Abstract
Background
Anatomical esophageal position may affect the short-term outcomes after minimally invasive esophagectomy (MIE). A previous single-institutional retrospective study suggested that the presence of a left-sided esophagus (LSE) made MIE more difficult and increased the incidence of postoperative complications.
Methods
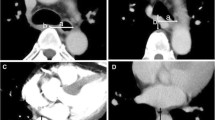
The current study was a multicenter retrospective study of 303 patients with esophageal cancer who underwent MIE at six esophageal cancer high-volume centers in Kyushu, Japan, between April 2011 and August 2016. The patients were divided into the LSE (66 patients) and non-LSE groups (237 patients) based on the esophageal position on computed tomography images obtained with the patients in the supine position.
Results
Univariate analysis showed that patients with LSE were significantly older than those with non-LSE (69 ± 8 vs. 65 ± 9 years; P = 0.002), had a significantly greater incidence of cardiovascular comorbidity (65.2% vs. 47.7%; P = 0.013), and a significantly longer operating time (612 ± 112 vs. 579 ± 102 min; P = 0.025). Logistic regression analysis verified that LSE was an independent risk factor for the incidence of pneumonia (odds ratio 3.3, 95% confidence interval 1.254–8.695; P = 0.016).
Conclusions
The presence of a LSE can increase the procedural difficulty of MIE and the incidence of morbidity after MIE. Thus, careful attention must be paid to anatomical esophageal position before performing MIE.

Similar content being viewed by others
References
Takeuchi H, Miyata H, Gotoh M et al (2014) A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg 260:259–266
Biere SS, van Berge Henegouwen MI, Maas KW et al (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet (Lond Engl) 379:1887–1892
Yoshida N, Yamamoto H, Baba H et al (2019) Can minimally invasive esophagectomy replace open esophagectomy for esophageal cancer? Latest analysis of 24,233 esophagectomies from the Japanese National Clinical Database. Ann Surg. https://doi.org/10.1097/SLA.0000000000003222
Baba Y, Yoshida N, Shigaki H et al (2016) Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single-institution study. Ann Surg 264:305–311
Molena D, Mungo B, Stem M et al (2014) Incidence and risk factors for respiratory complications in patients undergoing esophagectomy for malignancy: a NSQIP analysis. Semin Thorac Cardiovasc Surg 26:287–294
Yoshida N, Watanabe M, Baba Y et al (2014) Risk factors for pulmonary complications after esophagectomy for esophageal cancer. Surg Today 44:526–532
Shiozaki A, Fujiwara H, Okamura H et al (2012) Risk factors for postoperative respiratory complications following esophageal cancer resection. Oncol Lett 3:907–912
Paul DJ, Jamieson GG, Watson DI et al (2011) Perioperative risk analysis for acute respiratory distress syndrome after elective oesophagectomy. ANZ J Surg 81:700–706
Ferguson MK, Celauro AD, Prachand V (2011) Prediction of major pulmonary complications after esophagectomy. Ann Thorac Surg 91:1494–1500 (discussion 1491–1500)
Uchihara T, Yoshida N, Baba Y et al (2017) Risk factors for pulmonary morbidities after minimally invasive esophagectomy for esophageal cancer. Surg Endosc 32:2852–2858
Yoshida N, Baba Y, Shigaki H et al (2016) Effect of esophagus position on surgical difficulty and postoperative morbidities after thoracoscopic esophagectomy. Semin Thorac Cardiovasc Surg 28:172–179
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17:1471–1474
Kuwano H, Nishimura Y, Oyama T et al (2015) Guidelines for diagnosis and treatment of carcinoma of the esophagus April 2012 edited by the Japan Esophageal Society. Esophagus Off J Jpn Esophageal Soc 12:1–30
Raymond DP, Seder CW, Wright CD et al (2016) Predictors of major morbidity or mortality after resection for esophageal cancer: a society of thoracic surgeons general thoracic surgery database risk adjustment model. Ann Thorac Surg 102:207–214
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Okamura A, Watanabe M, Mine S et al (2016) Factors influencing difficulty of the thoracic procedure in minimally invasive esophagectomy. Surg Endosc 30:4279–4285
Zingg U, Smithers BM, Gotley DC et al (2011) Factors associated with postoperative pulmonary morbidity after esophagectomy for cancer. Ann Surg Oncol 18:1460–1468
Dhungel B, Diggs BS, Hunter JG et al (2010) Patient and peri-operative predictors of morbidity and mortality after esophagectomy: American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP), 2005-2008. J Gastrointest Surg Off J Soc Surg Aliment Tract 14:1492–1501
Nakamura M, Iwahashi M, Nakamori M et al (2008) An analysis of the factors contributing to a reduction in the incidence of pulmonary complications following an esophagectomy for esophageal cancer. Langenbeck’s Arch Surg 393:127–133
Yoshida N, Baba Y, Hiyoshi Y et al (2016) Duration of smoking cessation and postoperative morbidity after esophagectomy for esophageal cancer: how long should patients stop smoking before surgery? World J Surg 40:142–147
Yoshida N, Nakamura K, Kuroda D et al (2018) Preoperative smoking cessation is integral to the prevention of postoperative morbidities in minimally invasive esophagectomy. World J Surg 42:2902–2909
Yamana I, Takeno S, Hashimoto T et al (2015) Randomized controlled study to evaluate the efficacy of a preoperative respiratory rehabilitation program to prevent postoperative pulmonary complications after esophagectomy. Dig Surg 32:331–337
Inoue J, Ono R, Makiura D et al (2013) Prevention of postoperative pulmonary complications through intensive preoperative respiratory rehabilitation in patients with esophageal cancer. Dis Esophagus Off J Int Soc Dis Esophagus 26:68–74
Markar SR, Karthikesalingam A, Low DE (2015) Enhanced recovery pathways lead to an improvement in postoperative outcomes following esophagectomy: systematic review and pooled analysis. Dis Esophagus Off J Int Soc Dis Esophagus 28:468–475
Yoshida N, Baba Y, Shigaki H et al (2016) Preoperative nutritional assessment by controlling nutritional status (CONUT) is useful to estimate postoperative morbidity after esophagectomy for esophageal cancer. World J Surg 40:1910–1917
Filip B, Scarpa M, Cavallin F et al (2015) Postoperative outcome after oesophagectomy for cancer: nutritional status is the missing ring in the current prognostic scores. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 41:787–794
Akutsu Y, Matsubara H, Shuto K et al (2010) Pre-operative dental brushing can reduce the risk of postoperative pneumonia in esophageal cancer patients. Surgery 147:497–502
Iwahashi M, Nakamori M, Nakamura M et al (2014) Clinical benefits of thoracoscopic esophagectomy in the prone position for esophageal cancer. Surg Today 44:1708–1715
Markar SR, Wiggins T, Antonowicz S et al (2015) Minimally invasive esophagectomy: lateral decubitus vs. prone positioning; systematic review and pooled analysis. Surg Oncol 24:212–219
Yoshimura S, Mori K, Yamagata Y et al (2018) Quality of life after robot-assisted transmediastinal radical surgery for esophageal cancer. Surg Endosc 32:2249–2254
Acknowledgements
We thank Kelly Zammit, BVSc, and Cathel Kerr, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Uchihara, T., Yoshida, N., Baba, Y. et al. Esophageal Position Affects Short-Term Outcomes After Minimally Invasive Esophagectomy: A Retrospective Multicenter Study. World J Surg 44, 831–837 (2020). https://doi.org/10.1007/s00268-019-05273-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05273-8