Abstract
Background
A nutritional indicator suitable for predicting complications after esophagectomy has not been confirmed. The nutritional screening tool CONUT is a potential candidate.
Methods
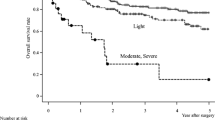
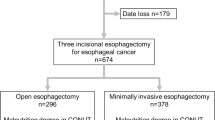
We retrospectively analyzed 352 patients who underwent elective esophagectomy with lymphadenectomy for esophageal cancer between April 2005 and December 2014. Patients were divided into three groups according to the malnutrition degree in controlling nutritional status (CONUT): normal, light malnutrition, moderate or severe malnutrition.
Results
The numbers of patients assigned to the normal, light malnutrition, and moderate or severe malnutrition groups were 205, 126, and 21, respectively. One hundred forty-seven (41.8 %) patients were considered malnourished. Patients with moderate or severe malnutrition had a significantly high incidence of any morbidity, severe morbidities, and surgical site infection. Hospital stay in patients with moderate or severe malnutrition was significantly longer. Logistic regression analysis suggested that moderate or severe malnutrition was an independent risk factor for any morbidity [hazard ratio (HR) 2.75, 95 % confidence interval (CI) 1.081–7.020; p = 0.034] and severe morbidities (HR 3.07, 95 % CI 1.002–9.432; p = 0.049).
Conclusions
CONUT was a convenient and useful tool to assess nutritional status before esophagectomy. Patients with moderate or severe malnutrition according to CONUT are at high risk for postoperative complications.

Similar content being viewed by others
References
Takeuchi H, Miyata H, Gotoh M et al (2014) A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg 260:259–266
Kurita N, Miyata H, Gotoh M et al (2015) Risk model for distal gastrectomy when treating gastric cancer on the basis of data from 33,917 Japanese patients collected using a nationwide web-based data entry system. Ann Surg 262:295–303
Watanabe M, Miyata H, Gotoh M et al (2014) Total gastrectomy risk model: data from 20,011 Japanese patients in a nationwide internet-based database. Ann Surg 260:1034–1039
Kobayashi H, Miyata H, Gotoh M et al (2014) Risk model for right hemicolectomy based on 19,070 Japanese patients in the National Clinical Database. J Gastroenterol 49:1047–1055
Matsubara N, Miyata H, Gotoh M et al (2014) Mortality after common rectal surgery in Japan: a study on low anterior resection from a newly established nationwide large-scale clinical database. Dis Colon Rectum 57:1075–1081
Kenjo A, Miyata H, Gotoh M et al (2014) Risk stratification of 7,732 hepatectomy cases in 2011 from the National Clinical Database for Japan. J Am Coll Surg 218:412–422
Kimura W, Miyata H, Gotoh M et al (2014) A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg 259:773–780
Mantziari S, Hübner M, Demartines N et al (2014) Impact of preoperative risk factors on morbidity after esophagectomy: is there room for improvement? World J Surg 38:2882–2890. doi:10.1007/s00268-014-2686-9
Ferguson MK, Celauro AD, Prachand V (2011) Assessment of a scoring system for predicting complications after esophagectomy. Dis Esophagus 24:510–515
Dutta S, Al-Mrabt NM, Fullarton GM et al (2011) A comparison of POSSUM and GPS models in the prediction of post-operative outcome in patients undergoing oesophago-gastric cancer resection. Ann Surg Oncol 18:2808–2817
Grotenhuis BA, van Hagen P, Reitsma JB et al (2010) Validation of a nomogram predicting complications after esophagectomy for cancer. Ann Thorac Surg 90:920–925
Dhungel B, Diggs BS, Hunter JG et al (2010) Patient and peri-operative predictors of morbidity and mortality after esophagectomy: American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP), 2005-2008. J Gastrointest Surg 14:1492–1501
Filip B, Scarpa M, Cavallin F et al (2015) Postoperative outcome after oesophagectomy for cancer: nutritional status is the missing ring in the current prognostic scores. Eur J Surg Oncol 41:787–794
Nozoe T, Kimura Y, Ishida M et al (2002) Correlation of pre-operative nutritional condition with post-operative complications in surgical treatment for oesophageal carcinoma. Eur J Surg Oncol 28:396–400
Ida S, Watanabe M, Yoshida N et al (2015) Sarcopenia is a predictor of postoperative respiratory complications in patients with esophageal cancer. Ann Surg Oncol 22:4432–4437
Yoshida N, Watanabe M, Baba Y et al (2014) Risk factors for pulmonary complications after esophagectomy for esophageal cancer. Surg Today 44:526–532
Sunpaweravong S, Ruangsin S, Laohawiriyakamol S et al (2012) Prediction of major postoperative complications and survival for locally advanced esophageal carcinoma patients. Asian J Surg 35:104–109
Findlay JM, Gillies RS, Millo J et al (2014) Enhanced recovery for esophagectomy: a systematic review and evidence-based guidelines. Ann Surg 259:413–431
Fukuda T, Seto Y, Yamada K et al (2008) Can immune-enhancing nutrients reduce postoperative complications in patients undergoing esophageal surgery? Dis Esophagus 21:708–711
Takeuchi H, Ikeuchi S, Kawaguchi Y et al (2007) Clinical significance of perioperative immunonutrition for patients with esophageal cancer. World J Surg 31:2160–2167. doi:10.1007/s00268-007-9219-8
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG et al (2005) CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp 20:38–45
López-Larramona G, Lucendo AJ, Tenías JM (2015) Association between nutritional screening via the Controlling Nutritional Status index and bone mineral density in chronic liver disease of various etiologies. Hepatol Res 45:618–628
Nochioka K, Sakata Y, Takahashi J, CHART-2 Investigators et al (2013) Prognostic impact of nutritional status in asymptomatic patients with cardiac diseases: a report from the CHART-2 Study. Circ J 77:2318–2326
Edge SB, Byrd DR, Compton CC et al (2009) AJCC cancer staging manual, 7th edn. Springer, New York
Society of Thoracic Surgeons (2013) Risk-adjusted morbidity and mortality for esophagectomy for cancer. http://www.sts.org/quality-research-patient-safety/quality/quality-performance-measures. Accessed 10 Oct 2015
National Cancer Institute (2010) Common Terminology Criteria for Adverse Events (CTCAE). United States Department of Health and Human Services. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf#search=‘http%3A%2F%2Fevs.nci.nih.gov%2Fftp1%2FCTCAE%2F+CTCAE_4.03_20100614_QuickReference_5x7.pdf. Accessed 10 Oct 2015
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Dickhaut SC, DeLee JC, Page CP (1984) Nutritional status: importance in predicting wound-healing after amputation. J Bone Joint Surg Am 66:71–75
Meguid MM, Mughal MM, Debonis D et al (1986) Influence of nutritional status on the resumption of adequate food intake in patients recovering from colorectal cancer operations. Surg Clin N Am 66:1167–1176
Detsky AS, Baker JP, O’Rourke K et al (1987) Predicting nutrition-associated complications for patients undergoing gastrointestinal surgery. J Parenter Enteral Nutr 11:440–446
Reilly JJ Jr, Gerhardt AL (1985) Modern surgical nutrition. Curr Probl Surg 22:1–81
Mazaki T, Ishii Y, Murai I (2015) Immunoenhancing enteral and parenteral nutrition for gastrointestinal surgery: a multiple-treatments meta-analysis. Ann Surg 261:662–669
Lawrence VA, Cornell JE, Smetana GW (2006) Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 144:596–608
Onodera T, Goseki N, Kosaki G (1984) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85:1001–1005
Han-Geurts IJ, Hop WC, Tran TC (2006) Nutritional status as a risk factor in esophageal surgery. Dig Surg 23:159–163
Noble F, Curtis N, Harris S et al (2012) Risk assessment using a novel score to predict anastomotic leak and major complications after oesophageal resection. J Gastrointest Surg 16:1083–1095
Sanz L, Ovejero VJ, González JJ et al (2006) Mortality risk scales in esophagectomy for cancer: their usefulness in preoperative patient selection. Hepatogastroenterology 53:869–873
Wang Q, Lau WY, Zhang B et al (2014) Preoperative total cholesterol predicts postoperative outcomes after partial hepatectomy in patients with chronic hepatitis B- or C-related hepatocellular carcinoma. Surgery 155:263–270
van Hagen P, Hulshof MC, van Lanschot JJ et al (2012) Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366:2074–2084
Fietkau R, Lewitzki V, Kuhnt T et al (2013) A disease-specific enteral nutrition formula improves nutritional status and functional performance in patients with head and neck and esophageal cancer undergoing chemoradiotherapy: results of a randomized, controlled, multicenter trial. Cancer 119:3343–3353
Hiura Y, Takiguchi S, Yamamoto K et al (2012) Effects of ghrelin administration during chemotherapy with advanced esophageal cancer patients: a prospective, randomized, placebo-controlled phase 2 study. Cancer 118:4785–4794
Brown RE, Abbas AE, Ellis S et al (2011) A prospective phase II evaluation of esophageal stenting for neoadjuvant therapy for esophageal cancer: optimal performance and surgical safety. J Am Coll Surg 212:582–588
Bower M, Jones W, Vessels B et al (2009) Nutritional support with endoluminal stenting during neoadjuvant therapy for esophageal malignancy. Ann Surg Oncol 16:3161–3168
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yoshida, N., Baba, Y., Shigaki, H. et al. Preoperative Nutritional Assessment by Controlling Nutritional Status (CONUT) is Useful to estimate Postoperative Morbidity After Esophagectomy for Esophageal Cancer. World J Surg 40, 1910–1917 (2016). https://doi.org/10.1007/s00268-016-3549-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3549-3