Abstract
Background
Liver resection and thermoablation are the mainstay of the surgical management of colorectal liver metastases (CRLM). The main limitation of thermoablation is the “heat-sink” effect for nodules next to large vessels. Herein, we report the preliminary results of microwave ablation (MWA) with associated Pringle maneuver to overcome this flaw.
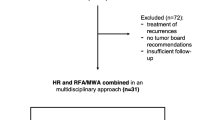
Methods
From November 2017, we performed intraoperative MWA with Pringle maneuver for nodules ≤3 cm with immediate proximity to large vessels (distance ≤ 5 mm, diameter ≥ 3 mm). We collected characteristics of nodules, surgical procedures and postoperative morbidity. Diameter of the ablation area, especially the ablative minimal margin, was calculated for each nodule. Recurrence was also evaluated.
Results
Nineteen patients underwent MWA with Pringle maneuver for 23 nodules. Nineteen (83%) ablated nodules were located in segments VI, VII and VIII, and one nodule was in segment I. Median size of nodules was 15 mm (10–21). No deaths occurred. Six patients (38%) experienced complications, among them only one was subsequent to the thermal ablation. Ablative minimal margin was ≥5 mm for 19 (83%) nodules. Margin was not sufficient for four nodules, among them only 2/23 cases (8.7%) of in situ recurrence occurred after 12 months of median follow-up.
Conclusions
In this preliminary study, MWA with Pringle maneuver was associated with a low related morbidity rate and favorable oncological outcome, especially when the radiological minimal margin was sufficient.




Similar content being viewed by others
References
Pan-Asian Adapted ESMO Consensus Guidelines for the Management of Patients with Metastatic Colorectal Cancer| ESMO. https://www.esmo.org/Guidelines/Gastrointestinal-Cancers/Pan-Asian-Adapted-ESMO-Consensus-Guidelines-for-the-Management-of-Patients-with-Metastatic-Colorectal-Cancer. Accessed 18 Aug 2019
ESMO Consensus Guidelines for the Management of Patients with Metastatic Colorectal Cancer|ESMO. https://www.esmo.org/Guidelines/Gastrointestinal-Cancers/Management-of-Patients-with-Metastatic-Colorectal-Cancer. Accessed 18 Aug 2019
Minami Y, Kudo M (2013) Radiofrequency ablation of liver metastases from colorectal cancer: a literature review. Gut Liver 7:1–6. https://doi.org/10.5009/gnl.2013.7.1.1
Vogl TJ, Nour-Eldin N-EA, Hammerstingl RM et al (2017) Microwave ablation (MWA): basics, Technique and results in primary and metastatic liver neoplasms—review article. Rofo 189:1055–1066. https://doi.org/10.1055/s-0043-117410
Goldberg SN, Hahn PF, Tanabe KK et al (1998) Percutaneous radiofrequency tissue ablation: does perfusion-mediated tissue cooling limit coagulation necrosis? J Vasc Interv Radiol 9:101–111
Ruiter SJS, Heerink WJ, de Jong KP (2019) Liver microwave ablation: a systematic review of various FDA-approved systems. Eur Radiol 29:4026–4035. https://doi.org/10.1007/s00330-018-5842-z
Pillai K, Akhter J, Chua TC et al (2015) Heat sink effect on tumor ablation characteristics as observed in monopolar radiofrequency, bipolar radiofrequency, and microwave, using ex vivo calf liver model. Medicine (Baltimore) 94:e580. https://doi.org/10.1097/MD.0000000000000580
Chetboun M, Kianmanesh R, Sommacale D et al (2016) Complete necrosis after microwave thermosphere ablation of liver metastases from colorectal cancer, histological proof of efficacy. J Surg Oncol 113:843–844. https://doi.org/10.1002/jso.24219
Piardi T, Lhuaire M, Memeo R et al (2016) Laparoscopic pringle maneuver: how we do it? Hepatobiliary Surg Nutr 5:345–349. https://doi.org/10.21037/hbsn.2015.11.01
Wang X, Sofocleous CT, Erinjeri JP et al (2013) Margin size is an independent predictor of local tumor progression after ablation of colon cancer liver metastases. Cardiovasc Intervent Radiol 36:166–175. https://doi.org/10.1007/s00270-012-0377-1
Heerink WJ, Solouki AM, Vliegenthart R et al (2018) The relationship between applied energy and ablation zone volume in patients with hepatocellular carcinoma and colorectal liver metastasis. Eur Radiol 28:3228–3236. https://doi.org/10.1007/s00330-017-5266-1
Regimbeau JM, Cosse C, Kaiser G et al (2017) Feasibility, safety and efficacy of two-stage hepatectomy for bilobar liver metastases of colorectal cancer: a LiverMetSurvey analysis. HPB (Oxford) 19:396–405. https://doi.org/10.1016/j.hpb.2017.01.008
Donadon M, Cescon M, Cucchetti A et al (2018) Parenchymal-sparing surgery for the surgical treatment of multiple colorectal liver metastases is a safer approach than major hepatectomy not impairing patients’ prognosis: a bi-institutional propensity score-matched analysis. Dig Surg 35:342–349. https://doi.org/10.1159/000479336
Alvarez FA, Sanchez Claria R, Oggero S, de Santibañes E (2016) Parenchymal-sparing liver surgery in patients with colorectal carcinoma liver metastases. World J Gastrointest Surg 8:407–423. https://doi.org/10.4240/wjgs.v8.i6.407
Memeo R, de Blasi V, Adam R et al (2016) Parenchymal-sparing hepatectomies (PSH) for bilobar colorectal liver metastases are associated with a lower morbidity and similar oncological results: a propensity score matching analysis. HPB 18:781–790. https://doi.org/10.1016/j.hpb.2016.06.004
Gillams A, Goldberg N, Ahmed M et al (2015) Thermal ablation of colorectal liver metastases: a position paper by an international panel of ablation experts, The Interventional Oncology Sans Frontières meeting 2013. Eur Radiol 25:3438–3454. https://doi.org/10.1007/s00330-015-3779-z
Chow FC-L, Chok KS-H (2019) Colorectal liver metastases: an update on multidisciplinary approach. World J Hepatol 11:150–172. https://doi.org/10.4254/wjh.v11.i2.150
Shady W, Petre EN, Do KG et al (2018) Percutaneous microwave versus radiofrequency ablation of colorectal liver metastases: ablation with clear margins (A0) provides the best local tumor control. J Vasc Interv Radiol 29:268–275.e1. https://doi.org/10.1016/j.jvir.2017.08.021
De Cobelli F, Marra P, Ratti F et al (2017) Microwave ablation of liver malignancies: comparison of effects and early outcomes of percutaneous and intraoperative approaches with different liver conditions : new advances in interventional oncology: state of the art. Med Oncol 34:49. https://doi.org/10.1007/s12032-017-0903-8
Barabino M, Gatti A, Santambrogio R et al (2017) Intraoperative local ablative therapies combined with surgery for the treatment of bilobar colorectal liver metastases. Anticancer Res 37:2743–2750
Chiappa A, Bertani E, Zbar AP et al (2016) Optimizing treatment of hepatic metastases from colorectal cancer: resection or resection plus ablation? Int J Oncol 48:1280–1289. https://doi.org/10.3892/ijo.2016.3324
Lu DSK, Raman SS, Limanond P et al (2003) Influence of large peritumoral vessels on outcome of radiofrequency ablation of liver tumors. J Vasc Interv Radiol 14:1267–1274
Ringe KI, Lutat C, Rieder C et al (2015) Experimental evaluation of the heat sink effect in hepatic microwave ablation. PLoS ONE 10:e0134301. https://doi.org/10.1371/journal.pone.0134301
Yu NC, Raman SS, Kim YJ et al (2008) Microwave liver ablation: influence of hepatic vein size on heat-sink effect in a porcine model. J Vasc Interv Radiol 19:1087–1092. https://doi.org/10.1016/j.jvir.2008.03.023
Kim C (2018) Understanding the nuances of microwave ablation for more accurate post-treatment assessment. Future Oncol 14:1755–1764. https://doi.org/10.2217/fon-2017-0736
Takahashi H, Kahramangil B, Kose E, Berber E (2018) A comparison of microwave thermosphere versus radiofrequency thermal ablation in the treatment of colorectal liver metastases. HPB (Oxford) 20:1157–1162. https://doi.org/10.1016/j.hpb.2018.05.012
Zaidi N, Okoh A, Yigitbas H et al (2016) Laparoscopic microwave thermosphere ablation of malignant liver tumors: an analysis of 53 cases. J Surg Oncol 113:130–134. https://doi.org/10.1002/jso.24127
Frich L, Mala T, Gladhaug IP (2006) Hepatic radiofrequency ablation using perfusion electrodes in a pig model: effect of the Pringle manoeuvre. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 32:527–532. https://doi.org/10.1016/j.ejso.2006.02.021
Shen P, Fleming S, Westcott C, Challa V (2003) Laparoscopic radiofrequency ablation of the liver in proximity to major vasculature: effect of the Pringle maneuver. J Surg Oncol 83:36–41. https://doi.org/10.1002/jso.10235
Smyrniotis V, Kostopanagiotou G, Theodoraki K et al (2004) The role of central venous pressure and type of vascular control in blood loss during major liver resections. Am J Surg 187:398–402. https://doi.org/10.1016/j.amjsurg.2003.12.001
de Baere T, Deschamps F, Briggs P et al (2008) Hepatic malignancies: percutaneous radiofrequency ablation during percutaneous portal or hepatic vein occlusion. Radiology 248:1056–1066. https://doi.org/10.1148/radiol.2483070222
Jungraithmayr W, Szarzynski M, Neeff H et al (2004) Significance of total vascular exclusion for hepatic cryotherapy: an experimental study. J Surg Res 116:32–41. https://doi.org/10.1016/s0022-4804(03)00054-4
Metcalfe MS, Mullin EJ, Texler M et al (2007) The safety and efficacy of radiofrequency and electrolytic ablation created adjacent to large hepatic veins in a porcine model. Eur J Surg Oncol 33:662–667. https://doi.org/10.1016/j.ejso.2007.02.011
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rhaiem, R., Kianmanesh, R., Minon, M. et al. Microwave Thermoablation of Colorectal Liver Metastases Close to Large Hepatic Vessels Under Pringle Maneuver Minimizes the “Heat Sink Effect”. World J Surg 44, 1595–1603 (2020). https://doi.org/10.1007/s00268-020-05379-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05379-4