Abstract
Background
The aim of this study was to investigate which histopathologic findings are most indicative for necrotizing soft tissue infections (NSTIs) in ambivalent cases.
Methods
Patients undergoing surgical exploration for suspected NSTIs with obtainment of incisional biopsies for histopathological assessment were included from January 2013 until August 2019. The frozen sections and formalin-fixed paraffin-embedded (FFPE) samples were retrospectively re-assessed. The primary outcome was the discharge diagnosis.
Results
Twenty-seven (69%) biopsies of the 39 included samples were from patients with NSTIs. Microscopic bullae (p = 0.043), severe fascial inflammation (p < 0.001) and fascial necrosis (p < 0.001) were significantly more often present in the NSTI group compared to the non-NSTI group. Muscle edema (n = 5), severe muscle inflammation (n = 5), muscle necrosis (n = 8), thrombosis (n = 10) and vasculitis (n = 5) were most frequently only seen in the NSTI group. In thirteen tissues samples, there were some discrepancies between the severity of findings in the frozen section and the FFPE samples. None of these discrepancies resulted in a different diagnosis or treatment strategy.
Conclusion
Microscopic bullae, severe fascial or muscle inflammation, fascial or muscle necrosis, muscle edema, thrombosis and vasculitis upon histopathological evaluation all indicate a high probability of a NSTI. At our institution, diagnosing NSTIs is aided by using intra-operative frozen section as part of triple diagnostics in ambivalent cases. Based on the relation between histopathologic findings and final presence of NSTI, we recommend frozen section for diagnosing NSTIs in ambivalent cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early diagnosis and immediate radical surgical treatment are vital for reducing the mortality rate of necrotizing soft tissue infections (NSTIs) [1,2,3]. NSTIs are notorious for being difficult to diagnose based on clinical symptoms, resulting in high rates of misdiagnosis and treatment delay [4, 5]. To resolve this problem, the approach using triple diagnostics (diagnosis based on macroscopic, histopathologic and microbiologic findings) has been proposed for ambivalent macroscopic cases [6]. The intra-operative evaluation of frozen sections and Gram stains enables identification of microscopic signs of NSTIs [6]. The use of triple diagnostics demonstrated a relatively low mortality rate and shorter intensive care stays, indicating a less severe disease course, likely due to identification of the NSTI in its earlier stages when only microscopically signs are visible [7]. However, there is still no clear consensus concerning the use of frozen sections for diagnosing NSTIs [8, 9]. This is mainly caused by the lack of current literature on this topic [10,11,12,13]. Back in 1984, Stamenkovic et al. [11] first reported that frozen sections might reduce the mortality rate of NSTIs resulting from the earlier recognition of the infection. However, the first guideline recommendation for using frozen sections to diagnose NSTIs, as part of triple diagnostics, was not made until 2018 [8]. Nonetheless, this guideline also stated that frozen sections are not very practical and require availability and experience of the pathologists, while intra-operative assessment of frozen sections has already become routine practice in surgical oncology [8, 14]. Therefore, the aim of this study was to investigate which histopathologic findings are most indicative for the diagnosis NSTI.
Methods
Study design
Patients undergoing surgical exploration for suspected NSTIs with obtainment of tissue biopsies for histopathological assessment during this initial exploration at an academic hospital were prospectively identified from January 2013 until August 2019 and included in this study. Biopsies taken secondarily from patients with an already confirmed and current NSTI were excluded. The clinical outcomes of patients included up to January 2019 were previously reported in an article by Nawijn et al. [7]. NSTIs were diagnosed based on macroscopic findings of necrosis of the subcutaneous tissue, fascia or muscle during surgical exploration. In case of ambivalent macroscopic findings such as fascial edema without clear necrosis, the triple diagnostics algorithm was used. Using this algorithm, the diagnosis NSTI was confirmed if either the intra-operative assessed frozen section or Gram stain was positive. If both were negative, the diagnosis NSTI was rejected [6]. Final diagnosis was made by clinical follow-up. When triple diagnostics were utilized, the following histopathologic characteristics of NSTIs were often used for assessing tissue biopsies: necrosis of superficial fascia, polymorphonuclear infiltration of the deep dermis and fascia, fibrinous thrombi of arteries and veins passing through the fascia, angiitis with fibrinoid necrosis of vessels walls and micro-organisms within the destroyed fascia and dermis [6, 11].
Data collection and outcome measures
Data collected from the medical charts included physical examination findings, intra-operative findings (based on surgical notes), histopathologic findings (both frozen sections and standard formalin-fixed paraffin-embedded (FFPE) samples) and discharge diagnosis. The sampling process for frozen sections is detailed in Fig. 1 [6]. At our institute, all samples (frozen and FFPE) are archived for 35 years and all tissue blocks from which sections were sliced are archived for 110 years. A data-collection form was designed to retrospectively re-assess the frozen sections in a protocolized manure without knowing the conclusion given by the previous pathologist (Appendix 1). Notion was made of which tissue layers were available and if they showed any abnormalities. All samples were assessed by an experienced pathologist. The frozen section, if available, was examined prior to assessing the FFPE sample. For the assessment of the overall histopathological characteristics of NSTIs, the most atypical finding from either the frozen section or FFPE sample was recorded. The primary outcome of this study was the discharge diagnosis reported in the discharge papers.
Statistical analyses
Categorical variables are presented as fractions or frequencies. Missing data were handled using pairwise deletion. The Fisher exact test was used for dichotomous independent variables and the Χ2 for trend for ordinal independent variables. For all analyses, a p value < 0.05 was considered statistically significant. Data were analyzed using STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP).
Results
Thirty-seven patients underwent surgical explorations during which biopsies were taken for histopathologic evaluation. Twenty-six patients were diagnosed with NSTIs (70%), of which four patients eventually died (15%). One patient had initially a negative exploration; however, due to clinically deterioration triple diagnostics were repeated two days later and were positive for NSTI. Another patient underwent a new exploration three months after hospitalization for an earlier NSTI, which was eventually negative (diagnosis: erysipelas). From both patients, the histopathologic samples were included, resulting in a total of 39 biopsies from 37 patients (Fig. 2). Eight biopsies were truly full-thickness biopsies (epidermis to muscle). The epidermis and dermis were both most commonly missing (both in 22 samples) (Fig. 3).
Histopathologic characteristics of NSTIs
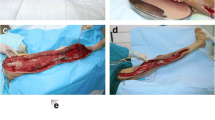
Bullae (p = 0.043), more severe fascial inflammation (p < 0.001), especially if rated as severe inflammation (p < 0.001) and fascial necrosis (p < 0.001) were significantly more often present in the NSTI group compared to the non-NSTI group (Table 1; Figs. 4, 5, 6). There were two NSTI patients without microscopic fascial necrosis; however, both had reported macroscopic fascial necrosis. Microscopic muscle edema (n = 5), severe muscle inflammation (n = 5), muscle necrosis (n = 8), thrombosis (n = 10) or vasculitis (n = 5) were in a minority of the cases found; however if present, it was in all but two case only found in NSTI patients (Fig. 7a).
Microscopic views of different histopathologic findings in necrotizing soft tissue infections. a Necrotic subcutaneous fat; b inflammation of subcutaneous fat and muscle tissue, combined with necrosis of the subcutaneous fat; c micro-thrombi; d necrotic and intact subcutaneous fat combined with vasculitis
Histopathological findings of necrotizing soft tissue infection (NSTI) found in biopsies from patients undergoing surgical exploration for suspected NSTI. a Positive histopathological findings. b Negative histopathological findings Figure legend: Dark blue inner circle represents all 27 NSTI patients; white numbers report the number of NSTI patients with a certain (in case of b: absent) histopathological findings (written in black); light blue outer circle represents all 12 non-NSTI patients; black numbers report the number of non-NSTI patients with a certain (in case of b: absent) histopathological findings (written in black)
Histopathologic characteristics of non-NSTIs
Twelve biopsies were from patients with eventually a non-NSTI discharge diagnosis. Severe fascial inflammation (n = 12), vasculitis (n = 12), thrombosis (n = 11) and fascial necrosis (n = 10) were absent in all or a majority of the cases (Fig. 7b). If histopathological abnormalities were found, this was most often either edema in the dermis (5/6), subcutaneous fat inflammation (7/11) or fascial edema (8/12) (Table 7, Appendix 2). These patients had as discharge diagnosis either cellulitis (n = 5), erysipelas (n = 5), bacteremia with septic embolisms caused by an endocarditis (n = 1) or an adverse drug reaction (ADR) with cutaneous eosinophilia (n = 1). One of the two non-NSTI patients with fascial necrosis also had microscopic thrombi (diagnosis: ADR with cutaneous eosinophilia). The thrombi and fascial necrosis were most likely secondary to the patient’s systemic (micro)vascular disease, which also explained the secondary influx of neutrophils. In the other patient with microscopic fascial necrosis (diagnosis: cellulitis), the necrosis was found during re-assessment of the biopsies for this study and was not reported by the pathologist that originally assessed the biopsy. This pathologist concluded ambivalent signs of a NSTI in the frozen section. Combined with a negative Gram stain and macroscopic vital fascia, the diagnosis NSTI was found unlikely and no debridement was performed. This patient did not clinically deteriorate after the exploration, however developed an abscess at the same location a week later. In retrospect, it is hypothesized that early abscess formation might have caused the necrosis seen microscopically.
Discrepancies
Thirty-four biopsies were first processed as frozen section followed by processing as FFPE sample. The five other samples were only processed as FFPE samples. In eleven samples (out of 34), one or more tissue layers were missing in the frozen section compared to the FFPE sample. Most often, the subcutaneous fat tissue was missing in the frozen section but present in the FFPE sample (n = 6) (Fig. 3). In thirteen samples (out of 34), there was a discrepancy between the severity of findings upon histopathological assessment of the frozen section and the FFPE samples (Table 2). However, none of these less severe findings in the frozen sections resulted in a different diagnosis or treatment strategy. In eleven of those thirteen samples, material of the FFPE sample was sliced from the same biopsy as the frozen section, and in the two other samples, the material of the sample was sliced from additionally taken tissue biopsies from which no frozen section was made.
Physical examination
The findings upon physical examination prior to surgery were reported in 38 cases. Blue or purple skin discoloration was reported in nineteen cases (15 in NSTI group). All of these fifteen NSTI cases had either microscopic necrosis of the subcutis or fascia, and in five cases, microscopic thrombi were found.
Macroscopic bullae were reported in eleven cases (9 in NSTI group). Microscopic bullae were as well seen upon histopathologic evaluation in five NSTI cases and only microscopically seen in one case (not reported upon physical examination). In the two non-NSTI cases with macroscopic bullae, the discharge diagnoses were a bacteremia caused by an endocarditis and an ADR with cutaneous eosinophilia.
Intra-operative findings
In 24 cases (out of 39), no macroscopic fascial necrosis was visible upon surgical exploration and triple diagnostics were necessary to make the diagnosis NSTI more or less likely. In 12 out of those 24 cases, microscopic necrosis of the fascia was found (Fig. 2). In five out of the twelve NSTI cases without macroscopic necrosis, fascial edema was also not explicitly reported. In total, fascial edema was explicitly reported in fourteen out of the 39 cases, of which two cases were non-NSTIs (diagnosis: both erysipelas).
Discussion
The use of intra-operative frozen section as part of the triple diagnostics algorithm in less evident macroscopic cases of NSTI has been suggested. Based on our findings, we propose major and minor histopathologic criteria for patients with suspected NSTIs (Table 3) and provide key notes for using frozen section sections (Table 4). In case of using frozen sections, pathologist should especially look for bullae, muscle edema, severe fascial or muscle inflammation, fascial or muscle necrosis and vascular abnormalities (e.g. thrombosis or vasculitis). The major criteria are the significant findings from this study; the minor criteria are findings that were distinctly seen in patients with NSTIs. These findings are in our opinion beneficial for recognizing NSTIs in frozen sections and should be the focus of larger studies with sufficient power.
The histopathological criteria regarding the fascia found in this study are comparable with prior studies (Table 5) [10, 13]. Although microscopic fascial necrosis was found to be a predictive finding for NSTIs in this current study and the study by Solomon et al. [13], two patients in our study had no microscopic fascial necrosis. In both cases, macroscopic fascial necrosis was reported in the operative report, resulting in hypothesis that these biopsies might have been taken from the resection margin (not well documented), and therefore, necrotic tissue was absent in the biopsy. Thus, it is important for surgeons to report the location from which area, in relation to the infection, the biopsy was taken. Furthermore, this shows that only looking for (microscopic) fascial necrosis does not result in 100% sensitivity, and therefore, biopsies should be assessed for other, additional, histopathologic findings. Considering that histopathological findings in the fascia as well as in the epidermis and muscle were predictive, obtaining full-thickness biopsies is strongly recommended. Unfortunately, only 21% of the biopsies in this study were full-thickness biopsies, so awareness among surgeons to obtain full-thickness biopsies (epidermis to muscle) should increase [6, 10, 11]. This is in contrast to samples for Gram-staining and culture, which preferable only contains clean handled fascia [7]. This is the first study differentiating the histopathological findings by tissue layer for NSTIs [10, 13].
Even if multiple tissue layers are biopsied, there is still a risk of losing tissue layers during processing of frozen sections. In 32% of the biopsies, tissue layers were absent in the frozen section compared to the FFPE sample, which was most often the subcutaneous fat. This is commonly caused by sampling errors; fat needs lower temperature to freeze compared to most other tissues, but when fat is overfreezed, it shatters more easily. Furthermore, fatty tissues are known to be more difficult to cut which can cause artifacts [15, 16]. Due to the instability of subcutaneous fat in frozen sections, subcutaneous fat findings were not included in our criteria.
In 38% of the biopsies, there were histopathological discrepancies between the frozen section and the FFPE sample. The signs of NSTIs appeared to be less outspoken in the frozen section (e.g. less severe inflammation, absent thrombi). The discrepancies in this study were most commonly due to the assessment of more superficial slices from the incisional biopsy for the frozen section and not due to sampling errors or artifacts. Even though discrepancies between frozen sections and FFPE samples were common and could result in underestimation of certain histopathologic characteristics, the diagnosis made and corresponding treatment strategy based on the frozen sections did not change after assessment of the FFPE sample. This is in line with studies from other medical fields using frozen sections, which report low rates of discordance between the frozen section conclusion and final diagnosis [14, 17, 18].
Histopathologic assessment is beneficial for diagnosing NSTIs, since clinical symptoms are not seldom unreliable [4, 5, 19]. A prior study showed that macroscopic fascial necrosis during surgical exploration has a high positive predictive value, but a low negative predictive value and therefore cannot simply rule out NSTIs [7]. Especially patients without evident macroscopic fascial necrosis benefit from using frozen sections, since half of the patients with NSTIs in this study did not have any signs of macroscopic fascial necrosis, while microscopic necrosis was (already) present. Also, patients with a high clinical suspicion for NSTI but with eventually a non-NSTI benefited from the frozen section, since ruling out microscopic necrosis in case of per-operative fascial edema averted unnecessary debridement. However, there were two patients with non-NSTIs and microscopic fascial necrosis in this study. A NSTI was eventually very unlikely in both cases based on the macroscopic evaluation, a negative Gram stain and the whole histological image. In these patients, it can be argued if a frozen section should have been taken in the first place, since the fascia was vital and no dishwater fluid or edema (which was present in all other ambivalent cases) was found upon macroscopic assessment. This stresses using frozen sections as part of the triple diagnostics algorithm and not as independent test. Using frozen sections in combination with other tests increases the reliability of the diagnosis made, especially in ambivalent cases.
Imaging, such as plain radiographs or computed tomography (CT), has also been proposed for diagnosing (ambivalent) NSTIs; however, it is not part of the diagnostic work-up at our institute and remains controversial in the current literature [8]. The use of CT-scans might be beneficial for certain patients, such as patients with a suspected intra-abdominal source of the infection [20]. A few studies have evaluated the diagnostic value of CT scans, all reporting high specificity, but widely variable sensitivity results [21,22,23]. Martinez et al. [22] proposed diagnosing NSTIs by assessing CT-scans using four criteria, resulting in a sensitivity of 100% and specificity of 98%. On the other hand, McGillicuddy et al. reported a sensitivity of 43% for diagnosing NSTI based on fascial air (specificity 98%) and a sensitivity of 39% for diagnosing NSTIs based on fluid tracking on CT-scans (specificity 85%), both criteria (with low sensitivity in the literature) were used in the criteria by Martinez et al. [22, 23]. Furthermore, CT scans cannot be performed in hemodynamically unstable patients (which is upon presentation frequent the case in NSTI patients) and could cause a significant delay in the surgical treatment of NSTIs [24, 25].
This study is limited by its small sample size, which constrained us to a descriptive analysis. One of the biggest arguments made against using frozen sections for diagnosing NSTIs is that it requires a pathologists with frozen section expertise [8]. Fortunately, we had the benefit of an experience pathologist who specializes in skin and soft tissues to re-assess all samples. With our protocolled assessment, we aimed to simplify the assessment, maintain generalizability and applicability of our results, and provide some sort of quantitative assessment of the samples and thus recommendations. During the retrospective scoring and assessment of the samples by the pathologist, the conclusion made did not differ from the conclusion reported in the first pathology report. The retrospective assessment only resulted in more details. We acknowledge that the implementation of frozen sections for diagnosing NSTI is affected by a hospital resources and regional collaborations, which requires the appropriate logistics for assessing frozen sections in emergency setting.
Conclusion
The presence of bullae, severe fascial or muscle inflammation, fascial or muscle necrosis, muscle edema, thrombosis or vasculitis upon histopathological evaluation all indicate a high probability of a NSTI. In more than half of all surgical explorations for NSTIs, frozen sections aided in making the diagnosis NSTI more or less likely. Even though discrepancies between frozen and FFPE samples were common, none of the diagnoses made based on the frozen section had to be revised after examination of the FFPE samples. Therefore, we recommend frozen section for diagnosing NSTIs in ambivalent cases as part of the triple diagnostics algorithm.
Abbreviations
- AUC:
-
Area under the curve
- ADR:
-
Adverse drug reaction
- FFPE:
-
Formalin-fixed paraffin-embedded
- NSTI:
-
Necrotizing soft tissue infection
- ROC:
-
Receiver operative characteristics
References
Gelbard RB, Ferrada P, Yeh DD, Williams BH, Loor M, Yon J et al (2018) Optimal timing of initial debridement for necrotizing soft tissue infection: a practice management guideline from the eastern association for the surgery of trauma. J Trauma Acute Care Surg 85(1):208–214
Nawijn F, Smeeing D, Houwert R, Leenen L, Hietbrink F (2020) Time is of the essence when treating necrotizing soft tissue infections: a systematic review and meta-analysis. World J Emerg Surg 15(1):4
Stevens DL, Bryant AE (2017) Necrotizing soft-tissue infections. N Engl J Med 377(23):2253–2265
Goh T, Goh L, Ang C, Wong C (2014) Early diagnosis of necrotizing fasciitis. Br J Surg 101:e119–e125
Wong C-H, Chang H-C, Pasupathy S, Khin L-W, Tan J-L, Low C-O (2003) Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am 85(8):1454–1460
Hietbrink F, Bode LG, Riddez L, Leenen LPH, van Dijk MR (2016) Triple diagnostics for early detection of ambivalent necrotizing fasciitis. World J Emerg Surg 11(1):1–7
Nawijn F, Houwert RM, van Wessem KPJ, Simmermacher RKJ, Govaert GAM, van Dijk MR et al (2019) A 5-Year evaluation of the implementation of triple diagnostics for early detection of severe necrotizing soft tissue disease: a single-center cohort study. World J Surg 43(8):1898–1905
Sartelli M, Guirao X, Hardcastle TC, Kluger Y, Boermeester MA, Raşa K et al (2018) 2018 WSES/SIS-E consensus conference: recommendations for the management of skin and soft-tissue infections. World J Emerg Surg 13:58
Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJD et al (2005) Infectious Diseases Society of America: practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis 41(10):1373–1406
Stegeman SA, Nijhuis I, Van Leeuwen AM, Bonsing BA, Steenvoorde P (2012) The value of frozen section biopsy in diagnosing necrotizing fasciitis: proposal of a new grading system. J Tissue Viability 21(1):13–16
Stamenkovic I, Lew PD (1984) Early recognition of potentially fatal necrotizing fasciitis. the use of frozen-section biopsy. N Engl J Med 310(26):1689–1693
Majeski J, Majeski E (1997) Necrotizing fasciitis: improved survival with early recognition by tissue biopsy and aggressive surgical treatment. South Med J 90(11):1065–1068
Solomon IH, Borscheid R, Laga AC, Askari R, Granter SR (2018) Frozen sections are unreliable for the diagnosis of necrotizing soft tissue infections. Mod Pathol 31(4):546–552. https://doi.org/10.1038/modpathol.2017.173
Ahmad Z, Barakzai M, Idrees R, Bhurgri Y (2008) Correlation of intra-operative frozen section consultation with the final diagnosis at a referral center in Karachi, Pakistan. Indian J Pathol Microbiol 51(4):469–473
Desciak EB, Maloney ME (2000) Artifacts in frozen section preparation. Dermatol Surg 26(5):500–504
Dey P (2018) Basic and advanced laboratory techniques in histopathology and cytology. Springer, Singapore, pp 51–55
Sams SB, Wisell JA (2017) Discordance between intraoperative consultation by frozen section and final diagnosis: a classification model to guide quality improvement. Int J Surg Pathol 25(1):41–50
Winther C, Græm N (2011) Accuracy of frozen section diagnosis: a retrospective analysis of 4785 cases. Apmis 119(4–5):259–262
Kiat H, En Natalie Y, Fatimah L (2017) Necrotizing fasciitis: how reliable are the cutaneous signs? J Emerg Trauma Shock 10(4):205
Guo K, Gong W, Zheng T, Hong Z, Wu X, Ren H et al (2019) Clinical parameters and outcomes of necrotizing soft tissue infections secondary to gastrointestinal fistulas. BMC Infect Dis 19(1):1–10
Fernando S, Tran A, Cheng W, Rochwerg B, Kyeremanteng K, Seely A et al (2019) Necrotizing soft tissue infections: diagnostic accuracy of physical examination, imaging, and LRINEC score. Ann Surg 269(1):58–65
Martinez M, Peponis T, Hage A, Yeh DD, Kaafarani HMA, Fagenholz PJ et al (2018) The role of computed tomography in the diagnosis of necrotizing soft tissue infections. World J Surg 42(1):82–87
McGillicuddy EA, Lischuk AW, Schuster KM, Kaplan LJ, Maung A, Lui FY et al (2011) Development of a computed tomography-based scoring system for necrotizing soft-tissue infections. J Trauma-Inj Infect Crit Care 70(4):894–899
Nawijn F, Smeeing DPJ, Houwert RM, Leenen LPH, Hietbrink F (2020) Time is of the essence when treating necrotizing soft tissue infections: a systematic review and meta-analysis. World J Emerg Surg 15:4
Wang DC, Parry CR, Feldman M, Tomlinson G, Sarrazin J, Glanc P (2015) Acute abdomen in the emergency department: is CT a time-limiting factor? Am J Roentgenol 205(6):1222–1229
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The institutional review board of the University Medical Center Utrecht provided a waiver for data collection (WAG/om/15/032329).
Conflict of interest
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
See Table 6.
Appendix 2
See Table 7.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nawijn, F., Hietbrink, F. & van Dijk, M.R. Getting it Right the First Time: Frozen Sections for Diagnosing Necrotizing Soft Tissue Infections. World J Surg 45, 148–159 (2021). https://doi.org/10.1007/s00268-020-05786-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05786-7