed Res Int. 2016;2016:5898161. https://doi.org/10.1155/2016/5898161.
Soliman OA, Koptan WMT. Proximal humeral fractures treated with hemiarthroplasty: does tenodesis of the long head of the biceps improve results? Injury. 2013;44(4):461–4. https://doi.org/10.1016/j.injury.2012.09.012.
Sohn H, Jeon YS, Lee J, Shin S. Clinical comparison between open plating and minimally invasive plate osteosynthesis for displaced proximal humeral fractures: a prospective randomized controlled trial. Injury. 2017;48(6):1175–82. https://doi.org/10.1016/j.injury.2017.03.027.
Zhang L, Zheng J, Wang W, et al. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop. 2011;35(11):1655–61. https://doi.org/10.1007/s00264-011-1227-5.
Gracitelli MEC, Malavolta EA, Assunção JH, et al. Locking intramedullary nails compared with locking plates for two- and three-part proximal humeral surgical neck fractures: a randomized controlled trial. J Shoulder Elbow Surg. 2016;25(5):695–703. https://doi.org/10.1016/j.jse.2016.02.003.
Plath JE, Kerschbaum C, Seebauer T, et al. Locking nail versus locking plate for proximal humeral fracture fixation in an elderly population: a prospective randomised controlled trial. BMC Musculoskelet Disord. 2019;20(1):20. https://doi.org/10.1186/s12891-019-2399-1.
Helfen T, Siebenbürger G, Fleischhacker E, Gleich J, Böcker W, Ockert B. Operative treatment of 2-part surgical neck type fractures of the proximal humerus in the elderly: cement augmented locking plate PHILOSTM vs. proximal humerus nail multiloc®. Injury. 2020;51(10):2245–52. https://doi.org/10.1016/j.injury.2020.06.026.
Zhu Y, Lu Y, Shen J, Zhang J, Jiang C. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Jt Surg Am. 2011;93(2):159–68. https://doi.org/10.2106/JBJS.J.00155.
Lopiz Y, Garcia-Coiradas J, Garcia-Fernandez C, Marco F. Proximal humerus nailing: a randomized clinical trial between curvilinear and straight nails. J Shoulder Elbow Surg. 2014;23(3):369–76. https://doi.org/10.1016/j.jse.2013.08.023.
Chen H, Ji X, Gao Y, et al. Comparison of intramedullary fibular allograft with locking compression plate versus shoulder hemi-arthroplasty for repair of osteoporotic four-part proximal humerus fracture: consecutive, prospective, controlled, and comparative study. Orthop Traumatol Surg Res. 2016;102(3):287–92. https://doi.org/10.1016/j.otsr.2015.12.021.
Fialka C, Stampfl P, Arbes S, Reuter P, Oberleitner G, Vécsei V. Primary hemiarthroplasty in four-part fractures of the proximal humerus: randomized trial of two different implant systems. J Shoulder Elbow Surg. 2008;17(2):210–5. https://doi.org/10.1016/j.jse.2007.07.002.
Sebastiá-Forcada E, Cebrián-Gómez R, Lizaur-Utrilla A, Gil-Guillén V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg. 2014;23(10):1419–26. https://doi.org/10.1016/j.jse.2014.06.035.
Lopiz Y, Alcobia-Diaz B, Galan-Olleros M, Garcia-Fernandez C, Picado AL, Marco F. Reverse shoulder arthroplasty versus nonoperative treatment for 3- or 4-part proximal humeral fractures in elderly patients: a prospective randomized controlled trial. J Shoulder Elbow Surg. 2019;28(12):59–2271 (S1058-2746(19)30465-3[pii]).
Rangan A, Handoll H, Brealey S, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA. 2015;313(10):1037–47. https://doi.org/10.1001/jama.2015.1629.
Handoll H, Brealey S, Rangan A, et al. The ProFHER (PROximal fracture of the humerus: evaluation by randomisation) trial—a pragmatic multicentre randomised controlled trial evaluating the clinical effectiveness and cost-effectiveness of surgical compared with non-surgical treatment for proximal fracture of the humerus in adults. Health Technol Assess. 2015;19(24):1–280. https://doi.org/10.3310/hta19240.
Launonen AP, Sumrein BO, Reito A, et al. Operative versus non-operative treatment for 2-part proximal humerus fracture: a multicenter randomized controlled trial. PLoS Med. 2019;16(7):e1002855. https://doi.org/10.1371/journal.pmed.1002855.
Parisien RL, Dashe J, Cronin PK, Bhandari M, Tornetta P. Statistical significance in trauma research: too unstable to trust? J Orthop Trauma. 2019;33(12):e466–70. https://doi.org/10.1097/BOT.0000000000001595.
Khormaee S, Choe J, Ruzbarsky JJ, et al. The fragility of statistically significant results in pediatric orthopaedic randomized controlled trials as quantified by the fragility index: a systematic review. J Pediatr Orthop. 2018;38(8):e418–23. https://doi.org/10.1097/BPO.0000000000001201.
Parisien RL, Trofa DP, Dashe J, et al. Statistical fragility and the role of P values in the sports medicine literature. J Am Acad Orthop Surg. 2019;27(7):e324–9. https://doi.org/10.5435/JAAOS-D-17-00636.
Ruzbarsky JJ, Khormaee S, Daluiski A. The fragility index in hand surgery randomized controlled trials. J Hand Surg Am. 2019;44(8):698.e1-e7. https://doi.org/10.1016/j.jhsa.2018.10.005.
Forrester LA, Jang E, Lawson MM, Capi A, Tyler WK. Statistical fragility of surgical and procedural clinical trials in orthopaedic oncology. J Am Acad Orthop Surg Glob Res Rev. 2020. https://doi.org/10.5435/JAAOSGlobal-D-19-00152.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Peter Kyriakides declares that he has no conflicts of interest. Blake Schultz declares that he has no conflicts of interest. Kenneth Egol declares that he has no conflicts of interest. Philipp Leucht declares he has no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kyriakides, P.W., Schultz, B.J., Egol, K. et al. The fragility and reverse fragility indices of proximal humerus fracture randomized controlled trials: a systematic review. Eur J Trauma Emerg Surg 48, 4545–4552 (2022). https://doi.org/10.1007/s00068-021-01684-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01684-2