Abstract
Background
Although recommendations exist for patients to be offered a post-operative helpline or telephone follow-up appointment at discharge after cholecystectomy, implementation of these is resource-intensive. Whilst the benefits of telephone follow-up are well documented, the use of digital modalities is less so. We aimed to identify if digital follow-up (DFU) was equivalent to routine care with telephone follow-up (TFU), for patients undergoing elective laparoscopic cholecystectomy.
Methods
All patients listed for elective laparoscopic cholecystectomy between August 2016 and March 2018 were offered routine post-operative care (TFU or no follow-up) or DFU at a tertiary referral centre in Nottingham.
Results
Of 597 patients undergoing laparoscopic cholecystectomy, 199 (33.3%) opted for TFU, and 98 (16.4%) for DFU. DFU was completed for 85 (86.7%) participants and TFU for 125 (62.8%), p < 0.0001. Over 5 times as many patients who chose TFU missed their appointment compared to DFU (5.6% vs. 30.9%, p < 0.001). At 30-days post-operatively, patients undergoing TFU had significantly more post-operative wound infections identified then those undergoing DFU (17.6% vs 5.9%, p = 0.01). However, this did not impact the incidence of 30-day readmissions between groups (7.2% TFU vs. 7.1% DFU). No complications were missed by either the DFU or TFU modalities. DFU was completed significantly earlier than TFU (median 6 days vs. 13.5 days, p = 0.001) with high patient acceptability, identifying complications and alerting clinicians to those patients requiring an early review.
Conclusion
This feasibility study has demonstrated that digital follow-up is an acceptable alternative to telephone follow-up after elective laparoscopic cholecystectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over 60,000 cholecystectomies are performed in the UK each year [1], with laparoscopic cholecystectomy being performed predominantly as a day-case procedure [2]. Whilst most institutions no longer offer routine post-operative follow-up, there are national guidelines recommending that either a post-operative helpline or telephone follow-up (TFU) appointment is provided at discharge [3]. The significant benefits of TFU are well documented, including increased patient satisfaction [4,5,6,7,8], reduced patient anxiety [4], reduced expenses and travel time for patients to reach hospital outpatient follow-up appointments [7], and reduced hospital costs in running a physical outpatient clinic service [5, 9]. Loss of follow-up also precludes necessary feedback for surgeons and a missed opportunity to guide learning and a change in practice [10].
Telemedicine and TFU, although less resource-intensive than physical follow-up appointments, still requires the use of trained health care professionals when compared with no follow-up, resources which are already stretched in the current National Health Service (NHS) and could be better used [9, 11].
Prior to Covid-19, the NHS aimed to deliver more health care remotely through the introduction of new technologies such as the NHS App [12]. This enables health care professionals in secondary care to communicate with patients and share information on their mobile devices at a time and place of their choosing. Integrating care locally [13] continues to be a priority and is even more important since the start of the pandemic. Despite advances in modern technology, little research has been undertaken to explore alternative modalities for post-operative follow-up, especially given that automated follow-up can minimise staffing, and the necessity for fixed appointment times.
The aim of this study was to identify if digital follow-up (DFU) using an online platform, was equivalent to routine care with telephone follow-up (TFU), for patients undergoing elective laparoscopic cholecystectomy. Primary objectives were to identify the incidence of 30-day post-operative complications identified by DFU compared with TFU. Secondary objectives were to identify the incidence of 30-day readmissions, reoperations, and the incidence of missed complications, in addition to follow-up compliance between groups.
Methods
Study design and setting
This prospective cohort study was conducted in a large NHS trust with tertiary centre capabilities. All patients listed for elective laparoscopic cholecystectomy between August 2016 and March 2018 were given free choice on whether they opted to use post-operative DFU or routine post-operative care. Routine care included TFU at the Nottingham City Hospital site, and no follow-up at the Queen’s Medical Centre and Circle Treatment Centre sites. The study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [14].
Study groups
Participants were recruited to participate in this study on referral to hospital for management of symptomatic gallstones. On receiving study information either postally or in person, each participant indicated their consent to participate digitally.
Digital follow-up
Access to the DFU survey was automated once participants had confirmation of an operation date and were discharged from hospital. Internally coded information technology links with the Nottingham University Hospitals NHS Trust (NUH) Patient Administration System (PAS) and the online platform meant that admission and discharge dates for surgery were inputted automatically. The entire process was overseen by a researcher to ensure no system glitches throughout.
Study participants registering for DFU received a system-automated email to complete a digital survey at 7 days post-operatively, and one further reminder for non-responders at day 10.
The 7-day follow-up survey (Table 1) consisted of 12 questions in six categories. Each question was allocated a score, with a score of 3 or more in any one category, or an overall score of greater than 9 from the total of all 12 questions coded to trigger a call-back. Although participants were not informed of their score, they were immediately informed of the outcome of their score by one of two automated videos:
Video 1: Reassured and discharged:
Participants were provided with a downloadable patient recovery information sheet and contact details for a specialist nurse should they need.
Video 2: Telephone call-back within 24 h:
Participants were informed they would receive a telephone consultation within 24 h. They were also provided with a downloadable patient recovery information sheet and contact details for a specialist nurse.
Participant scores following completed DFU surveys were forwarded to the trial researcher who was then able to track responses and conduct TFU where appropriate.
Telephone follow-up
Participants who opted for TFU were called between post-operative day 10 and 14 by one of three surgical care practitioners (SCPs). These were pre-booked appointment slots arranged with the patient on discharge from hospital. SCPs are trained health care professionals with prior registration as either an operating department practitioner or registered nurse with more than 5 years of post-registration experience.
Prospective audit was conducted for all patients. Data on complications, readmissions, reoperations, and mortality were taken from patient clinical notes, the PAS record of hospital attendances, and participant interview. Information on attendances to primary care, walk-in centres and other hospitals was, therefore, limited.
Outcomes
The outcome measures monitored included 30-day post-operative complications, 30-day readmissions, re-operations, and missed post-operative complications, and follow-up compliance.
Variables
Data on patient and hospital characteristics were collected, including patient age, sex, Charlson comorbidity index (CCI) [15], body mass index (BMI), and total length of hospital stay.
Statistical analysis
Data were analysed using GraphPad Prism® version 8.3.0 (GraphPad Software LLC, San Diego, CA, USA.). Differences between groups were evaluated using either Fisher’s exact test or chi-squared tests for categorical variables and Mann–Whitney tests for continuous variables. Differences were considered significant at p < 0.05.
Ethics
This study was a part of PhD project sponsored by NUH, through a collaboration with EIDO Healthcare Limited and The Royal College of Surgeons of England. The study proposal was appraised by the confidentiality advisory group: 16/CAG/0045, with public and patient involvement, and research ethics committee application: 16/SW/0088. It was registered with ClinicalTrials.gov: NCT02810860, and NUH research and innovation: 15GS002.
Results
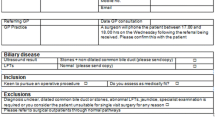
A total of 898 eligible patients were invited to participate in the study and use the digital platform across the three NUH sites. Some 607 (67.6%) patients went on to undergo cholecystectomy, with the remainder having non-operative management (Details and exclusions in Fig. 1).
Participant recruitment (STROBE diagram). DNA: Did not attend (patient missed their appointment despite prompting). *Non-standard operation = open cholecystectomy, laparoscopic cholecystectomy combined with another operation such as liver resection or gastric bypass. **Excluded = follow-up performed at ≥ 31 days post-operatively
Patient recruitment
Half (49.7%) of all patients undergoing laparoscopic cholecystectomy were offered post-operative follow-up. One third (33%) were offered DFU and two-thirds (67%) were offered TFU.
Of the patients who opted for follow-up, significantly more patients missed their TFU than DFU appointments (30.9% [n = 56], vs. 5.6% [n = 5], p < 0.001).
Patient demographics
Both follow-up and no follow-up groups were equally matched, as were DFU and TFU groups (Table 2).
Follow-up versus no follow-up
30-day complications
Significantly more complications were identified by patient follow-up than no follow-up (Table 3). In particular, the incidence of port-site wound infections and constipation were greater in the follow-up group.
30-day readmissions and reoperations
Only 15 (7.1%) of all 63 complications in the follow-up group required attendance (including review in the surgical admissions unit), and 2 (0.9%) a return to theatre. Only 3 (1.4%) of the readmissions were identified at follow-up (Table 4).
Digital follow-up versus telephone follow-up
30-Day complications
Significantly more post-operative wound infections were identified by TFU than DFU (Table 3).
30-Day readmissions and reoperations
Only 6 of all 22 complications (7.1% of the 85 DFU participants) in the DFU group required readmission, and 1 a return to theatre. Only 3 of the readmissions were identified at follow-up (Table 4). Conversely, 9 of all 41 complications (7.2% of the 125 TFU participants) in the TFU group required readmission, and 1 a return to theatre. None of these were identified at follow-up.
Complications not identified at follow-up
No complications were missed by either the DFU or TFU modalities. Complications not identified were those which occurred either before follow-up was offered or after follow-up was completed. Early complications (Participants 1, 2, and 8–15) occurred before follow-up, late complications (Participants 3–7, and 16) occurred after follow-up. Complications identified after follow-up were either not present at the time of follow-up (Participants 4, 6, and 7) or identified at the time of follow-up with patients given appropriate advice should the complication evolve with time (Participants 3, 5, and 16) (Table 5).
Digital follow-up survey
Post-operative follow-up was completed significantly earlier with DFU then TFU (median 6 days [IQR 5–11 days] vs. 13.5 days [IQR 6.7–22 days], p = 0.001).
A breakdown of DFU survey scores can be seen in Supplementary Table 1, with a summary of category scores in Fig. 2a and total scores in Fig. 2b.
a Complications identified by digital follow-up survey: category scores. Cumulative scores for each category of the post-operative digital follow-up questionnaire. Scores ≥ 3 (shown in red) for each category triggered participants to have telephone follow-up. b Complications identified by digital follow-up survey: total scores. Cumulative scores for all 12 questions of the post-operative digital follow-up questionnaire. Scores ≥ 9 (shown in red) overall triggered participants to have telephone follow-up
All 15 participants who received a telephone call back following completion of their DFU survey expressed satisfaction in using the platform as an alternative to no follow-up or a physical follow-up. Comments included “removing the cost and need to find hospital parking”, “extra reassurance”, “having the option for downloadable recovery information”, and “being able to review information at any time”. Problems described by participants did not centre around the follow-up process but physical access to the online platform which provided the DFU. Specifically, problems were with regard to registration on the site and log-in which was not intuitive due to multiple security factors (email, password, two type-sensitive memorable security words).
Discussion
This feasibility study has demonstrated that utilizing a DFU system is a viable alternative to TFU in participants undergoing elective laparoscopic cholecystectomy.
Participant demographics
There were no statistically significant differences in participant variables between no follow-up and follow-up groups. Differences in total length of hospital stay after surgery could be explained due to differences in case complexity as the QMC site mainly has inpatient cholecystectomies performed by hepatobiliary surgeons. These participants with more technically difficult operations may experience a longer length of hospital stay, and in-hospital reviews; therefore, not warranting follow-up, or resulting in alternative follow-up arrangements not captured by this study. Unfortunately, operative difficulty was not collected as part of this study which would be a useful correlation [16], especially whilst analysing total length of hospital stay. The DFU and TFU groups were equally matched for participant and hospital specific variables.
30-Day complications
Follow-up versus no follow-up
As expected, follow-up groups had significantly more complications identified at 30-days post-operatively than no follow-up groups. This would coincide with the fact that in this observational study participants who received follow-up were not only actively tracked but also reviewed either by telephone consultation or in person. Thus, even the smallest of complications, such as surgical site infections and the development of constipation were logged and monitored. Conversely obtaining data on no follow-up participants was a little less transparent involving prospective audit whilst in hospital, and then monitoring of PAS and health care records for recorded planned and unplanned admissions and treatments. Resultantly more subtle complications may have been managed in the community and therefore missed for the purposes of this study.
Digital versus telephone follow-up
Participants who received TFU had greater recorded surgical site infections than those who underwent DFU. Although DFU participants were closely monitored throughout the study, not all DFU participants received a telephone interview and, therefore, the more subtle features of a wound infection may have been missed on our automated survey. However, many of the wound infections identified by TFU received only verbal advice on wound care as opposed to the necessity for hospital or general practitioner attendance or a course of antibiotics, and therefore the extra complications identified at TFU were potentially insignificant.
30-Day readmission and reoperation
Overall numbers for readmission and reoperation at 30-days were small, and therefore although there were no significant differences between follow-up and no follow-up groups, the study was likely underpowered to comment. On review of national data however, 30-day readmission rates are quoted at 5.4–8.2%, and reoperation rates of 0.6–0.8% [2], exactly as seen in this study.
Mortality
As expected, there were no deaths in any group. This is in keeping with mortality being a poor outcome measure for cholecystectomy research given its low incidence [2, 17, 18].
Missed complications
No complications were missed nor were complications falsely identified in either DFU or TFU groups. This suggests that the automated DFU survey and associated scoring system is a safe alternative to conventional TFU.
The additional benefit of DFU is that the speed and ease of completion of follow-up surveys means that they could be offered at multiple post-operative time points to fully capture any possible early or late complications, such as those not captured in this study. Additionally, the digital process could be amended to facilitate a patient-triggered follow-up to aid earlier identification of those patients who may be developing a complication or need earlier clinician input. Such patient-triggered follow-up questionnaires could inform and give patients access to acute surgical triage units to ensure the timely admission and assessment of patients.
Missed appointments
Participants who were offered DFU were significantly more likely to complete their follow-up than those offered TFU. This was even though participants in both groups had opted in for their chosen follow-up modality. Additionally, TFU participants had a pre-arranged date and time for their follow-up appointment which was not only confirmed on discharge but also posted to participants. Despite this, 30.9% versus 5.6% (p < 0.001) of participants missed their TFU compared with DFU appointments.
This may have been because DFU was the more convenient modality, as prior studies have commented on participants missing TFU appointments due to participants resting [4], incorrect telephone numbers [7], hospital admissions [7], or resuming their normal activities such as a return to work. Participants undergoing DFU also received an email informing them that their follow-up was due to be completed, and a further reminder if they had still not done so. This also meant that DFU was completed much earlier than TFU; a median of 6 days versus 13.5 days, respectively.
Study strengths and limitations
Despite difficulties with participant recruitment and retention due to log-in difficulties required to complete the DFU survey, participants demonstrated a willingness to use DFU after laparoscopic cholecystectomy. Users described the availability of DFU and access to the digital platform as informative, reassuring, and convenient. Although it was not able to capture significant early complications it was able to capture feedback on more minor complications such as surgical site infections. In addition to providing useful feedback for surgeons, the timely management of these complications can also prevent more significant problems for patients. Patients with complications also reported improved care as completed DFU questionnaires triggered telephone appointments, discussion with specialists, and physical appointments without the trouble of arranging general practitioner appointments or walk-in centre waits.
Although this study provides practical, real-world information on the use of physician assisted DFU post-operatively, further research is necessary before its mainstream use, in particular a powered study to ensure that all groups are matched to ensure no missed complications. Due to third party data restrictions, we were unable to collect information on participant socio-economic status, which would have been useful to highlight any biases with DFU use.
Future work
At a time where NHS resources are limited [19, 20], an automated follow-up process using DFU may reduce the need for resource intensive physical follow-up or TFU appointments.
Future work should compare matched groups of patients undergoing DFU, TFU, and no follow-up as a randomised controlled trial. Outcomes should include both quantitative and qualitative measures as this study but also consider patient satisfaction surveys, focus groups, and a cost analysis.
References
Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland/Royal College of Surgeons of England (2016) Commissioning Guide: Gallstone Disease. https://www.rcseng.ac.uk/-/media/files/rcs/standards-and-research/commissioning/gallstone-disease-commissioning-guide-for-republication.pdf. Accessed 6 Mar 2022
CholeS Study Group (2016) Population-based cohort study of outcomes following cholecystectomy for benign gallbladder diseases in the UK and Ireland. Br J Surg 103:1704–1715
Bailey CR, Ahuja M, Bartholomew K et al (2019) Guidelines for day-case surgery 2019: guidelines from the association of anaesthetists and the British Association of day surgery. Anaesthesia 74:778–792
Fallis WM, Sucurrah D (2001) Outpatient laparoscopic cholecystectomy: home visit versus telephone follow-up. Can J Surg 44:39–44
Fischer K, Hogan V, Jager A et al (2015) Efficacy and utility of phone call follow-up after pediatric general surgery versus traditional clinic follow-up. Perm J 19:11–14
Gray RT, Sut MK, Badger SA et al (2010) Post-operative telephone review is cost-effective and acceptable to patients. Ulster Med J 79:76–79
Hwa K, Wren SM (2013) Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery. Results of a pilot program. JAMA Surg 148:823–827
Miller A, Barton K, Hassn A (2012) Nurse-led telephone follow-up after day case surgery. J Nurse Pract 8:E7–E8
Bailey J, Roland M, Roberts C (1999) Is follow up by specialists routinely needed after elective surgery? A controlled trial. J Epidemiol Community Health 53:118–124
van Boxel GI, Hart M, Kiszely A et al (2013) Elective day-case laparoscopic cholecystectomy: a formal assessment of the need for outpatient follow-up. Ann R Coll Surg Engl 95:561–564
Jones TR, Khout H, Bryant D et al (2007) Rapid response: follow-up after laparoscopic cholecystectomy. BMJ 335:295
National Information Board (2015) Policy paper: delivering the five year forward view. https://www.gov.uk/government/publications/implementing-personalised-health-and-care-2020/delivering-the-five-year-forward-view. Accessed 6 Mar 2022
NHS England (2017) Integrating care locally. https://www.england.nhs.uk/five-year-forward-view/next-steps-on-the-nhs-five-year-forward-view/integrating-care-locally/. Accessed 6 Mar 2022
von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Griffiths EA, Hodson J, Vohra RS et al (2019) Utilisation of an operative difficulty grading scale for laparoscopic cholecystectomy. Surg Endosc 33:110–121
Sandblom G, Videhult P, Crona Guterstam Y et al (2015) Mortality after a cholecystectomy: a population-based study. HPB (Oxford) 17:239–243
Attili AF, Carulli N, Roda E et al (1995) Epidemiology of gallstone disease in Italy: prevalence data of the Multicenter Italian Study on Cholelithiasis (M.I.COL.). Am J Epidemiol 141:158–165
Department of Health (2019) The NHS long term plan. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan-june-2019.pdf. Accessed 6 Mar 2022
Fullfact (2019) Spending on the NHS in England. https://fullfact.org/health/spending-english-nhs/. Accessed 6 Mar 2022
Funding
This work was supported by the Medical Research Council [Grant Number MR/K00414X/1]; and Arthritis Research UK [Grant Number 19891]. Prita Daliya was a recipient of a Research Fellowship funded by the Royal College of Surgeons of England and EIDO Healthcare Limited.
Author information
Authors and Affiliations
Contributions
Study design was contributed by PD, JC, JR, DNL, and SLP. Data collection was contributed by PD, JC, and JR. Data analysis was contributed by PD. Data interpretation was contributed by PD, JC, JR, DNL, and SLP. Writing of manuscript was contributed by PD, DNL, and SLP. Critical review was contributed by PD, JC, JR, DNL, and SLP. Final approval of submitted manuscript was contributed by PD, JC, JR, DNL, and SLP.
Corresponding author
Ethics declarations
Conflict of interest
Simon L Parsons is a company director for EIDO Healthcare Limited. None of the other authors has a conflict of interest to declare.
Data sharing
Data will be available upon reasonable request from Prita Daliya (prita.daliya@doctors.org.uk).
Ethical statement
The study proposal was appraised by the confidentiality advisory group: 16/CAG/0045, with public and patient involvement, and research ethics committee application: 16/SW/0088. It was registered with ClinicalTrials.gov: NCT02810860, and NUH research and innovation: 15GS002.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An abstract of this paper was presented to the 2021 Annual Virtual Conference of the Association of Surgeons of Great Britain and Ireland. The conference abstract has been published in the British Journal of Surgery, 2021, Volume 108 (Supplement_7), znab310.001, https://doi.org/10.1093/bjs/znab310.001.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Daliya, P., Carvell, J., Rozentals, J. et al. Digital Follow-Up After Elective Laparoscopic Cholecystectomy: A Feasibility Study. World J Surg 46, 2648–2658 (2022). https://doi.org/10.1007/s00268-022-06684-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06684-w