Abstract
Background
A multimodal analgesia (MMA) protocol has shown the effect of postoperative pain control and reduced the postoperative opioid consumption. However, it was questionable whether MMA could replace opioid-based patient-controlled analgesia (PCA) for postoperative pain control. Therefore, this study aimed to investigate whether an MMA protocol is non-inferior to opioid-based PCA for pain management after a minimally invasive colorectal cancer surgery.
Methods
A randomized, open-label, non-inferiority clinical trial was conducted on patients undergoing laparoscopic or robotic resection of colorectal cancer. The patients were randomly assigned to either the PCA or MMA group. The MMA protocol included pregabalin, tramadol, wound infiltration, and transversus abdominis plane block. The primary outcome was the numeric rating scale (NRS) score for pain at rest 24 h postoperatively.
Results
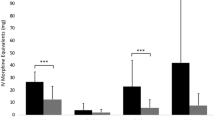
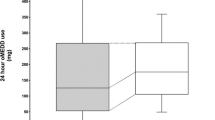
Ninety-seven patients were included in the intention-to-treat analysis. The mean difference in NRS score at rest at 24 h was 0.25 (95% confidence interval, − 0.61 to 1.11). This result demonstrated the non-inferiority of MMA to PCA in our non-inferiority margin (− 1). Compared with the PCA group, the median remifentanil dose (996 vs. 654 μg; p < 0.001) and time in the post-anesthesia care unit (35 vs. 25 min; p < 0.001) were significantly less in the MMA group.
Conclusions
Our MMA protocol successfully controlled postoperative pain and was non-inferior to morphine-based PCA based on patient-reported pain intensity, with no significant increase in adverse events. These results will help construct a strategy to reduce conventional opioid prescriptions for pain management after a minimally invasive colorectal cancer surgery.
Trial Registration Number Trial Registration Clinical Research Information Service Identifier: KCT0002593


Similar content being viewed by others
References
Echeverria-Villalobos M, Stoicea N, Todeschini AB et al (2020) Enhanced recovery after surgery (ERAS): a perspective review of postoperative pain management under ERAS pathways and its role on opioid crisis in the United States. Clin J Pain 36:219–226
Ip HY, Abrishami A, Peng PW et al (2009) Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 111:657–677
Joshi GP, Kehlet H (2019) Postoperative pain management in the era of ERAS: an overview. Best Pract Res Clin Anaesthesiol 33:259–267
Grass JA (2005) Patient-controlled analgesia. Anesth Analg 101:S44–S61
American Society of Anesthesiologists Task Force on Acute Pain Management (2012) Practice guidelines for acute pain management in the perioperative setting: an updated report by the American society of anesthesiologists task force on acute pain management. Anesthesiology 116:248–273
Oderda GM, Evans RS, Lloyd J et al (2003) Cost of opioid-related adverse drug events in surgical patients. J Pain Symptom Manag 25:276–283
Choi YY, Park JS, Park SY et al (2015) Can intravenous patient-controlled analgesia be omitted in patients undergoing laparoscopic surgery for colorectal cancer? Ann Surg Treat Res 88:86–91
Hah JM, Bateman BT, Ratliff J et al (2017) Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg 125:1733–1740
Falcone M, Luo C, Chen Y et al (2020) Risk of persistent opioid use following major surgery in matched samples of patients with and without cancer. Cancer Epidemiol Biomark Prev 29:2126–2133
Lee JS, Hu HM, Edelman AL et al (2017) New persistent opioid use among patients with cancer after curative-intent surgery. J Clin Oncol 35:4042–4049
Kehlet H, Dahl JB (1993) The value of ‘multimodal’ or ‘balanced analgesia’ in postoperative pain treatment. Anesth Analg 77:1048–1056
Schwenk ES, Mariano ER (2018) Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J Anesthesiol 71:345–352
Oh TK, Jeon YT, Choi JW (2019) Trends in chronic opioid use and association with five-year survival in South Korea: a population-based cohort study. Br J Anaesth 123:655–663
Xu YJ, Sun X, Jian H et al (2020) Randomized clinical trial of continuous transversus abdominis plane block, epidural or patient-controlled analgesia for patients undergoing laparoscopic colorectal cancer surgery. Br J Srug 107:e133–e141
Mishriky BM, Waldron NH, Habib AS (2015) Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. Br J Anaesth 114:10–31
Bamigboye AA, Hofmeyr GJ (2009) Local anaesthetic wound infiltration and abdominal nerves block during caesarean section for postoperative pain relief. Cochrane Database Syst Rev 8(3):CD006954
Kim D, Kim JK, Yeo J (2020) Translation and validation of the Korean version of the postoperative quality of recovery score QoR-15. Biomed Res Int 9(2020):3456234
Duthie DJ (1998) Remifentanil and tramadol. Br J Anaesth 81:51–57
Julious SA (2004) Sample sizes for clinical trials with normal data. Stat Med 23:1921–1986
Viscusi ER, Reynolds L, Chung F et al (2004) Patient-controlled transdermal fentanyl hydrochloride vs intravenous morphine pump for postoperative pain: a randomized controlled trial. JAMA 291:1333–1341
Pasricha SV, Tadrous M, Khuu W et al (2018) Clinical indications associated with opioid initiation for pain management in Ontario, Canada: a population-based cohort study. Pain 159:1562–1568
Clarke H, Soneji N, Ko DT et al (2014) Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ 348:g1251
Wick EC, Grant MC, Wu CL (2017) Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 152:691–697
Pedrazzani C, Menestrina N, Moro M et al (2016) Local wound infiltration plus transversus abdominis plane (TAP) block versus local wound infiltration in laparoscopic colorectal surgery and ERAS program. Surg Endosc 30:5117–5125
Yeap YL, Wolfe JW, Kroepfl E et al (2020) Transversus abdominis plane (TAP) block for laparoscopic live donor nephrectomy: continuous catheter infusion provides no additional analgesic benefit over single-injection ropivacaine. Clin Transplant 34:e13861
Niraj G, Kelkar A, Hart E et al (2015) Four quadrant transversus abdominis plane block and continuous transversus abdominis plane analgesia: a 3-year prospective audit in 124 patients. J Clin Anesth 27:579–584
Ohnuma T, Krishnamoorthy V, Ellis AR et al (2019) Association ’between gabapentinoids on the day of colorectal surgery and adverse postoperative respiratory outcomes. Ann Surg 270:e65–e67
Radbruch L, Glaeske G, Grond S et al (2013) Topical review on the abuse and misuse potential of tramadol and tilidine in Germany. Subst Abus 34:313–320
Raffa RB, Friderichs E, Reimann W et al (1992) Opioid and nonopioid components independently contribute to the mechanism of action of tramadol, an “atypical” opioid analgesic. J Pharmacol Exp Ther 260:275–285
Ma J, Wang XY, Sun QX et al (2018) Transversus abdominis plane block reduces remifentanil and propofol consumption, evaluated by closed-loop titration guided by bispectral index. Exp Ther Med 16:3897–3902
Elias KM, Stone AB, McGinigle K et al (2019) The reporting on ERAS compliance, outcomes, and elements research (RECOvER) checklist: a joint statement by the ERAS® and ERAS® USA societies. World J Surg 43:1–8. https://doi.org/10.1007/s00268-018-4753-0
Jamjittrong S, Matsuda A, Matsumoto S et al (2019) Postoperative non-steroidal anti-inflammatory drugs and anastomotic leakage after gastrointestinal anastomoses: systematic review and meta-analysis. Ann Gastroenterol Surg 4:64–75
Acknowledgements
We acknowledge the dedicated efforts of So Young Jeong, who served as a research investigator and appreciate the patients for their participation in this trial.
Author information
Authors and Affiliations
Contributions
SYP, JSP, JY contributed to the conception and design of the manuscript. SYP, JSP, JY, JKK, JO contributed to the acquisition of data. GSC, HJK were involved in the analysis and interpretation of data. SYP, JSP, JY contributed to the drafting the article. All authors contributed to the critical revision of the article for important intellectual content and the final approval of the version to be published. SYP, JSP contributed equally to this study as co-corresponding authors.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Jinseok Yeo, Jun Seok Park, Gyu-Seog Choi, Hye Jin Kim, Jay Kyoung Kim, Jinyoung Oh, and Soo Yeun Park have no conflicts of interest or financial ties to disclose.
Consent for publication
This manuscript has not been submitted for publication, nor has it been published in whole or in part elsewhere.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yeo, J., Park, J.S., Choi, GS. et al. Comparison of the Analgesic Efficacy of Opioid-Sparing Multimodal Analgesia and Morphine-Based Patient-Controlled Analgesia in Minimally Invasive Surgery for Colorectal Cancer. World J Surg 46, 1788–1795 (2022). https://doi.org/10.1007/s00268-022-06473-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06473-5