Abstract
Background
Primary hyperaldosteronism (PHA) frequently causes secondary hypertension and is a surgically amenable disease if associated with unilateral adenoma. Patients who underwent laparoscopic adrenalectomy at the authors’ department were followed to identify clinical parameters that predict resolution of hypertension.
Methods
All patients with PHA and adrenalectomy from 1993 to 2009 were identified. Charts and follow-up data were reviewed for clinical parameters and hormone levels. Univariate and multivariate analysis were performed with SPSS 15.0.
Results
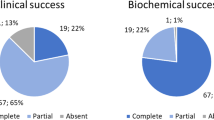
A cohort of 30 female and 24 male patients underwent laparoscopic adrenalectomy. Hypokalemia was observed in 47/54 (87%) patients. Twenty patients (37%) were cured without any further need of antihypertensive medication, 20 (37%) patients experienced an improvement in hypertension, and 14 (26%) patients remain unaffected. Consequently, hypertension was resolved or improved in 40/54 (74%) patients. A shorter duration of hypertension (<6 years), the number of antihypertensive drugs (<3), and the serum creatinine level (<1.3 mmol/l) were independent predictors of resolution of hypertension in a multivariate analysis. At final follow-up after a mean of 49 ± 40 months, resolution of hypertension was observed in 17/30 (57%) patients. Interestingly, in 10/17 patients a period longer than 12 months was required before a resolution of hypertension was observed. Coexistent hyperplasia, which was observed in 30% of patients, did not correlate with outcome.
Conclusions
In 50% of patients with PHA, hypertension resolves after laparoscopic adrenalectomy, but the process may require more than 12 months. Patients with a duration of hypertension of more than 6 years, more than 3 antihypertensive drugs, and elevated serum creatinine have a higher risk of persistent hypertension after surgery. Coexistent hyperplasia in the resected adrenal gland is not associated with persistent hypertension.
Similar content being viewed by others
Notes
Hyperplasia was defined by adrenocortical hyperplasia without the presence of an adenoma.
Coexisting hyperplasia was defined when both hyperplasia and an adenoma were present in one resected gland.
References
Young WF Jr (1999) Primary aldosteronism: a common and curable form of hypertension. Cardiol Rev 7:207–214
Lund JO, Nielsen MD, Giese J (1981) Prevalence of primary aldosteronism. Acta Med Scand 646(Suppl):54–57
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, Ganzaroli C, Giacchetti G, Letizia C, Maccario M, Mallamaci F, Mannelli M, Mattarello MJ, Moretti A, Palumbo G, Parenti G, Porteri E, Semplicini A, Rizzoni D, Rossi E, Boscaro M, Pessina AC, Mantero F (2006) A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol 48:2293–2300
Toniato A, Bernante P, Rossi GP, Pelizzo MR (2006) The role of adrenal venous sampling in the surgical management of primary aldosteronism. World J Surg 30:624–627. doi:10.1007/s00268-005-0482-2
Young WF, Stanson AW, Thompson GB, Grant CS, Farley DR, van Heerden JA (2004) Role for adrenal venous sampling in primary aldosteronism. Surgery 136:1227–1235
Abe M, Hamada M, Matsuoka H, Shigematsu Y, Sumimoto T, Hiwada K (1994) Myocardial scintigraphic characteristics in patients with primary aldosteronism. Hypertension 23(Suppl 1):I164–I167
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ (2005) Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol 45:1243–1248
Yip L, Lee JE, Shapiro SE, Waguespack SG, Sherman SI, Hoff AO, Gagel RF, Arens JF, Evans DB (2004) Surgical management of hereditary pheochromocytoma. J Am Coll Surg 198:525–534 discussion 534–535
de Graaf JS, Dullaart RP, Zwierstra RP (2003) Complications after bilateral adrenalectomy for pheochromocytoma in multiple endocrine neoplasia type 2—a plea to conserve adrenal function. Eur J Surg 165:843–846
Sawka AM, Young WF, Thompson GB, Grant CS, Farley DR, Leibson C, van Heerden JA (2001) Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med 135:258–261
Blumenfeld JD, Sealey JE, Schlussel Y, Vaughan ED Jr, Sos TA, Atlas SA, Muller FB, Acevedo R, Ulick S, Laragh JH (1994) Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med 121:877–885
Meria P, Kempf BF, Hermieu JF, Plouin PF, Duclos JM (2003) Laparoscopic management of primary hyperaldosteronism: clinical experience with 212 cases. J Urol 169:32–35
Ishidoya S, Ito A, Sakai K, Satoh M, Chiba Y, Sato F, Arai Y (2005) Laparoscopic partial versus total adrenalectomy for aldosterone producing adenoma. J Urol 174:40–43
Obara T, Ito Y, Okamoto T, Kanaji Y, Yamashita T, Aiba M, Fujimoto Y (1992) Risk factors associated with postoperative persistent hypertension in patients with primary aldosteronism. Surgery 112:987–993
Proye CA, Mulliez EA, Carnaille BM, Lecomte-Houcke M, Decoulx M, Wemeau JL, Lefebvre J, Racadot A, Ernst O, Huglo D, Carre A (1998) Essential hypertension: first reason for persistent hypertension after unilateral adrenalectomy for primary aldosteronism? Surgery 124:1128–1133
Lo CY, Tam PC, Kung AW, Lam KS, Wong J (1996) Primary aldosteronism. Results of surgical treatment. Ann Surg 224:125–130
Zarnegar R, Young WF Jr, Lee J, Sweet MP, Kebebew E, Farley DR, Thompson GB, Grant CS, Clark OH, Duh QY (2008) The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg 247:511–518
Roggenland D, Schneider S, Klein HH, Kann PH (2006) Endosonography—an additional diagnostic possibility in the differentiation between the two common types of primary hyperaldosteronism. Med Klin (Munich) 101:65–68 [in German]
Kann PH (2005) Endoscopic ultrasound imaging of the adrenals. Endoscopy 37:244–253
Young WF (2007) Primary aldosteronism: renaissance of a syndrome. Clin Endocrinol (Oxf) 66:607–618
Bruschi G, Banchini E, Mutti A, Biggi A, Coruzzi P, Civardi E, Martinelli M, Novarini A (1977) Physiopathological and functional semeiologic considerations in a case of primary normoaldosteronemic hyperaldosteronism. Ateneo Parmense Acta Biomed 48:157–165
Brunt LM, Moley JF, Doherty GM, Lairmore TC, DeBenedetti MK, Quasebarth MA (2001) Outcomes analysis in patients undergoing laparoscopic adrenalectomy for hormonally active adrenal tumors. Surgery 130:629–634 discussion 634–635
Pang TC, Bambach C, Monaghan JC, Sidhu SB, Bune A, Delbridge LW, Sywak MS (2007) Outcomes of laparoscopic adrenalectomy for hyperaldosteronism. ANZ J Surg 77:768–773
Celen O, O’Brien MJ, Melby JC, Beazley RM (1996) Factors influencing outcome of surgery for primary aldosteronism. Arch Surg 131:646–650
Meyer A, Brabant G, Behrend M (2005) Long-term follow-up after adrenalectomy for primary aldosteronism. World J Surg 29:155–159. doi:10.1007/s00268-004-7496-z
Goh BK, Tan YH, Yip SK, Eng PH, Cheng CW (2004) Outcome of patients undergoing laparoscopic adrenalectomy for primary hyperaldosteronism. JSLS 8:320–325
Rossi H, Kim A, Prinz RA (2002) Primary hyperaldosteronism in the era of laparoscopic adrenalectomy. Am Surg 68:253–256 discussion 256–257
Murashima M, Trerotola SO, Fraker DL, Han D, Townsend RR, Cohen DL (2009) Change in the pattern of adrenal venous sampling over time in patients with primary aldosteronism. J Hum Hypertens 23:292–294
Sukor N, Gordon RD, Ku YK, Jones M, Stowasser M (2009) Role of unilateral adrenalectomy in bilateral primary aldosteronism: a 22-year single center experience. J Clin Endocrinol Metab 94:2437–2445
Sechi LA, Novello M, Lapenna R, Baroselli S, Nadalini E, Colussi GL, Catena C (2006) Long-term renal outcomes in patients with primary aldosteronism. JAMA 295:2638–2645
Fukudome Y, Fujii K, Arima H, Ohya Y, Tsuchihashi T, Abe I, Fujishima M (2002) Discriminating factors for recurrent hypertension in patients with primary aldosteronism after adrenalectomy. Hypertens Res 25:11–18
Murashima M, Trerotola SO, Fraker DL, Han D, Townsend RR, Cohen DL (2009) Adrenal venous sampling for primary aldosteronism and clinical outcomes after unilateral adrenalectomy: a single-center experience. J Clin Hypertens (Greenwich) 11:316–323
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Waldmann, J., Maurer, L., Holler, J. et al. Outcome of Surgery for Primary Hyperaldosteronism. World J Surg 35, 2422–2427 (2011). https://doi.org/10.1007/s00268-011-1221-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1221-5