Abstract
Background
Pancreaticobiliary reflux is a pathologic phenomenon occurring in patients with gallstones. However, the occurrence of pancreaticobiliary reflux has not been studied in patients without gallstones. The objective of the present study was to measure the bile levels of amylase and lipase in patients without gallstones submitted to cholecystectomy as part of another surgical procedure, and to compare these values with the bile levels of amylase and lipase of patients submitted to cholecystectomy for gallstone disease.
Patients and methods
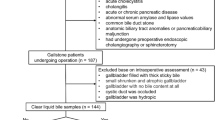
A prospective observational and comparative study was designed. A sample of 136 consecutive patients was included. Amylase and lipase levels were measured in bile. At our institution, normal plasma concentrations of amylase are 28–100 IU/l and lipase 13–60 IU/l. Normal values for pancreatic enzyme concentrations in bile have not been established. Therefore, bile amylase and lipase concentrations exceeding normal plasma concentrations were deemed to be elevated.
Results
Of the patients in the present study, 103 (76%) had gallstones and 33 (24%) had healthy gallbladders without gallstones. According to normal plasma levels for amylase and lipase, these enzymes in bile were elevated in 83.5% patients with gallstones, compared to elevated levels of amylase in 6% patients and lipase in 3% patients without gallstones (P < 0.0001).
Conclusions
Pancreaticobiliary reflux is a common phenomenon in patients with gallstones and an uncommon phenomenon in patients with healthy gallbladders without gallstone disease.



Similar content being viewed by others
References
Sai JK, Suyama M, Kubokawa Y et al (2003) Occult pancreaticobiliary reflux in patients with a normal pancreaticobiliary junction. Gastrointest Endosc 57:364–368
Horaguchi J, Fujita N, Noda Y et al (2008) Amylase levels in bile in patients with a morphologically normal pancreaticobiliary ductal arrangement. J Gastroenterol 43:305–311
Kamisawa T, Okamoto A (2006) Biliopancreatic and pancreaticobiliary refluxes in cases with and without pancreaticobiliary maljunction: diagnosis and clinical implications. Digestion 73:223–236
Beltrán MA, Vracko J, Cumsille MA et al (2007) Occult pancreaticobiliary reflux in gallbladder cancer and benign gallbladder diseases. J Surg Oncol 96:26–31
Mizuno M, Kato T, Koyama K (1996) An analysis of mutagens in the contents of the biliary tract in pancreaticobiliary maljunction. Surg Today 26:597–602
Ito T, Tsuchida A, Itokawa F et al (2005) Histologic and genetic analysis of the gallbladder in patients with occult pancreaticobiliary reflux. Int J Mol Med 15:425–430
Sai JK, Suyama M, Nobukawa B et al (2005) Precancerous mucosal changes in the gallbladder of patients with occult pancreaticobiliary reflux. Gastrointest Endosc 61:264–268
Sai JK, Suyama M, Kubokawa Y (2006) A case of gallbladder carcinoma associated with pancreaticobiliary reflux in the absence of pancreaticobiliary maljunction: a hint for early diagnosis of gallbladder carcinoma. World J Gastroenterol 28:4593–4595
Inagaki M, Goto J, Suzuki S et al (2007) Gallbladder carcinoma associated with occult pancreaticobiliary reflux in the absence of pancreaticobiliary maljunction. J Hepatobiliary Pancreat Surg 14:529–533
Sai JK, Suyama M, Nobukawa B et al (2005) Severe dysplasia of the gallbladder associated with occult pancreaticobiliary reflux. J Gastroenterol 40:756–760
Lenriot JP, Gigot JF, Segol P et al (1998) Bile duct cysts in adults: a multi-institutional retrospective study. Ann Surg 228:159–166
Kimura K, Ohto M, Ono T et al (1977) Congenital cystic dilatation of the common bile duct: relationships to anomalous pancreaticobiliary ductal union. AJR Am J Roentgenol 128:571–577
McKee MD (2007) Pancreaticobiliary reflux and gallbladder cancer. J Surg Oncol 96:455–456
Anderson MC, Hauman RL, Suriyapa C et al (1979) Pancreatic enzymes levels in bile of patients with extrahepatic biliary disease. Am J Surg 137:301–306
Vracko J, Wiechel KL (2003) Increased gallbladder trypsin in acute cholecystitis indicates functional disorder in the sphincter of Oddi and could make EPT a logical procedure. Surg Laparosc Endosc Percutan Tech 13:308–313
Itokawa F, Itoi T, Nakamura K et al (2004) Assessment of occult pancreaticobiliary reflux in patients with pancreaticobiliary disease by ERCP. J Gastroenterol 39:988–994
Beltrán MA, Barría C (2007) Heterotopic pancreas in the gallbladder—the importance of an uncommon condition. Pancreas 34:488–491
Ko CW, Schulte SJ, Lee SP (2005) Biliary sludge is formed by modification of hepatic bile by the gallbladder mucosa. Clin Gastroenterol Hepatol 3:672–678
Tazuma S, Kajiyama G (2001) Carcinogenesis of malignant lesions of the gallbladder—the impact of chronic inflammation and gallstones. Langenbecks Arch Surg 386:224–229
Chao TC, Wang CS, Jan YY et al (1999) Carcinogenesis in the biliary system associated with APDJ. J Hepatobiliary Pancreat Surg 6:218–222
Masumoto Y, Fujii H, Itakura J et al (2003) Pancreaticobiliary maljunction: pathophysiological and clinical aspects and the impact in biliary carcinogenesis. Langenbecks Arch Surg 388:122–131
Funabiki T, Matsubara T, Miyakawa S et al (2009) Pancreaticobiliary maljunction and carcinogenesis to biliary and pancreatic malignancy. Langenbecks Arch Surg 394:159–169
Cicala M, Habib FI, Fiocca F et al (2001) Increased sphincter of Oddi basal pressure in patients affected by gallstone disease: a role for biliary stasis and colicky pain? Gut 48:414–417
Tanaka M, Ikeda S, Kawakami K et al (1982) The presence of a positive pressure gradient from pancreatic to choledochal cyst demonstrated by duodenoscopic micro-transducer manometry: clue to pancreaticobiliary reflux. Endoscopy 14:45–47
Vracko J, Markovic S, Wiechel KL (2006) Conservative treatment versus endoscopic sphincterotomy in the management of acute cholecystitis in elderly patients at surgical risk. Endoscopy 38:773–778
Vracko J, Zemva Z, Pegan V et al (1994) Sphincter of Oddi function studied by radioimmunoassay of biliary trypsin in patients with bile duct stones and in controls. Surg Endosc 8:389–392
Vracko J, Wiechel KL (2000) Trypsin level in gallbladder bile and ductitis and width of the cystic duct. Hepatogastroenterology 47:115–120
Hjorth E (1947) Contributions to the knowledge of pancreatic reflux as a factor in chronic affections of the gallbladder. Acta Chir Scand 96:12–29
Tzovaras G, Rowlands BJ (1988) Diagnosis and treatment of sphincter of Oddi dysfunction and other functional biliary disorders. Br J Surg 85:588–595
Eversman D, Fogel EL, Rusche M et al (1999) Frequency of abnormal pancreatic and biliary sphincter manometry compared with clinical suspicion of sphincter of Oddi dysfunction. Gastrointest Endosc 50:637–641
Petersen BT (2004) An evidence-based review of sphincter of Oddi dysfunction: part I, presentations with “objective” biliary findings (types I and II). Gastrointest Endosc 59:525–534
Prajapati DN, Hogan WJ (2003) Diagnosis and treatment of sphincter of Oddi dysfunction. Gastroenterol Clin North Am 32:601–618
Yokohata K, Tanaka M (2000) Cyclic motility of the sphincter of Oddi. J Hepatobiliary Pancreat Surg 7:178–182
Tanaka M (2002) Advances in research and clinical practice in motor disorders of the sphincter of Oddi. J Hepatobiliary Pancreat Surg 9:564–568
Canfield AJ, Hetz SP, Schriver JP et al (1998) Biliary dyskinesia: a study of more than 200 patients and review of the literature. J Gastrointest Surg 2:443–448
Amaral J, Xiao ZL, Chen Q et al (2001) Gallbladder muscle dysfunction in patients with chronic acalculous disease. Gastroenterology 120:506–511
Chen PF, Nimeri A, Pham QH et al (2001) The clinical diagnosis of chronic acalculous cholecystitis. Surgery 130:578–583
Acknowledgments
This work is registered as Clinicaltrials.Gov—Protocol Registration System—Nct00890201.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beltrán, M.A., Contreras, M.A. & Cruces, K.S. Pancreaticobiliary Reflux in Patients with and without Cholelithiasis: Is It a Normal Phenomenon?. World J Surg 34, 2915–2921 (2010). https://doi.org/10.1007/s00268-010-0771-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0771-2