Abstract
Purpose
There were fewer data to guide the application of enhanced recovery after surgery (ERAS) theory into sacral tumour surgery. In the present study, we were aiming to describe a multidisciplinary program of ERAS and evaluate the availability in sacral tumour surgery.
Methods
This was a prospective study of patients with sacral tumour between March 2021 and September 2021 at a single centre. We proposed a multidisciplinary program of ERAS for pre-admission, preoperative, intraoperative, postoperative, and post-discharge clinical care which positively influenced outcomes of patients with sacral tumour. All patients were prospectively assigned into two groups, ERAS group in which patients received ERAS protocols (n = 63), No-ERAS group in which patients had conventional clinical pathways (n = 62). Patient data were collected which included demographics, preoperative preparation, detailed information of surgical procedure, 60-day reoperation rate, 60-day readmission, postoperative length of stay (PLOS), time to first ambulation and flatus after surgery, time to removal of last drainage tube, and visual analogue scale (VAS) score at first ambulation and discharge. Complications referred to ones that occurred within 60 days after surgery. The above parameters were compared between ERAS group and No-ERAS group.
Results
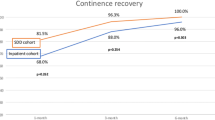
Time to first ambulation after surgery in ERAS group (mean 20.9 h) was significantly shorter than that in No-ERAS group (mean 104.3 ho). Meanwhile, time to first flatus after surgery in ERAS group (mean 26.7 h) was also significantly shorter than that in No-ERAS group (mean 37.3 h). Patients in ERAS group had statistically shorter PLOS (10.7 days) as compared to that in No-ERAS group (13.8 days). In ERAS group, 19 of 63 patients (30.2%) were discharged within seven days after surgery as compared to seven of 62 patients (11.3%) in No-ERAS group. VAS score at first ambulation in ERAS group was not obviously higher than that in No-ERAS group though the time of first ambulation in ERAS group was statistically earlier than one in No-ERAS group. Furthermore, VAS score at discharge in ERAS group was significantly lower than that in No-ERAS group. The rate of postoperative incision necrosis was 6.3% (4/63) in ERAS group and 8.1% (5/62) in No-ERAS group and all of these nine patients underwent reoperation before discharge. The difference was not statistically significant in the wound complication of incision necrosis and 60-day reoperation rate. Only one readmission occurred in No-ERAS group due to the surgical site infection and also there was no significant difference of 60-day readmission rate between these two groups. Furthermore, there was no statistical difference of complications of femoral artery thrombosis and rectal rupture between ERAS group and No-ERAS group.
Conclusions
Our proposed ERAS pathway for sacral tumour surgery and early walking facilitate safe and prompt discharge. ERAS protocols of sacral tumour surgery could decrease PLOS without significantly increasing postoperative complications, 60-day readmission rate and 60-day reoperation rate. The application of ERAS pathway in the field of sacral tumour surgery should have personalized feature with regard to resection type.











Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78:606–617
Chen KK, Chan JJ, Zubizarreta NJ et al (2021) Enhanced recovery after surgery protocols in lower extremity joint arthroplasty: using observational data to identify the optimal combination of components. J Arthroplast 36:2722–2728
Ding ZC, Xu B, Liang ZM et al (2020) Limited influence of comorbidities on length of stay after total hip arthroplasty: experience of enhanced recovery after surgery. Orthop Surg 12:153–161
Frassanito L, Vergari A, Nestorini R et al (2020) Enhanced recovery after surgery (ERAS) in hip and knee replacement surgery: description of a multidisciplinary program to improve management of the patients undergoing major orthopedic surgery. Musculoskelet Surg 104:87–92
Garg B, Mehta N, Bansal T et al (2021) Design and implementation of an enhanced recovery after surgery protocol in elective lumbar spine fusion by posterior approach: a retrospective, comparative study. Spine 46:E679–E687
Garin C (2020) Enhanced recovery after surgery in pediatric orthopedics (ERAS-PO). Orthop Traumatol Surg Res 106:S101–S107
Jayakumar P, Di JN, Fu JY et al (2017) A patient-focused technology-enabled program improves outcomes in primary total hip and knee replacement surgery. JBJS Open Access 2:e0023
Wang J, Du Z, Yang R et al (2020) Primary aneurysmal bone cyst of sacrum for adolescent: eleven cases experience and literature review. J Clin Neurosci 82:93–98
Wang J, Li D, Yang R et al (2020) Epidemiological characteristics of 1385 primary sacral tumors in one institution in China. World J Surg Oncol 18:297
Guo W, Tang X, Zang J et al (2013) One-stage total en bloc sacrectomy: a novel technique and report of 9 cases. Spine 38:E626–E631
Li D, Guo W, Qu H et al (2013) Experience with wound complications after surgery for sacral tumors. Eur Spine J 22:2069–2076
Li D, Guo W, Tang X et al (2011) Surgical classification of different types of en bloc resection for primary malignant sacral tumors. Eur Spine J 20:2275–2281
Li D, Guo W, Tang X et al (2014) Preservation of the contralateral sacral nerves during hemisacrectomy for sacral malignancies. Eur Spine J 23:1933–1939
Ji T, Guo W, Yang R et al (2017) What are the conditional survival and functional outcomes after surgical treatment of 115 patients with sacral chordoma? Clin Orthop Relat Res 475:620–630
Zhang Y, Guo W, Tang X et al (2018) Can aortic balloon occlusion reduce blood loss during resection of sacral tumors that extend into the lower lumber spine? Clin Orthop Relat Res 476:490–498
Huang L, Guo W, Yang R et al (2016) Proposed scoring system for evaluating neurologic deficit after sacral resection: functional outcomes of 170 consecutive patients. Spine 41:628–637
Zang J, Guo W, Yang RL et al (2015) Is total en bloc sacrectomy using a posterior-only approach feasible and safe for patients with malignant sacral tumors? J Neurosurg Spine 22:563–570
Gil JA, Goodman AD, Mulcahey MK (2018) Psychological factors affecting outcomes after elective shoulder surgery. J Am Acad Orthop Surg 26:e98–e104
Soffin EM, YaDeau JT (2016) Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth 117:iii62–iii72
Zang J, Guo W, Yang Y et al (2019) Surgical treatment of giant benign sacral neurogenic tumors using the posterior-only approach. Clin Neurol Neurosurg 185:105483
Wang J, Li D, Yang R et al (2020) Outcome of surgical treatment of children and adolescents with primary malignant sacral tumours. Int Orthop 44:1841–1851
Qi BC, Yu J, Qiao WS (2020) Comparison of intrathecal morphine versus local infiltration analgesia for pain control in total knee and hip arthroplasty: a meta-analysis. Medicine 99:e21971
Weibel S, Rucker G, Eberhart LH et al (2020) Drugs for preventing postoperative nausea and vomiting in adults after general anaesthesia: a network meta-analysis. Cochrane Database Syst Rev 10:CD012859
Stepan JG, London DA, Osei DA et al (2018) Perioperative celecoxib and postoperative opioid use in hand surgery: a prospective cohort study. J Hand Surg Am 43:346–353
Anderson PA, Savage JW, Vaccaro AR et al (2017) Prevention of surgical site infection in spine surgery. Neurosurgery 80:S114–S123
Markatos K, Kaseta M, Nikolaou VS (2015) Perioperative skin preparation and draping in modern total joint arthroplasty: current evidence. Surg Infect 16:221–225
Yuan S, Michaelsson K, Wan Z et al (2019) Associations of smoking and alcohol and coffee intake with fracture and bone mineral density: a Mendelian randomization study. Calcif Tissue Int 105:582–588
Burgess LC, Arundel J, Wainwright TW (2019) The effect of preoperative education on psychological, clinical and economic outcomes in elective spinal surgery: a systematic review. Healthcare (Basel) 7:48
Barberan-Garcia A, Ubre M, Roca J et al (2018) Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg 267:50–56
Debono B, Sabatier P, Boniface G et al (2021) Implementation of enhanced recovery after surgery (ERAS) protocol for anterior cervical discectomy and fusion: a propensity score-matched analysis. Eur Spine J 30:560–567
Koucheki R, Koyle M, Ibrahim GM et al (2021) Comparison of interventions and outcomes of enhanced recovery after surgery: a systematic review and meta-analysis of 2456 adolescent idiopathic scoliosis cases. Eur Spine J 30:3457–3472
Wei R, Guo W, Ji T et al (2017) One-step reconstruction with a 3D-printed, custom-made prosthesis after total en bloc sacrectomy: a technical note. Eur Spine J 26:1902–1909
Kushioka J, Yamashita T, Okuda S et al (2017) High-dose tranexamic acid reduces intraoperative and postoperative blood loss in posterior lumbar interbody fusion. J Neurosurg Spine 26:363–367
Drosos GI, Ververidis A, Valkanis C et al (2016) A randomized comparative study of topical versus intravenous tranexamic acid administration in enhanced recovery after surgery (ERAS) total knee replacement. J Orthop 13:127–131
Truntzer J, Comer G, Kendra M et al (2017) Perioperative smoking cessation and clinical care pathway for orthopaedic surgery. JBJS reviews 5:e11
Wang J, Du Z, Yang R et al (2020) Analysis of clinical outcome for adolescent patients undergoing conservative nerve-sparing surgery based on the proposed resection classification for sacral giant cell tumor. J Clin Neurosci 80:23–29
Kaczocha M, Azim S, Nicholson J et al (2018) Intrathecal morphine administration reduces postoperative pain and peripheral endocannabinoid levels in total knee arthroplasty patients: a randomized clinical trial. BMC Anesthesiol 18:27
Harsten A, Hjartarson H, Toksvig-Larsen S (2012) Total hip arthroplasty and perioperative oral carbohydrate treatment: a randomised, double-blind, controlled trial. Eur J Anaesthesiol 29:271–274
Yuan QM, Zhao ZH, Xu BS (2016) Efficacy and safety of tranexamic acid in reducing blood loss in scoliosis surgery: a systematic review and meta-analysis. Eur Spine J 26:131–139
Wei R, Guo W, Yang RL et al (2019) Reconstruction of the pelvic ring after total en bloc sacrectomy using a 3D-printed sacral endoprosthesis with re-establishment of spinopelvic stability: a retrospective comparative study. Bone Joint J 101:880–888
De Bie A, Siboni R, Smati MF et al (2020) Intrathecal morphine injections in lumbar fusion surgery: case-control study. Orthop Traumatol Surg Res 106:1187–1190
Pendi A, Acosta FL, Tuchman A et al (2017) Intrathecal morphine in spine surgery: A meta-analysis of randomized controlled trials. Spine 42:E740–E747
Tang B, Ji T, Guo W et al (2018) Which is the better timing between embolization and surgery for hypervascular spinal tumors, the same day or the next day?: a retrospective comparative study. Medicine 97:e10912
Pitchon DN, Dayan AC, Schwenk ES et al (2018) Updates on multimodal analgesia for orthopedic surgery. Anesthesiol Clin 36:361–373
Wang J, Du Z, Yang R et al (2021) Surgical strategy of pediatric benign sacral tumors. J Pediatr Orthop 41:227–235
Tang XD, Guo W, Yang RL et al (2010) Use of aortic balloon occlusion to decrease blood loss during sacral tumor resection. J Bone Joint Surg Am 92:1747–1753
Adeyemo EA, Aoun SG, Barrie U et al (2021) Enhanced recovery after surgery reduces postoperative opioid use and 90-day readmission rates after open thoracolumbar fusion for adult degenerative deformity. Neurosurgery 88:295–300
Garriga C, Murphy J, Leal J et al (2019) Impact of a national enhanced recovery after surgery programme on patient outcomes of primary total knee replacement: an interrupted time series analysis from “The National Joint Registry of England, Wales, Northern Ireland and the Isle of Man”. Osteoarthr Cartil 27:1280–1293
Soffin EM, Wetmore DS, Barber LA et al (2019) An enhanced recovery after surgery pathway: association with rapid discharge and minimal complications after anterior cervical spine surgery. Neurosurg Focus 46:E9
Soffin EM, Wetmore DS, Beckman JD et al (2019) Opioid-free anesthesia within an enhanced recovery after surgery pathway for minimally invasive lumbar spine surgery: a retrospective matched cohort study. Neurosurg Focus 46:E8
Auyong DB, Allen CJ, Pahang JA et al (2015) Reduced length of hospitalization in primary total knee arthroplasty patients using an updated enhanced recovery after orthopedic surgery (ERAS) pathway. J Arthroplast 30:1705–1709
Tang B, Ji T, Tang X et al (2015) Risk factors for major complications in surgery for hypervascular spinal tumors: an analysis of 120 cases with adjuvant preoperative embolization. Eur Spine J 24:2201–2208
Tang X, Yang R, Qu H et al (2018) Factors associated with spinopelvic fixation mechanical failure after total sacrectomy. Spine 43:1268–1274
Code availability
SPSS software during the current study is available from the corresponding author on reasonable request.
Funding
This work was supported by Natural Science Foundation of China (NO: 82272947), Peking University People’s Hospital Research and Development Funds (NO: RDG2021-02, RDL2022-14, RZ2023-02), and Clinical Medicine Plus X-Young Scholars Project, Peking University, the Fundamental Research Funds for the Central Universities (NO: PKU2023LCXQ016).
Author information
Authors and Affiliations
Contributions
JW (contribution: collect and analyze data and draft the article)
CC (contribution: collect data and take charge of preoperative SAE)
DL(contribution: collect and analyze data)
YY (contribution: collect and analyze data)
JX (contribution: collect data and take charge of anesthesia)
LZ (contribution: collect data and take charge of nursing)
FH (contribution: collect data and take charge of anesthesia)
WG (contribution: perform surgery and study design)
XT (contribution: perform surgery and study design)
Corresponding authors
Ethics declarations
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jun Wang and Chen Chen are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Chen, C., Li, D. et al. Enhanced recovery after surgery (ERAS) in sacral tumour surgery and comprehensive description of a multidisciplinary program: a prospective study in a specialized hospital in China. International Orthopaedics (SICOT) 48, 581–601 (2024). https://doi.org/10.1007/s00264-023-06016-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-06016-0