Abstract
Purpose
Only a few reports have been published so far on factors that predict postoperative coronal alignment after unicompartmental knee arthroplasty (UKA). The purpose of this study is to clarify the relationship between the arithmetic hip-knee-ankle angle (aHKA) and postoperative coronal alignment after medial fixed-bearing UKA.
Methods
One hundred and one consecutive patients (125 knees) who underwent medial fixed-bearing UKA were assessed. Pre- and postoperative coronal HKA angles, lateral distal femoral angle (LDFA), medial proximal tibial angle (MPTA), and the thickness of the tibial and femoral bone cut were measured. aHKA was calculated as 180° − LDFA + MPTA. Correlations between postoperative HKA angle and aHKA, LDFA, and MPTA were investigated by single regression analysis. After the patients were divided into three groups according to the postoperative HKA angle, i.e., HKA angle > 180°, 175° < HKA angle ≤ 180°, and HKA angle ≤ 175°, aHKA, LDFA, MPTA, preoperative HKA angle, and the thickness of the distal femoral as well as tibial bone cut were compared among the three groups.
Results
aHKA and MPTA were positively correlated with postoperative HKA angle, while no correlation was found between postoperative HKA angle and LDFA. Among the three groups classified by postoperative HKA angle, significant differences were found in aHKA, MPTA, and preoperative HKA angle, while no significant difference was found in LDFA and the amount of distal femoral and tibial osteotomies.
Conclusions
aHKA was correlated with postoperative HKA angle after medial fixed-bearing UKA, which was probably due to the influence of MPTA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medial unicompartmental knee arthroplasty (UKA) is an effective treatment for isolated medial osteoarthritis (OA) or osteonecrosis (ON) of the medial femoral condyle [1], yielding successful functional outcomes, high satisfaction rates, and a fast recovery after surgery [2,3,4,5,6,7]. Also, it has been suggested that patients undergoing UKA have fewer complications than patients who underwent total knee arthroplasty (TKA) [8, 9], and it has previously been reported that UKA is a more suitable technique for Asian patients than TKA, as their lifestyle requires deep knee flexion [10].
However, some past studies have reported higher revision risk in UKA compared to TKA [11,12,13,14], and malalignment of the lower limb alignment has been identified as the major contributing factor to high revision rate, poor clinical outcomes, and early polyethylene wear [15, 16]. Mild under-correction is considered to be acceptable, while a consequence of excessive residual varus alignment is increased compartment force by overloading medially, which can lead to failure due to polyethylene wear [16,17,18,19]. On the contrary, overcorrection of the coronal alignment may result in degeneration of the lateral compartment and lead to premature loosening of the prosthesis [17, 18]. Therefore, a reproducible method of predicting postoperative coronal alignment is desired to assume the risk of postoperative coronal malalignment. However, only a few studies have reported the risk factors of postoperative coronal malalignment in UKA [20, 21].
Recently, a new morphological assessment method, the arithmetic hip-knee-ankle angle (aHKA), has attracted attention as a method of assessing lower limb morphology while the mechanical hip-knee-ankle angle has been used to assess coronal alignment traditionally [22]. To calculate aHKA, lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA) are measured separately using long-leg radiographs, and an arithmetic method is subsequently used. aHKA is predictive of the patient’s constitutional knee alignment when comparing arthritic to non-arthritic patients [22]. Because aHKA uses only bony landmarks and is independent of the relationship of the femur to the tibia, it is not affected by joint space narrowing. At the same time, aHKA is not affected by whether the patient is standing or lying down at the time of imaging, so it is expected to have fewer measurement errors between patients.
The purpose of this study is to clarify the relationship between aHKA and postoperative coronal alignment after medial fixed-bearing UKA. We hypothesized that preoperative aHKA is correlated with postoperative HKA angle after medial fixed-bearing UKA.
Materials and methods
The hospital ethics committee approved the study protocol (No. 1510, Date of Approval: 02 Dec 2013) of this study. One hundred and one consecutive patients (125 knees) underwent medial fixed-bearing UKA using the Persona Partial Knee System (Zimmer Biomet Inc., Warsaw, IN, USA) and informed consent was obtained from all the patients, and the obtained data were retrospectively collected and analyzed. The inclusion criteria for UKA were a radiographic diagnosis of isolated end-stage (Kellgren-Lawrence grade 4) medial compartment OA or ON with an active ROM of ≥ 90°, a fixed flexion deformity of ≤ 15°, and a varus deformity of ≤ 10°. Of ON, those with end-stage OA in the background were treated as OA. Magnetic resonance imaging was performed for all the cases before surgery and the cases without the intact anterior cruciate ligament and articular surface of the lateral compartment were treated with TKA, not UKA. All the 125 UKAs were included in the study. Senior two surgeons with > 15 years of experience performed the surgery.
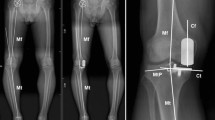
After inflating the tourniquet to 250 mmHg, a limited-medial parapatellar approach was performed. Following the macroscopic observation of an intact articular surface of the lateral as well as patellofemoral compartments, the minimal soft tissue release of the medial structures and osteophyte removal were performed. A proximal tibial osteotomy was then performed using an accelerometer-based portable navigation system (OrthAlign Plus®, UniAlign™; OrthAlign Inc., Aliso Viejo, CA, USA), which helps the surgeon to precisely perform tibial bone cut in UKA with coronal and sagittal alignment. It provides a measurement accuracy of ± 0.5° when measuring the angle between the OrthAlign Plus® unit and the reference sensor (manufacturer’s data). The target value of preoperative planning in coronal alignment was set to neutral (0°) in varus. Sagittal alignment was set regarding the original posterior tibial slope, which was measured with reference to the perpendicular line of the sagittal axis. The tibial sagittal axis was defined as the line connecting the anterior one-third of the medial tibial plateau and midpoints of the tibial plafond. The sagittal alignment was set to 6.0° and 8.0° when the angle was ≤ 6.0° and ≥ 8.0°, respectively, and the target value was set as the target value of preoperative planning when the angle was between 6.0° and 8.0° as in previous studies [23, 24]. The target osteotomy volume of the tibia (excluding the thickness of the bone saw blade) was set to 4 mm using a special stylus in all the cases. Following the tibial osteotomy, a distal femoral osteotomy was performed with the spacer block technique referring to the surface of the proximal tibial cut. The femoral rotation was carefully adjusted to the mechanical axis of the tibia, and the remaining (posterior and chamfer part) osteotomies of the femur were performed. The thickness of the tibial and femoral bone cut was measured using a calliper and the actual osteotomies were calculated by adding the thickness of the bone saw blades (1.27 mm). Pre- and postoperative coronal HKA angles, LDFA, and MPTA were measured based on long-leg standing radiographs (Fig. 1). LDFA was measured as the lateral angle formed by the mechanical axis of the femur and a line drawn across the articular surface of the distal femur at the most distal points of the lateral and medial femoral condyles. MPTA was measured as the angle formed medially by the mechanical axis of the tibia and a line drawn between the most distal articular contours of the midpoints of the lateral and medial plateaus. aHKA was calculated as 180° − LDFA + MPTA (Fig. 2). Two examples of actual aHKA calculation are given to advance understanding using preoperative long-leg standing radiographs. Case 1 (Fig. 3a, 3b): LDFA is 88.1° and MPTA is 83.3°. aHKA is calculated as 180° − LDFA (°) + MPTA (°) = 175.2°. Postoperative HKA angle is 175.7°. Case 2 (Fig. 3c, 3d): LDFA is 89.2° and MPTA is 87.4°. aHKA is calculated as 180° − LDFA (°) + MPTA (°) = 178.2°. Postoperative HKA angle is 178.4°.
Preoperative long-leg standing radiographs in two cases to illustrate the calculation of aHKA. a Case 1: LDFA is 88.1° and MPTA is 83.3°. aHKA is calculated as 180° − LDFA (°) + MPTA (°) = 175.2°. b Case 1: postoperative HKA angle is 175.7°. c Case 2: LDFA is 89.2° and MPTA is 87.4°. aHKA is calculated as 180° − LDFA (°) + MPTA (°) = 178.2°. d Case 2: postoperative HKA angle is 178.4°
The data are expressed as means ± standard deviations. To determine the intra-observer and inter-observer reliability of the measurements of LDFA, MPTA, and HKA angle, two investigators assessed the first ten patients twice and calculated intra-class correlation coefficients (ICCs). The ICCs for intra-observer reliability were > 0.84 (range 0.84–1.00) and those for inter-observer reliability were > 0.82 (range 0.82–0.96) for all measurements. Correlations between postoperative HKA angle and aHKA, LDFA, and MPTA were investigated by single regression analysis. Also, patients were divided into three groups according to the postoperative HKA angle, i.e., group valgus (HKA angle > 180°), group mild varus (175° < HKA angle ≤ 180°), and group severe varus (HKA angle ≤ 175°). The Tukey–Kramer test was utilized to compare aHKA, LDFA, MPTA, preoperative HKA angle, the thickness of the distal femoral bone cut, and the thickness of the tibial bone cut among the three groups. Data analyses were performed using BellCurve for Excel (Social Survey Research Information Co., Ltd., Tokyo, Japan). The sample size calculation was performed using G*Power 3 (Heinrich Heine Universität Düsseldorf, Germany). Based on our calculations, a minimum sample size of 89 patients was required for the single regression analysis with an effect size f2 of 0.15, a type I error (α) of 0.05, and a power (1 − β) of 0.95. Statistical significance was considered at P < 0.05.
Results
A total of 125 knees in 101 patients were enrolled in the study. The mean ± SD of age was 74.04 ± 8.1 years (range 51–89 years). Of all cases, 39 (31.2%) were male, and 86 (68.8%) were female; 59 (47.2%) had surgery on the left knee, and the others (66 (52.8%) were on the right knee; 106 (84.8%) were diagnosed as OA, and 19 (15.2%) were diagnosed as ON (Table 1). The mean ± SD of radiological parameters (including preoperative and postoperative HKA angle, LDFA, MPTA, and aHKA), the amount of distal femoral osteotomy, and the amount of tibial osteotomy are presented in Table 1. Of the 125 knees included in our study, 24 knees, 77 knees, and 24 knees were classified as group valgus, group mild varus, and group severe varus, respectively.
As for the correlation analyses between postoperative HKA angle and aHKA, LDFA, or MPTA, aHKA (R2 = 0.5003) and MPTA (R2 = 0.4092) were positively correlated with postoperative HKA angle (P < 0.001), while no correlation was found between postoperative HKA angle and LDFA (Fig. 4). In comparisons between the three groups classified according to the postoperative HKA angle, i.e., group valgus, group mild varus, and group severe varus, significant differences were found among the three groups in aHKA, MPTA, and preoperative HKA angle, while no significant difference was found among the three groups in LDFA (Fig. 5), which were consistent with the results from the correlation analyses. Regarding the amount of distal femoral osteotomy, no significant difference was found among the three groups, and the same was true with regard to the amount of tibial osteotomy (Fig. 6).
a Correlation analysis between aHKA and postoperative HKA angle. The aHKA was positively correlated with the postoperative HKA angle. b Correlation analysis between LDFA and postoperative HKA angle. No correlation was found between the two measurements. c Correlation analysis between MPTA and postoperative HKA angle. MPTA was positively correlated with the postoperative HKA angle
a Mean and the standard deviation of aHKA for each postoperative HKA angle group. Significant differences were found between each of the three groups (P < 0.01). b Mean and the standard deviation of LDFA for each postoperative HKA angle group. No significant difference was found among the three groups. c Mean and the standard deviation of MPTA for each postoperative HKA angle group. Significant differences were found between each of the three groups (P < 0.01). d Mean and the standard deviation of the preoperative HKA angle for each postoperative HKA angle group. Significant differences were found between each of the three groups (P < 0.01)
a Mean and the standard deviation of the amount of distal femoral osteotomy for each postoperative HKA angle group. No significant difference was found among the three groups. b Mean and the standard deviation of the amount of tibial osteotomy for each postoperative HKA angle group. No significant difference was found among the three groups
Discussion
The main finding of this study was that the aHKA was positively correlated with postoperative HKA angle (R2 = 0.5003) (Fig. 4a), and analysis of each element of aHKA showed that MPTA was positively correlated with postoperative HKA angle (R2 = 0.4092) (Fig. 4c) while no correlation was found between LDFA and postoperative HKA angle (Fig. 4b). Similar results were obtained when the cases were compared by dividing them into three groups by postoperative HKA angle (Fig. 5a–c). Overall, the preliminary hypothesis was proved to be correct. Specific examples show that case 1 (Fig. 3a; 175.2°) has aHKA smaller than case 2 (Fig. 3c; 178.2°), and case 1 (Fig. 3b; 175.7°) is also smaller than case 2 (Fig. 3d; 178.4°) in terms of postoperative HKA angle, which is in line with the trend shown in this study.
Also, many of the cases were end-stage medial compartment OA (Kellgren-Lawrence grade 4) and the medial joint space was considered to have almost disappeared, which was assumed to be a factor in the significant association between pre- and postoperative HKA angle (Fig. 5d). Also, just to be sure, the amount of osteotomy in each group was compared, but there was no significant difference, indicating that the present results were not due to the effect of the amount of osteotomy (Fig. 6). The current study first explored the relationship between aHKA and postoperative HKA in fixed-bearing UKA.
UKA is essentially only a resurfacing procedure and the osteotomy angle does not cause alignment changes. Given the lack of influence of the osteotomy volume on the results, the original bone morphology, i.e., aHKA, is considered to be directly reflected in the postoperative HKA angle. Liu et al. showed that aHKA was correlated with the HKA angle after mobile-bearing UKA and a high aHKA (> 180°) would increase the risk of postoperative valgus malalignment. They concluded that in patients with preoperative aHKA > 180°, mobile-bearing UKA should be conducted with caution [25]. The present study showed the same to be true for fixed-bearing UKA with the spacer block technique, and in addition, aHKA was shown to be a useful indicator of the risk of excessive postoperative varus malalignment.
aHKA has attracted attention in recent years as a method of assessing bone morphology in the lower limb with the rising interest in kinematic techniques in TKA, which aims to restore pre-arthritic alignment [26], as it is based on a practical, straightforward method for estimating constitutional lower limb alignment after the development of arthritic deformity. LDFA and MPTA do not change in the process of joint space narrowing in the absence of significant bone loss. In other words, the calculation of the aHKA is not affected by joint space narrowing or tibiofemoral subluxation and is independent of the joint line convergence angle, which has been shown in a past study [27]. In this study, HKA angle, LDFA, and MPTA were measured using long-leg standing radiographs, which have been reported to show a good correlation with those measured by CT, and the use of long-leg standing radiographs was considered to be acceptable because of its simplicity [28]. In UKA, aHKA has recently been used to assess lower limb alignment. Plancher et al. investigated if pre-arthritic/kinematic alignment of knees results in sustained long-term restoration of function, without conversion to TKA, following 150 fixed-bearing medial UKAs at an average of ten years after surgery. As a result, patients with compared to those without pre-arthritic/kinematically aligned knees had significantly longer mean survival and higher KOOS Activities of Daily Living and Sport subscale scores [29]. Bayoumi et al. assessed whether patients with pre-arthritically aligned knees demonstrated better mid-term outcomes and survivorship compared to patients with non-pre-arthritically aligned knees following medial fixed-bearing UKA using aHKA algorithm. As a result, pre-arthritically aligned knees and knees with relative overcorrection from their pre-arthritic alignment following UKA demonstrated better mid-term outcomes and survivorship than knees with relative under-correction from their pre-arthritic alignment [30].
Although UKA is a successful procedure for medial OA and ON, failures still exist in patients undergoing UKA, and lateral OA progression is one of the major complications that lead to conversion to TKA [31, 32]. Valgus malalignment, i.e., overcorrection of the lower limb alignment following UKA, is one of the most common reasons for the progression of lateral OA [33, 34]. For example, a past study found that patients with progressive lateral OA had valgus malalignment after UKA in a cohort of 3351 knees with a minimum follow-up of ten years [34]. It is therefore very important to find out the risk factors of postoperative valgus malalignment and proactively avoid them. Conversely, problems have also been reported for varus malalignment after UKA. Slaven et al. reported that when 61 revision cases for loosening after medial fixed-bearing UKAs were compared with 61 matched clinical success UKAs, the loosening group showed the mean HKA angle was 6.1° ± 3.1° of varus while the matched success group showed the mean HKA angle was 4.0° ± 2.7° of varus (P < 0.001) [35]. Also, Foissey et al. described patients with joint line lowering and postoperative varus malalignment were at high risk of tibial implant failure in 366 UKAs with a mean follow-up period of 61.3 months [36]. Given these, in medial fixed-bearing UKA with the use of the spacer block technique referring to the surface of the proximal tibial cut, it may be necessary to increase or decrease the amount of tibial osteotomy depending on the preoperative aHKA and consider the thickness of the insert used to maintain proper postoperative alignment.
This study had some limitations. Firstly, we assessed the relationship between the postoperative HKA angle and a new morphological indicator (aHKA) while we did not investigate the impact of lower-leg alignment after UKA. Therefore, further long-term follow-up of patients is required to clarify the relationship between postoperative alignment and clinical outcomes including patient-reported outcome measurements. Secondly, radiographic measurements, including pre- and postoperative HKA angle, LDFA, and MPTA, were still affected by the rotation of lower extremity and osteophyte formation while both the intra-observer and inter-observer agreements for these measurements were well within acceptable limits. Lastly, this study was a retrospective analysis involving fixed-bearing medial UKA with the spacer block technique only. Therefore, it is unclear if the current results are applicable for the mobile-bearing medial UKA or the fixed-bearing medial UKA with the use of other surgical techniques, e.g., the intramedullary rod method.
Conclusions
aHKA was correlated with postoperative HKA angle after medial fixed-bearing UKA, and it was assumed to be mainly due to the influence of MPTA. aHKA, an indicator of bony nature unaffected by loading or joint space narrowing, was considered useful in predicting the occurrence of postoperative coronal malalignment after UKA.
Data availability
Authors can confirm that all relevant data are included in the article.
References
Wilson HA, Middleton R, Abram SGF et al (2019) Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ 364:l352
Bayoumi T, van der List JP, Ruderman LV, Zuiderbaan HA, Kerkhoffs GMMJ, Pearle AD (2023) Successful same-day discharge in 88% of patients after unicompartmental knee arthroplasty: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 31(3):946–962
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 97-B(6):793–801
Mittal A, Meshram P, Kim WH, Kim TK (2020) Unicompartmental knee arthroplasty, an enigma, and the ten enigmas of medial UKA. J Orthop Traumatol 21(1):15
Ge J, Liu C, Sun X, Zhang Q, Ji B, Guo W (2023) Gap balance difference of unicompartmental knee arthroplasty between hanging leg and supine leg position: a prospective cohort study. Int Orthop 47(3):745–753
Foissey C, Batailler C, Vahabi A, Fontalis A, Servien E, Lustig S (2023) Better accuracy and implant survival in medial imageless robotic-assisted unicompartmental knee arthroplasty compared to conventional unicompartmental knee arthroplasty: two- to eleven-year follow-up of three hundred fifty-six consecutive knees. Int Orthop 47(2):533–541
Favroul C, Batailler C, Canetti R et al (2023) Image-based robotic unicompartmental knee arthroplasty allowed to match the rotation of the tibial implant with the native kinematic knee alignment. Int Orthop 47(2):519–526
Goh GS, Bin AbdRazak HR, Tay DK, Chia SL, Lo NN, Yeo SJ (2018) Unicompartmental knee arthroplasty achieves greater flexion with no difference in functional outcome, quality of life, and satisfaction vs total knee arthroplasty in patients younger than 55 years. A propensity score-matched cohort analysis. J Arthroplasty 33(2):355–361
Mortazavi SMJ, Vosoughi F (2022) Association of alignment variables, posteromedial tibial cartilage wear and anterior cruciate ligament insufficiency in participants with varus knee osteoarthritis: a cross-sectional study. Int Orthop 46(5):1029–1036
Kim MS, Koh IJ, Choi YJ, Lee JY, In Y (2017) Differences in patient-reported outcomes between unicompartmental and total knee arthroplasties: a propensity score-matched analysis. J Arthroplasty 32(5):1453–1459
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2018) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(6):1811–1822
Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD (2017) Annual revision rates of partial versus total knee arthroplasty: a comparative meta-analysis. Knee 24(2):179–190
Ellis RT, Nettrour JF, Keeney JA (2021) TKA is more durable than UKA for morbidly obese patients: a two-year minimum follow-up study. J Arthroplasty 36(6):1933–1941
Andronic O, Helmy N, Kellner C, Graf DA (2023) A decreased tibial tuberosity-trochlear groove distance is associated with lateral patellofemoral joint degeneration after implantation of medial fixed-bearing unicompartmental knee arthroplasty — a minimum five year follow-up. Int Orthop 47(9):2225–2233
Bae JH, Kim JG, Lee SY, Lim HC, In Y, MUKA Study group (2020) Epidemiology of bearing dislocations after mobile-bearing unicompartmental knee arthroplasty: multicenter analysis of 67 bearing dislocations. J Arthroplasty 35(1):265–271
van der List JP, Zuiderbaan HA, Pearle AD (2016) Why do medial unicompartmental knee arthroplasties fail today? J Arthroplasty 31(5):1016–1021
Ko YB, Gujarathi MR, Oh KJ (2015) Outcome of unicompartmental knee arthroplasty: a systematic review of comparative studies between fixed and mobile bearings focusing on complications. Knee Surg Relat Res 27(3):141–148
Chen H, Liu C, Mulatibieke Y, Zhang Q, Guo W (2023) The impact of preoperative MRI-detected lateral meniscal intra-substance signal abnormalities on mid-term functional outcomes following mobile-bearing unicompartmental knee arthroplasty. Int Orthop 47(10):2467–2475
Vasso M, Del Regno C, D’Amelio A, Viggiano D, Corona K, Schiavone Panni A (2015) Minor varus alignment provides better results than neutral alignment in medial UKA. Knee 22(2):117–121
Ahn JH, Kang HW, Yang TY, Lee JY (2016) Risk factors of post-operative malalignment in fixed-bearing medial unicompartmental knee arthroplasty. Int Orthop 40(7):1455–1463
Ishibashi K, Sasaki E, Otsuka H, Kazushige K, Yamamoto Y, Ishibashi Y (2020) Valgus correctability and meniscal extrusion were associated with alignment after unicompartmental knee arthroplasty. Clin Orthop Relat Res 478(7):1636–1644
Griffiths-Jones W, Chen DB, Harris IA, Bellemans J, MacDessi SJ (2021) Arithmetic hip-knee-ankle angle (aHKA): an algorithm for estimating constitutional lower limb alignment in the arthritic patient population. Bone Jt Open 2(5):351–358
Nakano N, Takayama K, Kuroda Y et al (2021) Preoperative varus deformity of the knee affects the intraoperative joint gap in unicompartmental knee arthroplasty. Knee 32:90–96
Suda Y, Takayama K, Ishida K et al (2020) Improved implant alignment accuracy with an accelerometer-based portable navigation system in medial unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28(9):2917–2923
Liu C, Chen H, Ge J, Huang C, Zhang Q, Guo W (2023) Predicting valgus malalignment after mobile-bearing UKA using a new method: the arithmetic HKA of the arthritic knee. Arch Orthop Trauma Surg 143(10):6381–6391
Hutt J, Massé V, Lavigne M, Vendittoli PA (2016) Functional joint line obliquity after kinematic total knee arthroplasty. Int Orthop 40(1):29–34
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470(1):45–53
Gieroba TJ, Marasco S, Babazadeh S, Di Bella C, van Bavel D (2023) Arithmetic hip knee angle measurement on long leg radiograph versus computed tomography-inter-observer and intra-observer reliability. Arthroplasty 5(1):35
Plancher KD, Brite JE, Briggs KK, Petterson SC (2022) Pre-arthritic/kinematic alignment in fixed-bearing medial unicompartmental knee arthroplasty results in return to activity at mean 10-year follow-up. J Bone Joint Surg Am 104(12):1081–1089
Bayoumi T, Burger JA, Ruderman LV et al (2023) Restoration or relative overcorrection of pre-arthritic coronal alignment leads to improved results following medial unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 31(9):3981–3991
El-Galaly A, Kappel A, Nielsen PT, Jensen SL (2019) Revision risk for total knee arthroplasty converted from medial unicompartmental knee arthroplasty: comparison with primary and revision arthroplasties, based on mid-term results from the Danish Knee Arthroplasty Registry. J Bone Joint Surg Am 101(22):1999–2006
Kazarian GS, Barrack TN, Okafor L, Barrack RL, Nunley RM, Lawrie CM (2020) High prevalence of radiographic outliers and revisions with unicompartmental knee arthroplasty. J Bone Joint Surg Am 102(13):1151–1159
Kang KT, Son J, Baek C, Kwon OR, Koh YG (2018) Femoral component alignment in unicompartmental knee arthroplasty leads to biomechanical change in contact stress and collateral ligament force in knee joint. Arch Orthop Trauma Surg 138(4):563–572
Slaven SE, Cody JP, Sershon RA, Ho H, Hopper RH Jr, Fricka KB (2021) Alignment in medial fixed-bearing unicompartmental knee arthroplasty: the limb has a leg up on the component. J Arthroplasty 36(12):3883–3887
Slaven SE, Cody JP, Sershon RA, Ho H, Hopper RH Jr, Fricka KB (2020) The impact of coronal alignment on revision in medial fixed-bearing unicompartmental knee arthroplasty. J Arthroplasty 35(2):353–357
Foissey C, Batailler C, Vahabi A, Fontalis A, Servien E, Lustig S (2023) Combination of a high residual varus and joint-line lowering strongly increases the risk of early implant failure in medial unicompartmental knee arthroplasty. J Arthroplasty 38(11):2275–2281
Funding
Open Access funding provided by Kobe University. This work was supported by Takeda Science Foundation.
Author information
Authors and Affiliations
Contributions
NN: conceptualization, formal analysis, investigation, methodology, validation, writing original draft, writing review and editing.
MT: formal analysis, investigation, writing review and editing.
TK: formal analysis, investigation, writing review and editing.
YK: formal analysis, investigation, writing review and editing.
KI: investigation, validation.
SH: investigation, validation.
RK: supervision, writing review and editing.
TM: conceptualization, supervision, writing review and editing.
Corresponding author
Ethics declarations
Ethics approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Written informed consent was obtained from all patients.
Consent to publish
Written informed consent was obtained from all patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakano, N., Tsubosaka, M., Kamenaga, T. et al. Predicting postoperative coronal alignment after fixed-bearing unicompartmental knee arthroplasty using a new morphological assessment method: the arithmetic hip-knee-ankle angle. International Orthopaedics (SICOT) 48, 889–897 (2024). https://doi.org/10.1007/s00264-023-06072-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-06072-6