Abstract
Objective
The purpose of this systematic review and meta-analysis of randomized controlled trials (RCTs) and non-RCTs was to gather data to evaluate the efficacy and safety of tranexamic acid (TXA) versus placebo after a scoliosis surgery.
Methods
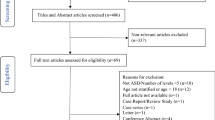
The electronic databases including Embase, PubMed, CENTRAL (Cochrane Controlled Trials Register), Web of Science, and Google database were searched to identify relevant studies published from the time of the establishment of these databases up to May 2016. This systematic review and meta-analysis was performed according to the PRISMA statement criteria. The primary outcomes were total blood loss, intraoperative blood loss, and hemoglobin after surgery. The second outcome is need for transfusion. Stata 12.0 software was used for the meta-analysis. After testing for publication bias and heterogeneity across studies, data were aggregated for random-effects modeling when necessary.
Results
A total of 685 patients (347 patients in the TXA group and 338 in the control group) were finally included for this meta-analysis. The pooled results revealed that administration of TXA can decrease the total blood loss after scoliosis surgery [mean difference (MD) = 682.30, 95% confidence interval (CI) −930.60 to −434.00; P = 0.000] and intraoperative blood loss [(MD) = −535.28; 95% CI −683.74 to −368.82; P = 0.000]. For the hemoglobin (Hb) value after scoliosis surgery, TXA can decrease the Hb value for 0.51 dL [(MD) = 0.51; 95% CI 0.25–0.78; P = 0.000]. There is no statistically significant difference between the TXA versus placebo in terms of the need for transfusion (relative risk = 0.55, 95% CI 0.25–1.20, P = 0.132).
Conclusion
Based on the current meta-analysis, TXA can decrease the total blood loss and intraoperative blood loss during scoliosis surgery. It is recommended that it be routinely used in scoliosis surgery. High-dose TXA (>20 mg/kg) is more effective than low-dose TXA (<20 mg/kg) in controlling blood loss. However, for the need for transfusion, more high-quality RCTs need to be identified.









Similar content being viewed by others
References
Shapiro F, Sethna N (2004) Blood loss in pediatric spine surgery. Eur Spine J 13(Suppl 1):S6–S17. doi:10.1007/s00586-004-0760-y
Guay J, Haig M, Lortie L, Guertin MC, Poitras B (1994) Predicting blood loss in surgery for idiopathic scoliosis. Can J Anaesth 41(9):775–781. doi:10.1007/BF03011583
Nuttall GA, Horlocker TT, Santrach PJ, Oliver WC Jr, Dekutoski MB, Bryant S (2000) Predictors of blood transfusions in spinal instrumentation and fusion surgery. Spine 25(5):596–601
Hur SR, Huizenga BA, Major M (1992) Acute normovolemic hemodilution combined with hypotensive anesthesia and other techniques to avoid homologous transfusion in spinal fusion surgery. Spine 17(8):867–873
Hu SS (2004) Blood loss in adult spinal surgery. Eur Spine J 13(1):S3–S5. doi:10.1007/s00586-004-0753-x
Madjdpour C, Spahn D (2005) Allogeneic red blood cell transfusions: efficacy, risks, alternatives and indications. Br J Anaesth 95(1):33–42. doi:10.1093/bja/aeh290
Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB (1999) An analysis of blood management in patients having a total hip or knee arthroplasty*. J Bone Jt Surg Am 81(1):2–10
Cermakova Z, Simetka O, Kořístka M (2013) Transfusion-related acute lung injury (TRALI)-review. Ceska Gynekol 78(2):211–215
Dunn CJ, Goa KL (1999) Tranexamic acid: a review of its use in surgery and other indications. Drugs 57(6):1005–1032
Kang JS, Moon KH, Kim BS, Yang SJ (2016) Topical administration of tranexamic acid in hip arthroplasty. Int Orthop. doi:10.1007/s00264-016-3195-2 (Epub ahead of print)
Chen JY, Chin PL, Moo IH, Pang HN, Tay DK, Chia SL, Lo NN, Yeo SJ (2016) Intravenous versus intra-articular tranexamic acid in total knee arthroplasty: a double-blinded randomised controlled noninferiority trial. Knee 23(1):152–156. doi:10.1016/j.knee.2015.09.004
McHugh SM, Kolarczyk L, Lang RS, Wei LM, Jose M, Subramaniam K (2016) A comparison of high-dose and low-dose tranexamic acid antifibrinolytic protocols for primary coronary artery bypass surgery. Indian J Anaesth 60(2):94–101. doi:10.4103/0019-5049.176279
Berney MJ, Dawson PH, Phillips M, Lui DF, Connolly P (2015) Eliminating the use of allogeneic blood products in adolescent idiopathic scoliosis surgery. Eur J Orthop Surg Traumatol Orthop Traumatol 25(Suppl 1):S219–S223. doi:10.1007/s00590-015-1624-3
da Rocha VM, de Barros AG, Naves CD, Gomes NL, Lobo JC, Villela Schettino LC, da Silva LE (2015) Use of tranexamic acid for controlling bleeding in thoracolumbar scoliosis surgery with posterior instrumentation. Rev Bras Ortop 50(2):226–231. doi:10.1016/j.rboe.2015.03.007
Lykissas MG, Crawford AH, Chan G, Aronson LA, Al-Sayyad MJ (2013) The effect of tranexamic acid in blood loss and transfusion volume in adolescent idiopathic scoliosis surgery: a single-surgeon experience. J Child Orthop 7(3):245–249. doi:10.1007/s11832-013-0486-7
McLeod LM, French B, Flynn JM, Dormans JP, Keren R (2015) Antifibrinolytic use and blood transfusions in pediatric scoliosis surgeries performed at US Children’s Hospitals. J Spinal Disord Tech 28(8):E460–E466. doi:10.1097/BSD.0b013e3182a22a54
Neilipovitz DT, Murto K, Hall L, Barrowman NJ, Splinter WM (2001) A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg 93(1):82–87
Ng BK, Chau WW, Hung AL, Hui AC, Lam TP, Cheng JC (2015) Use of tranexamic acid (TXA) on reducing blood loss during scoliosis surgery in Chinese adolescents. Scoliosis 10:28. doi:10.1186/s13013-015-0052-9
Sethna NF, Zurakowski D, Brustowicz RM, Bacsik J, Sullivan LJ, Shapiro F (2005) Tranexamic acid reduces intraoperative blood loss in pediatric patients undergoing scoliosis surgery. Anesthesiology 102(4):727–732
Sui WY, Ye F, Yang JL (2016) Efficacy of tranexamic acid in reducing allogeneic blood products in adolescent idiopathic scoliosis surgery. BMC Musculoskelet Disord 17(1):187. doi:10.1186/s12891-016-1006-y
Verma K, Errico T, Diefenbach C, Hoelscher C, Peters A, Dryer J, Huncke T, Boenigk K, Lonner BS (2014) The relative efficacy of antifibrinolytics in adolescent idiopathic scoliosis: a prospective randomized trial. J Bone Jt Surg Am 96(10):e80. doi:10.2106/JBJS.L.00008
Xu C, Wu A, Yue Y (2012) Which is more effective in adolescent idiopathic scoliosis surgery: batroxobin, tranexamic acid or a combination? Arch Orthop Trauma Surg 132(1):25–31. doi:10.1007/s00402-011-1390-6
Yagi M, Hasegawa J, Nagoshi N, Iizuka S, Kaneko S, Fukuda K, Takemitsu M, Shioda M, Machida M (2012) Does the intraoperative tranexamic acid decrease operative blood loss during posterior spinal fusion for treatment of adolescent idiopathic scoliosis? Spine 37(21):E1336–E1342. doi:10.1097/BRS.0b013e318266b6e5
Chen S, Wu K, Kong G, Feng W, Deng Z, Wang H (2016) The efficacy of topical tranexamic acid in total hip arthroplasty: a meta-analysis. BMC Musculoskelet Disord 17(1):81. doi:10.1186/s12891-016-0923-0
North WT, Mehran N, Davis JJ, Silverton CD, Weir RM, Laker MW (2016) Topical vs intravenous tranexamic acid in primary total hip arthroplasty: a double-blind. Randomized controlled trial. J Arthroplasty 31(4):928–929. doi:10.1016/j.arth.2015.12.001
Xie J, Ma J, Yue C, Kang P, Pei F (2016) Combined use of intravenous and topical tranexamic acid following cementless total hip arthroplasty: a randomised clinical trial. Hip Int 26(1):36–42. doi:10.5301/hipint.5000291
Tzortzopoulou A, Cepeda MS, Schumann R, Carr DB (2008) Antifibrinolytic agents for reducing blood loss in scoliosis surgery in children. Cochrane Database Syst Rev 3:Cd006883. doi:10.1002/14651858.CD006883.pub2
Chimento GF, Huff T, Ochsner JL Jr, Meyer M, Brandner L, Babin S (2013) An evaluation of the use of topical tranexamic acid in total knee arthroplasty. J Arthroplasty 28(8 Suppl):74–77. doi:10.1016/j.arth.2013.06.037
Ortmann E, Besser MW, Klein AA (2013) Antifibrinolytic agents in current anaesthetic practice. Br J Anaesth 111(4):549–563. doi:10.1093/bja/aet154
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing interests exist.
Funding
The authors are grateful for the support by the National Natural Science Foundation of China (No. 81272046), and the Research Foundation of the Tianjin Health Bureau (No. 14KG121), the Research Foundation of the Tianjin Science and Technology Committee (No. 15JCYBJC25300). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Rights and permissions
About this article
Cite this article
Yuan, QM., Zhao, ZH. & Xu, BS. Efficacy and safety of tranexamic acid in reducing blood loss in scoliosis surgery: a systematic review and meta-analysis. Eur Spine J 26, 131–139 (2017). https://doi.org/10.1007/s00586-016-4899-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4899-0