Abstract
Objective
To compare clinical, biochemical, tumoural and mutational characteristics of Von Hippel Lindau Syndrome (VHL)-associated pheochromocytoma (PCC) to multiple endocrine neoplasia 2A (MEN2A)-associated pheochromocytoma.
Design
Retrospective study design in a tertiary health care centre in Northern India.
Methods
A total of 47 patients with biochemical and histologically proven pheochromocytoma/paraganglioma (PCC/PGL): 29 associated with VHL and 18 with MEN2A, were divided in two cohorts, respectively. Analysis of their medical records along with a prospective follow-up was done.
Results
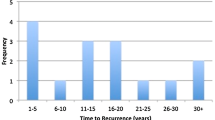
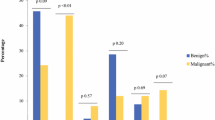
There were more children <19 years in VHL group (13 vs 1). Despite majority of VHL-PCC showing elevation of normetanephrine (NMN) (93%) as compared to MEN2A-PCC (22.2%), 75.8% presented with hypertension as compared to MEN2A (33.3%). The average size of VHL-PCC tumours was 5.66 cm. VHL-PCC as compared to MEN2A-PCC were multifocal (75% vs 61.1%), bilateral synchronous (72.4 vs 61.1%) and extra-adrenal (17.2% vs 0%). Both VHL (24%) and MEN2A-PCC (27.7%) showed multiple nodules, but more MEN2A PCC showed extra-tumoural hyperplasia (44.4% vs. 6.8%). In VHL, the commonest mutation (n = 17) was missense mutation with a hot spot on exon 3, while in MEN2A-PCC majority (66.6%) had 634 mutation in exon 11 and only 2 patients had the rare 611 mutation in exon 10.
Conclusion
In contrast to world literature, our study suggests Indian VHL-PCC can be symptomatic in spite of noradrenergic phenotype, large in size and multifocal. Multiple nodules in VHL-PCC could increase risk of recurrence following subtotal adrenalectomy.
Similar content being viewed by others
References
Pillai S, Gopalan V, Smith RA, Lam AK (2016) Updates on the genetics and the clinical impacts on phaeochromocytoma and paraganglioma in the new era. Crit Rev Oncol Hematol 1(100):190–208
Gimenez-Roqueplo AP, Dahia PL, Robledo M (2012) An update on the genetics of paraganglioma, pheochromocytoma, and associated hereditary syndromes. Horm Metab Res 44(05):328–333
Karasek, David et al. (2010) Genetic testing for pheochromocytoma. Current hypertension reports vol. 12(6):456–464. https://doi.org/10.1007/s11906-010-0151-1
Buffet A, Ben Aim L, Leboulleux S, Drui D, Vezzosi D, Libé R, Ajzenberg C, Bernardeschi D, Cariou B, Chabolle F, Chabre O (2019) Positive impact of genetic test on the management and outcome of patients with paraganglioma and/or pheochromocytoma. J Clin Endocrinol Metab 104(4):1109–1118
Neumann HP, Bausch B. McWhinney S. Rea (2002) Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med 346(19):1459–1466.
Li, Shimena R et al. (2020) Clinical and Biochemical Features of Pheochromocytoma Characteristic of Von Hippel-Lindau Syndrome. World J Surg 44(2):570–577. https://doi.org/10.1007/s00268-019-05299-y
Christina Pamporaki, Barbora Hamplova, Mirko Peitzsch, Aleksander Prejbisz, Felix Beuschlein, Henri J.L.M. Timmers, Martin Fassnacht, Barbara Klink, Maya Lodish, Constantine A. Stratakis, Angela Huebner, Stephanie Fliedner, Mercedes Robledo, Richard O. Sinnott, Andrzej Januszewicz, Karel Pacak, Graeme Eisenhofer (2017) Characteristics of Pediatric vs Adult Pheochromocytomas and Paragangliomas. J Clin Endocrinol Metabolism 102(4):1122–1132. https://doi.org/10.1210/jc.2016-3829
Petenuci J, Guimaraes AG, Fagundes GF, Benedetti AF, Afonso AC, Pereira MA, Zerbini MC, Siqueira S, Yamauchi F, Soares SC, Srougi V et al (2021) Genetic and clinical aspects of paediatric pheochromocytomas and paragangliomas. Clin Endocrinol 95(1):117–124
Eisenhofer G, Walther MM, Huynh TT, Li ST, Bornstein SR, Vortmeyer A, Mannelli M, Goldstein DS, Linehan WM, Lenders JW, Pacak K (2001) Pheochromocytomas in von Hippel-Lindau syndrome and multiple endocrine neoplasia type 2 display distinct biochemical and clinical phenotypes. J Clin Endocrinol Metab 86(5):1999–2008
Telenius-Berg M, Berg B, Hamberger B, Tibblin S (1987) Screening for early asymptomatic pheochromocytoma in MEN-2. Henry Ford Hosp Med J 35(2):110–114
Aprill BS, Drake AJ, Lasseter DH, Mohamed Shakir KM (1994 Mar 15) (1994) Silent adrenal nodules in von Hippel-Lindau disease suggest pheochromocytoma. Ann Intern Med 120(6):485–487
Pomares FJ, Canas R, Rodriguez JM, Hernandez AM, Parrilla P, Tebar FJ (1998) Differences between sporadic and multiple endocrine neoplasia type 2A phaeochromocytoma. Clin Endocrinol 48(2):195–200
Walther Mm, Reiter R, Keiser Hr, Choyke Pl, Venzon D, Hurley K, Gnarra Jr, Reynolds Jc, Glenn Gm, Zbar B, Linehan Wm (1999) Clinical and genetic characterization of pheochromocytoma in von Hippel-Lindau families: comparison with sporadic pheochromocytoma gives insight into natural history of pheochromocytoma. J Urol 162(3 Part 1):659–664.
Aufforth RD, Ramakant P, Sadowski SM, Mehta A, Trebska-McGowan K, Nilubol N, Pacak K, Kebebew E (2015) Pheochromocytoma screening initiation and frequency in von Hippel-Lindau syndrome. J Clin Endocrinol Metab 100(12):4498–4504
Eisenhofer G, Lenders JW, Linehan WM, Walther MM, Goldstein DS, Keiser HR (1999) Plasma normetanephrine and metanephrine for detecting pheochromocytoma in von Hippel-Lindau disease and multiple endocrine neoplasia type 2. N Engl J Med 340(24):1872–1879
Richard S, Beigelman C, Duclos JM, Fendler JP, Plauchu H, Plouin PF, Schlumberger M, Vermesse B, Proye C.(1994) Pheochromocytoma as the first manifestation of von Hippel-Lindau disease. Surgery 116(6):1076–1081.
Neumann H, Berger DP, Sigmund G, Blum U, Schmidt D, Parmer RJ, Volk B, Kirste G (1993) Pheochromocytomas, multiple endocrine neoplasia type 2, and von Hippel-Lindau disease. New England J Med 329(21):1531–1538.
Koch CA, Mauro D, Walther MM, Linehan WM, Vortmeyer AO, Jaffe R, Pacak K, Chrousos GP, Zhuang Z, Lubensky IA (2002) Pheochromocytoma in von Hippel-Lindau disease: distinct histopathologic phenotype compared to pheochromocytoma in multiple endocrine neoplasia type 2. Endocr Pathol 13(1):17–27
Nordstrom‐O'Brien M, van der Luijt RB, van Rooijen E, van den Ouweland AM, Majoor‐Krakauer DF, Lolkema MP, van Brussel A, Voest EE, Giles RH (2010)Genetic analysis of von Hippel‐Lindau disease. Human Mutation 31(5):521–537.
Lomte N, Kumar S, Sarathi V, Pandit R, Goroshi M, Jadhav S, Lila AR, Bandgar T, Shah NS (2018) Genotype phenotype correlation in Asian Indian von Hippel-Lindau (VHL) syndrome patients with pheochromocytoma/paraganglioma. Fam Cancer 17(3):441–449
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to be declared by any author.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dhanda, M., Agarwal, A., Mandal, K. et al. Clinical, Biochemical, Tumoural and Mutation Profile of VHL- and MEN2A-Associated Pheochromocytoma: A Comparative Study. World J Surg 46, 591–599 (2022). https://doi.org/10.1007/s00268-021-06393-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06393-w