Abstract
Purpose
Optimal surgical management of perforated diverticulitis of the sigmoid colon has yet to be clearly defined. The purpose of this study was to evaluate efficacy of a “Damage Control Strategy” (DCS).
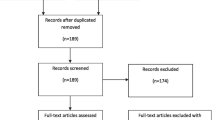
Materials and methods
Patients with perforated diverticulitis of the sigmoid colon complicated by generalized peritonitis (Hinchey III and IV) surgically treated according to a damage control strategy between May 2011 and February 2017 were enrolled in the present multicenter retrospective cohort study. Data were collected at three surgical centers. DCS comprises a two-stage concept: [1] limited resection of the perforated colon segment with oral and aboral blind closure during the emergency procedure and [2] definitive reconstruction at scheduled second laparotomy (anastomosis ∓ loop ileostomy or a Hartmann’s procedure) after 24–48 h.
Results
Fifty-eight patients were included into the analysis [W:M 28:30, median age 70.1 years (30–92)]. Eleven patients (19%) initially presented with fecal peritonitis (Hinchey IV) and 47 patients with purulent peritonitis (Hinchey III). An anastomosis could be created during the second procedure in 48 patients (83%), 14 of those received an additional loop ileostomy. In the remaining ten patients (n = 17%), an end colostomy was created at second laparotomy. A fecal diversion was performed in five patients to treat anastomotic complications. Thus, altogether, 29 patients (50%) had stoma at the end of the hospital stay. The postoperative mortality was 9% (n = 5), and median postoperative hospital stay was 18.5 days (3–66). At the end of the follow-up, 44 of 53 surviving patients were stoma free (83%).
Conclusion
The use of the Damage Control strategy leads to a comparatively low stoma rate in patients suffering from perforated diverticulitis with generalized peritonitis.

Similar content being viewed by others
References
Holmer C, Kreis ME (2014) Diverticular disease—choice of surgical procedure. Chir Z Für Alle Geb Oper Medizen 85(4):308–313
Vermeulen J, Gosselink MP, Busschbach JJV, Lange JF (2010) Avoiding or reversing Hartmann’s procedure provides improved quality of life after perforated diverticulitis. J Gastrointest Surg Off J Soc Surg Aliment Tract 14(4):651–657
Aydin HN, Remzi FH, Tekkis PP, Fazio VW (2005) Hartmann’s reversal is associated with high postoperative adverse events. Dis Colon Rectum 48(11):2117–2126
Oberkofler CE, Rickenbacher A, Raptis DA, Lehmann K, Villiger P, Buchli C (2012) A multicenter randomized clinical trial of primary anastomosis or Hartmann’s procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg 256(5):819–826
Jurowic C, Germer C-T (2016) Leitliniengerechte Therapie der Divertikulitis. Coloproctol 38(4):267–278
Vermeulen J, Coene PPLO, Van Hout NM, van der Harst E, Gosselink MP, Mannaerts GHH (2009) Restoration of bowel continuity after surgery for acute perforated diverticulitis: should Hartmann’s procedure be considered a one-stage procedure? Colorectal Dis Off J Assoc Coloproctol G B Irel 11(6):619–624
Kafka-Ritsch R, Birkfellner F, Perathoner A, Raab H, Nehoda H, Pratschke J (2012) Damage control surgery with abdominal vacuum and delayed bowel reconstruction in patients with perforated diverticulitis Hinchey III/IV. J Gastrointest Surg Off J Soc Surg Aliment Tract 16(10):1915–1922
Perathoner A, Klaus A, Mühlmann G, Oberwalder M, Margreiter R, Kafka-Ritsch R (2010) Damage control with abdominal vacuum therapy (VAC) to manage perforated diverticulitis with advanced generalized peritonitis–a proof of concept. Int J Colorectal Dis Juni 25(6):767–774
Langenfeld SJ (2013) Mandatory exploration is not necessary for patients with acute diverticulitis and free intraperitoneal air. J Trauma Acute Care Surg Mai 74(5):1376
Cirocchi R, Arezzo A, Vettoretto N, Cavaliere D, Farinella E, Renzi C (2014) Role of damage control surgery in the treatment of Hinchey III and IV sigmoid diverticulitis: a tailored strategy. Medicine (Baltimore) 93(25):e184
Sohn M, Agha A, Heitland W, Gundling F, Steiner P, Iesalnieks I (2016) Damage control strategy for the treatment of perforated diverticulitis with generalized peritonitis. Tech Coloproctol 20(8):577–583
Klarenbeek BR, de Korte N, van der Peet DL, Cuesta MA (2012) Review of current classifications for diverticular disease and a translation into clinical practice. Int J Colorectal Dis 27(2):207–214
Hinchey EJ, Schaal PG, Richards GK (1978) Treatment of perforated diverticular disease of the colon. Adv Surg 12:85–109
Demmel N, Muth G, Maag K, Osterholzer G (1994) Prognostic scores in peritonitis: the Mannheim Peritonitis Index or APACHE II? Langenbecks Arch Für Chir 379(6):347–352
Rogy M, Függer R, Schemper M, Koss G, Schulz F (1990) The value of 2 distinct prognosis scores in patients with peritonitis. The Mannheim Peritonitis Index versus the Apache II score. Chir Z Für Alle Geb Oper Medizen 61(4):297–300
Függer R, Rogy M, Herbst F, Schemper M, Schulz F (1988) Validation study of the Mannheim Peritonitis Index. Chir Z Für Alle Geb Oper Medizen 59(9):598–601
Brunkhorst F, Hagel S (2011) Sepsis. Intensivmed 48:57–73
Binda GA, Karas JR, Serventi A, Sokmen S, Amato A, Hydo L (2012) Primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a prematurely terminated randomized controlled trial. Colorectal Dis Off J Assoc Coloproctol G B Irel 14(11):1403–1410
Cirocchi R, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A (2013) Treatment of Hinchey stage III–IV diverticulitis: a systematic review and meta-analysis. Int J Colorectal Dis 28(4):447–457
O’Sullivan GC, Murphy D, O’Brien MG, Ireland A (1996) Laparoscopic management of generalized peritonitis due to perforated colonic diverticula. Am J Surg 171(4):432–434
Myers E, Hurley M, O’Sullivan GC, Kavanagh D, Wilson I, Winter DC (2008) Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg 95(1):97–101
Toorenvliet BR, Swank H, Schoones JW, Hamming JF, Bemelman WA (2010) Laparoscopic peritoneal lavage for perforated colonic diverticulitis: a systematic review. Colorectal Dis Off J Assoc Coloproctol G B Irel 12(9):862–867
Angenete E, Thornell A, Burcharth J, Pommergaard H-C, Skullman S, Bisgaard T (2016) Laparoscopic lavage is feasible and safe for the treatment of perforated diverticulitis with purulent peritonitis: the first results from the randomized controlled trial DILALA. Ann Surg 263(1):117–122
Swank HA, Vermeulen J, Lange JF, Mulder IM, van der Hoeven JAB, Stassen LPS (2010) The ladies trial: laparoscopic peritoneal lavage or resection for purulent peritonitis and Hartmann’s procedure or resection with primary anastomosis for purulent or faecal peritonitis in perforated diverticulitis (NTR2037). BMC Surg 10:29
Vennix S, Musters GD, Mulder IM, Swank HA, Consten EC, Belgers EH (2015) Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. Lancet Lond Engl 386(10000):1269–1277
Schultz JK, Yaqub S, Wallon C, Blecic L, Forsmo HM, Folkesson J (2015) Laparoscopic lavage vs primary resection for acute perforated diverticulitis: the SCANDIV randomized clinical trial. JAMA 314(13):1364–1375
Kruis W, Germer C-T, Leifeld L (2014) German Society for Gastroenterology, Digestive and Metabolic Diseases and The German Society for General and Visceral Surgery. Diverticular disease: guidelines of the german society for gastroenterology, digestive and metabolic diseases and the german society for general and visceral surgery. Digestion 90(3):190–207
Leifeld L, Germer CT, Böhm S, Dumoulin FL, Häuser W, Kreis M (2014) S2k guidelines diverticular disease/diverticulitis. Z Für Gastroenterol 52(7):663–710
Author information
Authors and Affiliations
Contributions
MS, II, AA, PS, AH, JP, PR, and FA contributed significantly to the design of the study, interpretation of data, drafting of the manuscript, critical revision, and final approval of this work. All authors agree to be accountable for the accuracy and integrity of this work.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sohn, M., Iesalnieks, I., Agha, A. et al. Perforated Diverticulitis with Generalized Peritonitis: Low Stoma Rate Using a “Damage Control Strategy”. World J Surg 42, 3189–3195 (2018). https://doi.org/10.1007/s00268-018-4585-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4585-y