Abstract
Background
The COVID-19 pandemic has brought many challenges including barriers to delivering high-quality surgical care and follow-up while minimizing the risk of infection. Telehealth has been increasingly utilized for post-operative visits, yet little data exists to guide surgeons in its use. We sought to determine safety and efficacy of telehealth follow-up in patients undergoing cholecystectomy during the global pandemic at a VA Medical Center (VAMC).
Methods
This was a retrospective review of patients undergoing cholecystectomy at a level 1A VAMC over a 2-year period from August 2019 to August 2021. Baseline demographics, post-operative complications, readmissions, emergency department (ED) visits and need for additional procedures were reviewed. Patients who experienced a complication prior to discharge, underwent a concomitant procedure, had non-absorbable skin closure, had new diagnosis of malignancy or were discharged home with drain(s) were ineligible for telehealth follow-up and excluded.
Results
Over the study period, 179 patients underwent cholecystectomy; 30 (17%) were excluded as above. 20 (13%) missed their follow-up, 52 (35%) were seen via telehealth and 77 (52%) followed-up in person. There was no difference between the two groups regarding baseline demographics or intra-operative variables. There was no significant difference in post-operative complications [4 (8%) vs 6 (8%), p > 0.99], ED utilization [5 (10%) vs 7 (9%), p = 0.78], 30-day readmission [3 (6%) vs 6 (8%), p = 0.74] or need for additional procedures [2 (4%) vs 4 (5%), p = 0.41] between telehealth and in-person follow-up.
Conclusion
Telehealth follow-up after cholecystectomy is safe and effective in Veterans. There were no differences in outcomes between patients that followed up in-person vs those that were seen via phone or video. Routine telehealth follow-up after uncomplicated cholecystectomy should be considered for all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The COVID-19 pandemic brought many new challenges to our health care system. On the forefront is delivering high quality healthcare while minimizing the risk of infection with the SARS-CoV-2 virus (COVID-19). While COVID-19 affects all age groups, there continues to be a disproportionate risk of morbidity and mortality in ages 65 years and older and those with an underlying medical condition [1, 2]. This predisposes the Veteran population of 19 million in the United States (US) to potentially worse outcomes as 50% are older than 65 years compared to 18.5% of civilians [3]. Veterans are also 14 times more likely to have five or more medical conditions than the general population and 14.7 times more likely to have a reported poor health status compared to the general population [4]. Thus, it was critical to find ways to protect this vulnerable population during the COVID-19 pandemic while continuing to provide access to surgery and surgical specialists. This brought about a rise in utilization of telehealth, defined in this study to include phone- or video-based medical care. Utilization of telehealth within the Veteran Affairs (VA) system rapidly increased during the pandemic with many specialties nearly doubling or tripling phone and video visits [5].
Outside the VA, the pandemic also caused a substantial increase in telehealth utilization. According to Medicare data, there was a 23-fold increase in telehealth visits between the first and second quarters of 2020 [6]. Data from over 30 healthcare organizations, located in all US states, reported telehealth accounting for 69% of all ambulatory visits during April 2020 [7]. This was driven mostly by non-surgical specialties: psychiatry (56.8% of visits via telehealth), gastroenterology (54.5%), endocrinology (53.1%), and neurology (47.9%) [6]. Comparatively, general surgery and surgical specialties lagged in the use of telehealth. Prior to the COVID-19 pandemic, general surgery utilization of telehealth was reported to be 9.7% (based on survey data) [8]. Taking into account a telehealth conversion rate of 7.5% for general surgery, surgery utilization of telehealth continues to be less than other specialties even during the pandemic [9].
The hesitation in the use of telehealth for initial surgical evaluation is likely related to the need to physically examine patients and determine the appropriate surgical approach. However, post-operative follow-up of low-risk patients presents a unique group that may best be served by telemedicine. This has been demonstrated in several, small, published studies. Hwa et al. started a physician assistant led post-operative clinic for ambulatory, elective surgery patients who had undergone either an open hernia repair or laparoscopic cholecystectomy [10]. They followed 110 patients who were seen via telehealth after surgery and identified no complications in the cholecystectomy group. Carlock et al. looked at low risk inpatients (age less than 60 years old, hospital stay less than 2 days, absence of drains on discharge, and pathology without evidence of malignancy) and their complication rates after surgery with telephone follow-up alone. This study found that just 3% of patients had complications (including abdominal pain and abdominal abscess) that were missed in telephone follow-up and required hospital readmission for their management [11].
These series of small studies suggest that telehealth follow-up after surgery can be safe and effective in certain populations. The purpose of our study is to compare morbidity, mortality, readmission and Emergency Department (ED) utilization in patients who followed up via phone- or video versus face-to-face visits after laparoscopic cholecystectomy. Our hypothesis is that telehealth follow-up after laparoscopic cholecystectomy is safe and effective in appropriately selected Veterans.
Methods
Patient selection
This study was approved by the Colorado Multi-Institutional Review Board (COMIRB) #220962. We conducted a retrospective chart review of all patients who underwent cholecystectomy during the study period, August 2019 to August 2021, at the Rocky Mountain Regional VA Medical Center in Aurora, Colorado. The Rocky Mountain Regional VA Medical Center is part of Veterans Integrated Service Network (VISN) 19. Patients were identified via CPT code as transcribed by the operating room nurse upon the completion of the surgery in the electronic record. The CPT codes included in this study were laparoscopic cholecystectomy (47562), laparoscopic cholecystectomy with cholangiography (47563), laparoscopic cholecystectomy with exploration of common bile duct (47564), cholecystectomy (47600) and cholecystectomy with exploration of common bile duct (47610).
Patient characteristics
Patients were separated into cohorts based on method of postoperative follow-up, telehealth (phone based follow-up) versus in-person based upon note title and the presence/absence of a physical exam to reduce the risk of error from incorrect note titles. Baseline demographics and service-connectedness were recorded. Patient address was used to determine census tract of residence using geocoding and estimate patient social vulnerability as indicated by the Social Vulnerability Index, which is a composite measure based on the United States’ census. Geocoding was performed in R statistical software (Vienna, Austria) [12,13,14,15].
Exclusion criteria
All patients were offered a phone telehealth appointment for follow-up unless they met one of the following exclusion criteria: (1) patient required removal of non-absorbable sutures or wound closure device, (2) required re-operation during the index admission, (3) cholecystectomy as concomitant procedure, (4) intraoperative complications, (5) were discharged with drain in place, (6) or were diagnosed with a new malignancy. Patients were considered lost to follow-up if there was no follow-up within 3 months with the surgical team.
Outcomes measures
Outcomes of interest include the primary outcome of any complication (morbidity) within 30 days of surgery as defined by the VA Surgical Quality Improvement Program (VASQIP) [16]. Secondary outcome measures include death of any cause within 30 days, readmission to inpatient status within 30 days, utilization of the ED within 30 days and the need for additional procedures.
Statistical analysis
Comparison of patient and surgery characteristics between the two groups utilized t-tests for continuous variables and Chi-squared tests (Fisher’s exact tests when applicable) of association for categorical variables. P-values < 0.05 were considered statistically significant. All statistical analyses were performed with GraphPad Prism software.
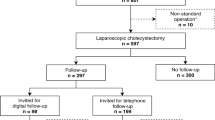
Results
During the 2-year study period, 179 patients (mean age 57 range 22–88, male gender 144 patients, 80%) underwent cholecystectomy as determined by CPT codes; 30 (17%) patients were excluded as per the exclusion criteria (Fig. 1). The majority of excluded patients had had an additional procedure at the time of cholecystectomy such as pancreaticoduodenectomy, Nissen fundoplication, colectomy, etc., (10, 33%); or had an intraoperative drain present on discharge (10, 33%). Twenty (13%) patients did not have a follow-up appointment with the surgical team although seven (5%) were seen either in-person or via phone by non-surgical Providers and were without complications. Fifty-two (35%) patients were seen via telehealth and 77 (52%) patients followed-up in person. All telehealth visits occurred via telephone.
Patient demographics
Patient demographics are available in Table 1. There was no significant difference in baseline demographics (age, race/ethnicity, sex, BMI, CCI, SVI, service connection) between telehealth and in-person follow-up. groups. Excluded patients were older (67 vs 58 vs 56.5) and had more co-morbidities (CCI 3.36) than included patients (CCI 2.11, p = 0.006). Distance from the VAMC was grouped into close (less than 50 miles) and far (50 miles or further). Seventy-two (56%) patients lived less than 50 miles from VAMC, and 57 (44%) patients lived 50 miles or further from VAMC. There was no significant difference in distance to the VAMC for patients who followed up by telehealth vs in-person, p = 0.21 (Table 1).
Operative factors
The majority of cholecystectomies were elective; 84 (65%) patients underwent a planned procedure with 45 (35%) patients undergoing urgent surgery after presentation to ED. American Society of Anesthesiologists (ASA) classification used to measure patients’ pre-anesthesia medical co-morbidities and there was no significant difference in ASA classification between patients in either group, p = 0.90 (Table 1). No patients were converted to open in the telehealth group and 5 patients were converted to open in the in-person follow-up group, p = 0.09. The remaining intraoperative factors are summarized in Table 1.
Post-operative outcomes
Fifteen (12%) patients had visits to ED (not requiring readmission) within 30 days of surgery for a surgery-related concern. There was no significant difference between ED visits for telehealth vs in-person follow-up, (10% vs 9%, p = 0.78) (Table 2). Thirty-day readmissions were required in 9 patients with no significant difference between the groups, p = 0.74 (Table 2).
Ten (8%) patients had a complication not requiring re-operation. Postoperative complications included three (2%) cardiopulmonary complications (pneumonia, pulmonary embolism and atrial fibrillation), and 5 (4%) infectious complications: 2 superficial, 1 deep and 2 organ/space infections. One (1%) bile leak occurred. One (1%) patient required a post-operative blood transfusion but no re-operation. Overall, there was no significant difference in complications between telehealth and in-person groups, p > 0.99 (Table 2).
There were 6 required additional procedures. Two re-operations occurred, both in patients in the in-person follow-up group. Reoperations were for internal hernia with small bowel obstruction on postoperative day 20 (diagnostic laparoscopy with lysis of adhesions) and an incarcerated incisional hernia (diagnostic laparoscopy with conversion to open, repair of enterotomy) on postoperative day 5. Endoscopic retrograde cholangiopancreatography (ERCP) was performed in 2 patients for retained stones. Additionally, there were 2 bedside incision and drainage/reopening of incision for superficial wound infections, this occurred in the in-person follow-up group. There was no significant difference in need for additional procedures between the groups, p = 0.41 (Table 2).
Discussion
Telehealth for routine post-operative follow-up after uncomplicated laparoscopic cholecystectomy is safe and effective in Veterans. Video- and phone-based surgical telehealth has been in place and offered at this tertiary VAMC prior to the COVID-19 pandemic; however, its use has increased significantly since the beginning of the pandemic. This follows national trends and is especially relevant as we transition into ‘life with COVID-19.’ We determined telehealth was safe as the patients who followed up via telehealth did not have an increased rate of complications, ED visits, 30-day readmissions or additional procedures (Fig. 2).
Telehealth is of particular benefit to the Veterans within large, rural areas such as VA Integrated Services Network (VISN) 19. This, the largest VA region, covers over 540,000 square miles across 10 states [17]. It is offered via standard phone call or VA Voice Connect (VVC) where the Veteran can download an app on their computer or phone in order to provide both voice and video conferencing with their physician.
When comparing overall follow-up practices in the United States to Europe, there are significant differences. In Europe, patients are not routinely scheduled for in-person follow-up after outpatient surgery. While there are several variations, the most common practice is a follow-up phone call on the first postoperative day followed by as needed phone or in-person visits thereafter [18]. In contrast, patients in the US are scheduled for follow-up 2–4 weeks after surgery. All follow-up visits, unless the patient returns to the operating room, are included in a single, global 90-day payment which may encourage more post-operative follow-up (as there is no additional cost to the patient) [19]. The European approach, however, is not without issue and some patients report difficulty in contacting Providers which can give them a sense of abandonment [18]. Routine telehealth follow-up presents a middle-ground approach that may be of benefit to European and American surgeons.
An unanticipated finding of our study was confirmation of the delay/deferral of medical care in high-risk patients during the COVID-19 pandemic. The average age of a Veteran in the United States is 65 years [20] which is older than the mean age of our included patient population is (58 and 56.5 years in our telehealth and in-person groups, respectively). This may reflect the hesitancy of patients who are older, frail and those with multiple co-morbidities to visit the hospital during the pandemic [21]. However, this may also signify generational differences in comfort with in-person vs. electronic-based follow-up. Chao et al. found that patients utilizing telehealth during the pandemic were significantly younger than their in-person counterparts, 46.8 years old (34.1–58.4) compared with 52.6 years old (38.3–62.3) (p < 0.001) [9]. More study is needed to define the barriers, technologic or otherwise, to routine telehealth follow-up as its safety is demonstrated by our study and a number of other groups.
Hwa et al. included 19 patients who underwent cholecystectomy and had telehealth post operative follow up [10] with no patients suffering complications. A study by Carlock et al. grouped several procedures: laparoscopic appendectomy, laparoscopic cholecystectomy, umbilical hernia repair, and inguinal hernia repair in low risk patients (age less than 60 years, hospital stay less than 2 days, absence of drains on discharge, and pathology without evidence of malignancy). The cholecystectomy patients had a median age 39 and median ASA class 2 (no ASA class 3 or 4 patients were included) for the patients who underwent cholecystectomy [11]. The complication rate for cholecystectomies only in these studies reported as 0% [10] and 8% [11], confirming that telehealth was safe in their study populations.
There are two main limitations in this study. First, while all surgeons were instructed to offer telehealth to all patients after uncomplicated cholecystectomy—there is no way to confirm that this occurred instead of offering telehealth to a specific subset of patients. Even had the surgeons offered telehealth only to those they thought would do well, both groups had similar rates of complications thus demonstrating safety regardless of selection bias.
The second limitation is our small study size. To the best of our knowledge, it is the largest study of post-operative cholecystectomy patients but given that tens of thousands of patients undergo cholecystectomy annually, it represents far less than 1% of current cases. In addition, there were 20 patients lost to postoperative follow-up reflecting 13% of included patients. In reality, just 13 patients (8%) were lost to follow-up with respect to complications as 5 patients were seen by non-surgical Providers (and doing well) and 2 patients called in to cancel their follow-up as they were also doing well. This rate is similar to a recent, large systematic review by Robinson et al. who encountered a 0.0–10.7% rate in surgical clinical trials from 2008 to 2020. [22]
The patients offered telehealth follow-up in our study would be traditionally considered low-risk as our exclusion criteria included all patients who had suffered intra-operative complications, required drain placement or had concomitant procedures performed. This criteria could be used to select future patients who would be appropriate for telehealth-only follow-up. This would be of great benefit to patients who had traveled great distances for their surgery, and especially beneficial to those patients in the 10-state region of VISN 19. Additionally, while a malignancy diagnosis requires extensive patient counseling, this conversation does not have to occur in person and this exclusion criteria could be modified in some patients. Future studies are warranted to include other procedures such as appendectomy, inguinal hernia repair and other sub-specialty surgery where the risk of complications are low and patients are compliant. With the development of video-based follow-up, such as the VA’s Video Connect software, this may become a more viable option for more complex patients who have concerns about their wounds and recovery.
In conclusion, telehealth follow-up after cholecystectomy is safe and effective in Veterans. There was no difference in post-operative complications, ED visits, 30-day readmission or the need for additional procedures between patients that followed up in-person vs. those that were evaluated via phone within 3 months of their procedure. Thus, we would recommend routine telehealth follow-up for all patients after uncomplicated cholecystectomy.
References
Garg S et al (2020) Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep 69(15):458–464
Cardemil CV et al (2021) COVID-19-Related hospitalization rates and severe outcomes among veterans from 5 veterans affairs medical centers: hospital-based surveillance study. JMIR Public Health Surveill 7(1):e24502–e24502
Luo J et al (2021) Coronavirus disease 2019 in veterans receiving care at veterans health administration facilities. Ann Epidemiol 55:10–14
Agha Z et al (2000) Are patients at veterans affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med 160(21):3252–3257
Myers US et al (2021) Flattening the curve by getting ahead of it: how the VA healthcare system is leveraging telehealth to provide continued access to care for rural veterans. J Rural Health 37(1):194–196
Patel SY et al (2021) (2021) Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff 40(2):349–358
Fox BT, Sizemore JO (2020) Telehealth: fad or the future. In: Epic health research network
Kane CK, Gillis K (2018) The use of telemedicine by physicians: still the exception rather than the rule. Health Aff 37(12):1923–1930
Chao GF et al (2021) Use of telehealth by surgical specialties during the COVID-19 pandemic. JAMA Surg 156(7):620–626
Hwa K, Wren SM (2013) Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg 148(9):823–827
Carlock TC et al (2020) Telephone follow-up for emergency general surgery procedures: safety and implication for health resource use. J Am Coll Surg 230(2):228–236
Team RC (2020) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Wickham DKAH (2013) Ggmap: spatial visualization with ggplot2. R Journal 5(1):144–161
Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B (2011) A social vulnerability index for disaster management. J Homel Secur Emerg Manag 8(1):1–22
Carmichael H et al (2019) Using the social vulnerability index to examine local disparities in emergent and elective cholecystectomy. J Surg Res 243:160–164
Khuri SF et al (1998) The department of veterans affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA surgical quality improvement program. Ann Surg 228(4):491–507
VA Rocky Mountain Network (2020) About the VA rocky mountain network. Available at https://www.visn19.va.gov/about/index.asp
Dahlberg K, Jaensson M, Nilsson U (2019) “Let the patient decide”—Person-centered postoperative follow-up contacts, initiated via a phone app after day surgery: secondary analysis of a randomized controlled trial. Int J Surg 61:33–37
Centers for Medicare & Medicaid Services (2018) Global surgery booklet. Medicare learning network. Centers for Medicare & Medicaid Services, Baltimore
Vespa JE (2020) Those who served: America’s veterans from world war ii to the war on terror. American community survey report. US Census Bureau, Washington
Gavin K (2022) Pandemic disrupted many older adults’ health care plans. MHealth Lab
Robinson NB et al (2021) Characteristics of randomized clinical trials in surgery from 2008 to 2020: a systematic review. JAMA Netw Open 4(6):e2114494
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Edward L Jones is a consultant for Boston. Drs. Danielle Abbitt, Kevin Choy, Heather Carmichael, Teresa S Jones, Krzystof J Wikiel, Carlton C Barnett, John T Moore Thomas N Robinson, and Ms. Rose Castle have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was presented at the 2022 SAGES Annual Meeting in Denver, CO.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abbitt, D., Choy, K., Castle, R. et al. Telehealth follow-up after cholecystectomy is safe in veterans. Surg Endosc 37, 3201–3207 (2023). https://doi.org/10.1007/s00464-022-09501-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09501-6