Abstract
Purpose
Endocrinopathies constitute ~ 10% of secondary hypertension (SH) etiologies. Primary aldosteronism, pheochromocytoma (PHEO), and Cushing’s syndrome are common causes. Early identification and treatment result in resolution/improvement of SH. The aim of this study was to characterize the clinical course, outcomes, and remission-associated prognostic factors of SH related to adrenal tumors.
Methods
Retrospective cohort study including patients with SH who underwent adrenalectomy from 2000 to 2019. Postoperative outcomes were analyzed. Remission was defined as normalization of blood pressure without drug use.
Results
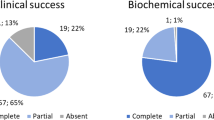
Eighty-three patients with SH were included. Mean ± SD age was 38.8 ± 14.2 years and 75.9% were women. Diagnosis was PHEO in 35 patients (42.2%), aldosteronoma (APA) in 28 (33.7%), cortisol producing adenoma (CPA) in 16 (19.3%), and ACTH-dependent Cushing’s in 4 (4.8%). Laparoscopic adrenalectomy was performed in 81 (97.6%) patients. Mean ± SD follow-up was 57.4 ± 49.6 months (range 1–232). Surgical morbidity occurred in 7.2% of patients and there was no mortality. Remission of SH occurred in 61(73.5%): 100% of ACTH-dependent Cushing’s, 85.7% of PHEO, 68.8% of CPA, and 57.1% of APA. Biochemical phenotype and the combination of larger tumor size, number of antihypertensive drugs, male gender, older age, obesity, and preoperative SH for more than 5 years were associated with less likely clinical remission in patients with APA (p = 0.004), CPA (p < 0.0001), and PHEO (p < 0.0001).
Conclusion
SH remission rates are 57–100% after adrenalectomy. Several prognostic factors could be used to predict SH control. Adrenalectomy provides good clinical outcome and must be considered a treatment option in all surgical candidates.


Similar content being viewed by others
References
Pappachan JM, Buch HN (2017) Endocrine hypertension : a practical approach when to suspect endocrine. Adv Exp Med Biol 956:215–237
Rosas-Peralta M, Palomo-Piñón S, Borrayo-Sánchez G et al (2016) Consenso de Hipertensión Arterial Sistémica en México. Rev Med Inst MEx Seguro Soc 54(1):S6-51
Barquera S, Campos-Nonato I, Hernández-Barrera L et al (2010) Hypertension in Mexican adults: results from the National Health and Nutrition Survey 2006. Salud Publica Mex 52(SUPPL.1):63–71
Mancia G, De Backer G, Dominiczak A, et al. (2018)ESC/ESH Guidelines for the Management of Arterial Hypertension. Vol 25.; 2018
Omura M, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T (2004) Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertens Res 27(3):193–202
Thomas RM, Ruel E, Shantavasinkul PC, Corsino L (2015) Endocrine hypertension: an overview on the current etiopathogenesis and management options. World J Hypertens 5(2):14–27. https://doi.org/10.5494/wjh.v5.i2.14.Endocrine
Bouznad N, El Mghari G, El Ansari N (2016) Etiology of endocrine arterial hypertensions: about a series of cases. PanAfrican Med J 7(23):170. https://doi.org/10.11604/pamj.2016.23.170.8968
Wrenn SM, Vaidya A, Lubitz CC (2020) Primary aldosteronism. Gland Surg 9(1):14–24. https://doi.org/10.21037/gs.2019.10.23
Neumann HPH, Young WF, Eng C (2019) Pheochromocytoma and paraganglioma. N Engl J Med 381(6):552–565. https://doi.org/10.1056/NEJMra1806651
Morris LF, Harris RS, Milton DR et al (2013) Impact and timing of bilateral adrenalectomy for refractory adrenocorticotropic hormone-dependent Cushing’s syndrome. Surgery 154(6):1174. https://doi.org/10.1016/j.surg.2013.06.017
Nieman LK (2018) Recent updates on the diagnosis and management of Cushing’s syndrome. Endocrinol Metab (Seoul, Korea) 33(2):139–146. https://doi.org/10.3803/EnM.2018.33.2.139
Grasso M, Boscaro M, Scaroni C, Ceccato F (2018) Secondary arterial hypertension : from routine clinical practice to evidence in patients with adrenal tumor. High Blood Press Cardiovasc Prev
Yang J, Shen J, Fuller PJ (2017) A practical approach to diagnosing endocrine hypertension. Nephrology 22(9):633–677. https://doi.org/10.1111/nep.13078
Brunt LM, Moley JF, Doherty GM, Lairmore TC, DeBenedetti MK, Quasebarth MA (2001) Outcomes analysis in patients undergoing laparoscopic adrenalectomy for hormonally active adrenal tumors. Surgery 130(4):629–635. https://doi.org/10.1067/msy.2001.116920
Pogorzelski R, Toutounchi S, Krajewska E et al (2014) The effect of surgical treatment of phaeochromocytoma on concomitant arterial hypertension and diabetes mellitus in a single-centre retrospective study. Cent Eur J Urol 67(4):361–365. https://doi.org/10.5173/ceju.2014.04.art9
Falhammar H, Kjellman M, Calissendorff J (2018) Treatment and outcomes in pheochromocytomas and paragangliomas: a study of 110 cases from a single center. Endocrine 62(3):566–575. https://doi.org/10.1007/s12020-018-1734-x
Mamilla D, Araque KA, Brofferio A et al (2019) Postoperative management in patients with pheochromocytoma and paraganglioma. Cancers (Basel) 11(7):936. https://doi.org/10.3390/cancers11070936
Huang K-H, Chung S-D, Chen S-C et al (2007) Clinical and pathological data of 10 malignant pheochromocytomas: long-term follow up in a single institute. Int J Urol 14(3):181–185. https://doi.org/10.1111/j.1442-2042.2007.01687.x
Lenders JWM, Eisenhofer G (2017) Update on modern management of pheochromocytoma and paraganglioma. Endocrinol Metab (Seoul, Korea) 32(2):152–161. https://doi.org/10.3803/EnM.2017.32.2.152
Weigel RJ, Wells SA, Gunnells JC, Leight GS (1994) Surgical treatment of primary hyperaldosteronism. Ann Surg 219(4):347–352. https://doi.org/10.1097/00000658-199404000-00004
Lo CY, Tam PC, Kung AW, Lam KS, Wong J (1996) Primary aldosteronism. Results of surgical treatment Ann Surg 224(2):125–130. https://doi.org/10.1097/00000658-199608000-00003
Gil-Cárdenas A, Cordón C, Gamino R et al (2008) Laparoscopic adrenalectomy: lessons learned from an initial series of 100 patients. Surg Endosc Other Interv Tech 22(4):991–994. https://doi.org/10.1007/s00464-007-9556-6
Williams TA, Lenders JWM, Mulatero P et al (2017) Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol 5(9):689–699. https://doi.org/10.1016/S2213-8587(17)30135-3
Zarnegar R, Young WFJ, Lee J et al (2008) The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg 247(3):511–518. https://doi.org/10.1097/SLA.0b013e318165c075
Funder JW, Carey RM, Mantero F et al (2016) The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 101(5):1889–1916. https://doi.org/10.1210/jc.2015-4061
He BJ, Anderson ME (2013) Aldosterone and cardiovascular disease: the heart of the matter. Trends Endocrinol Metab 24(1):21–30. https://doi.org/10.1016/j.tem.2012.09.004
Wolley M, Thuzar M, Stowasser M (2020) Controversies and advances in adrenal venous sampling in the diagnostic workup of primary aldosteronism. Best Pract Res Clin Endocrinol Metab 34(3):101400. https://doi.org/10.1016/j.beem.2020.101400
Charles L, Triscott J, Dobbs B (2017) Secondary hypertension: discovering the underlying cause. Am Fam Physician 96(7):453–461
Cicala MV, Mantero F (2010) Hypertension in Cushing’s syndrome: from pathogenesis to treatment. Neuroendocrinology 92(Suppl 1):44–49. https://doi.org/10.1159/000314315
Sacerdote A, Weiss K, Tran T et al (2005) Hypertension in patients with Cushing’s disease: pathophysiology, diagnosis, and management. Curr Hypertens Rep 7(3):212–218. https://doi.org/10.1007/s11906-005-0013-4
Schernthaner-Reiter MH, Siess C, Gessl A et al (2019) Factors predicting long-term comorbidities in patients with Cushing’s syndrome in remission. Endocrine 64(1):157–168. https://doi.org/10.1007/s12020-018-1819-6
Iacobone M, Mantero F, Basso SM, Lumachi F, Favia G (2005) Results and long-term follow-up after unilateral adrenalectomy for ACTH-independent hypercortisolism in a series of fifty patients. J Endocrinol Invest 28(4):327–332. https://doi.org/10.1007/BF03347198
Jha S, Sinaii N, McGlotten RN, Nieman LK (2020) Remission of hypertension after surgical cure of Cushing’s syndrome. Clin Endocrinol (Oxf) 92(2):124–130. https://doi.org/10.1111/cen.14129
Alvarez D, Tuzon A, Meseguer M, Sebastian C, Galeano J, Ponce JL (2010) [Laparoscopic adrenalectomy. Analysis of 100 cases]. Cir Esp 87(1):39–44. https://doi.org/10.1016/j.ciresp.2009.06.014
Vorselaars WMCM, Postma EL, Mirallie E et al (2018) Hemodynamic instability during surgery for pheochromocytoma: comparing the transperitoneal and retroperitoneal approach in a multicenter analysis of 341 patients. Surgery 163(1):176–182. https://doi.org/10.1016/j.surg.2017.05.029
Brunaud L, Nguyen-Thi P-L, Mirallie E et al (2016) Predictive factors for postoperative morbidity after laparoscopic adrenalectomy for pheochromocytoma: a multicenter retrospective analysis in 225 patients. Surg Endosc 30(3):1051–1059. https://doi.org/10.1007/s00464-015-4294-7
Carr AA, Wang TS (2016) Minimally Invasive Adrenalectomy. Surg Oncol Clin N Am 25(1):139–152. https://doi.org/10.1016/j.soc.2015.08.007
Author information
Authors and Affiliations
Contributions
Study conception and design: Clemente-Gutierrez U, Herrera MF, and Velazquez-Fernandez D. Acquisition of data: Clemente-Gutierrez U, Perez Soto RH, Hernandez-Acevedo JD, and Casanueva-Perez E. Analysis and interpretation of data: Clemente-Gutierrez U., Herrera MF, and Velazquez-Fernandez D. Drafting of manuscript: Clemente-Gutierrez U., Herrera MF, and Velazquez-Fernandez D. Critical revision of manuscript: Clemente-Gutierrez U., Iniguez-Ariza N, Pantoja-Millan J, Sierra-Salazar M, Herrera MF, and Velazquez-Fernandez D.
Corresponding author
Ethics declarations
Ethics approval
This protocol was approved by the institutional bioethics committee for human research (# 3190) of our institution.
Informed consent
Due to the retrospective nature of this research, the institutional bioethics committee for human research exempted the need for informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Clemente-Gutiérrez, U., Pérez-Soto, R.H., Hernández-Acevedo, J.D. et al. Endocrine hypertension secondary to adrenal tumors: clinical course and predictive factors of clinical remission. Langenbecks Arch Surg 406, 2027–2035 (2021). https://doi.org/10.1007/s00423-021-02245-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02245-2