Abstract
Purpose
Enhanced recovery after surgery (ERAS), still emerging for the spine, proposes a multimodal approach of perioperative care involving the optimization of every procedural step, with the patient in a proactive position regarding his/her management. We aimed to demonstrate a reduction in the length of hospital stay for ACDF without increasing the risk for patients by comparing 2 groups before and after ERAS implementation using propensity score (PS)-matched analysis.
Methods
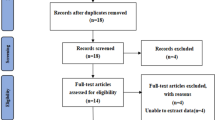
We selected 2 periods of 1 year, before (n = 268 patients) and after ERAS implementation (n = 271 patients). Data were collected on patient demographics, operative and perioperative details, 90-day readmissions and morbidity. ERAS-trained nurses were involved to support patients at each pre/per/postoperative step with the help of a mobile app. A satisfaction survey was included. PS analyses were used for dealing with confounding bias in this retrospective observational study.
Results
After PS matching, the outcomes of 202 well-balanced pairs of patients were compared (conventional vs ERAS). LOS was reduced from 2.96 ± 1.35 to 1.40 ± 0.6 days (Student, p < 0.001). All 90-day surgical morbidity was similar between the 2 groups, including 30-day readmission (0.5% vs 0%; p = 1), 30- to 90-day readmission (0.5% vs 0.0%; p = 1), 90-day reoperation (0% vs 1%; p = 0.49), major complications (3.0% vs 3.5%; p = 1) and minor complications (2.0% vs 3.5%; p = 0.54). There was no significant difference concerning the satisfaction survey.
Conclusions
The introduction of ERAS for ACDF in our institution has resulted in a significant decrease in LOS, without causing an increase in postoperative complications and has maintained patients’ satisfaction.

Similar content being viewed by others
References
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78:606–617. https://doi.org/10.1093/bja/78.5.606
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 248:189–198. https://doi.org/10.1097/SLA.0b013e31817f2c1a
Jones EL, Wainwright TW, Foster JD et al (2014) A systematic review of patient reported outcomes and patient experience in enhanced recovery after orthopaedic surgery. Ann R Coll Surg Engl 96:89–94. https://doi.org/10.1308/003588414X13824511649571
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152:292–298. https://doi.org/10.1001/jamasurg.2016.4952
Wainwright TW, Immins T, Middleton RG (2016) Enhanced recovery after surgery (ERAS) and its applicability for major spine surgery. Best Pract Res Clin Anaesthesiol 30:91–102. https://doi.org/10.1016/j.bpa.2015.11.001
Ali ZS, Ma TS, Ozturk AK et al (2017) Pre-optimization of spinal surgery patients: development of a neurosurgical enhanced recovery after surgery (ERAS) protocol. Clin Neurol Neurosurg 164:142–153. https://doi.org/10.1016/j.clineuro.2017.12.003
Adamson T, Godil SS, Mehrlich M et al (2016) Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. J Neurosurg Spine 24:878–884. https://doi.org/10.3171/2015.8.SPINE14284
Lied B, Sundseth J, Helseth E (2008) Immediate (0–6 h), early (6–72 h) and late (%3e72 h) complications after anterior cervical discectomy with fusion for cervical disc degeneration; discharge six hours after operation is feasible. Acta Neurochir (Wien) 150:111–118. https://doi.org/10.1007/s00701-007-1472-y (discussion 118)
Khanna R, Kim RB, Lam SK et al (2018) Comparing short-term complications of inpatient versus outpatient single-level anterior cervical discectomy and fusion: an analysis of 6940 patients using the ACS-NSQIP database. Clin Spine Surg 31:43. https://doi.org/10.1097/BSD.0000000000000499
McClelland S, Passias PG, Errico TJ et al (2017) Inpatient versus outpatient anterior cervical discectomy and fusion: a perioperative complication analysis of 259,414 patients from the healthcare cost and utilization project databases. Int J Spine Surg 11:11. https://doi.org/10.14444/4011
Mullins J, Pojskić M, Boop FA, Arnautović KI (2018) Retrospective single-surgeon study of 1123 consecutive cases of anterior cervical discectomy and fusion: a comparison of clinical outcome parameters, complication rates, and costs between outpatient and inpatient surgery groups, with a literature review. J Neurosurg Spine 28:630–641. https://doi.org/10.3171/2017.10.SPINE17938
Helseth Ø, Lied B, Halvorsen CM et al (2015) Outpatient cervical and lumbar spine surgery is feasible and safe: a consecutive single center series of 1449 patients. Neurosurgery 76:728–737. https://doi.org/10.1227/NEU.0000000000000746 (discussion 737–738)
McGirt MJ, Godil SS, Asher AL et al (2015) Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus 39:E9. https://doi.org/10.3171/2015.9.FOCUS15335
Indicateurs par spécialité|Stats ATIH. https://www.scansante.fr/applications/action-gdr-chirurgie-ambulatoire-spec. Accessed 3 Jan 2017
Wang MY (2010) Early complications related to anterior cervical surgery. World Neurosurg 74:272. https://doi.org/10.1016/j.wneu.2010.06.026
Arshi A, Wang C, Park HY et al (2017) Ambulatory anterior cervical discectomy and fusion is associated with a higher risk of revision surgery and perioperative complications: an analysis of a large nationwide database. Spine J. https://doi.org/10.1016/j.spinee.2017.11.012
Bovonratwet P, Webb ML, Ondeck NT et al (2018) Discrepancies in the definition of “outpatient” surgeries and their effect on study outcomes related to ACDF and lumbar discectomy procedures: a retrospective analysis of 45,204 cases. Clin Spine Surg. https://doi.org/10.1097/BSD.0000000000000615
Verrier J-F, Paget C, Perlier F, Demesmay F (2016) How to introduce a program of enhanced recovery after surgery? The experience of the CAPIO group. J Visc Surg 153:S33–S39. https://doi.org/10.1016/j.jviscsurg.2016.10.001
Lonjon G, Boutron I, Trinquart L et al (2014) Comparison of treatment effect estimates from prospective nonrandomized studies with propensity score analysis and randomized controlled trials of surgical procedures. Ann Surg 259:18–25. https://doi.org/10.1097/SLA.0000000000000256
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46:399–424. https://doi.org/10.1080/00273171.2011.568786
Debono B, Bousquet P, Sabatier P et al (2016) Postoperative monitoring with a mobile application after ambulatory lumbar discectomy: an effective tool for spine surgeons. Eur Spine J 25:3536–3542. https://doi.org/10.1007/s00586-016-4680-4
Rampersaud YR, Moro ERP, Neary MA et al (2006) Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine 31:1503–1510. https://doi.org/10.1097/01.brs.0000220652.39970.c2
Kehlet H, Thienpont E (2013) Fast-track knee arthroplasty—status and future challenges. Knee 20(Suppl 1):S29–33. https://doi.org/10.1016/S0968-0160(13)70006-1
Wang MY, Chang P-Y, Grossman J (2017) Development of an enhanced recovery after surgery (ERAS) approach for lumbar spinal fusion. J Neurosurg Spine 26:411–418. https://doi.org/10.3171/2016.9.SPINE16375
Venkata HK, van Dellen JR (2016) A perspective on the use of an enhanced recovery program in open, non-instrumented day surgery for degenerative lumbar and cervical spinal conditions. J Neurosurg Sci 62(3):245–254. https://doi.org/10.23736/S0390-5616.16.03695-X
Fu MC, Gruskay JA, Samuel AM et al (2017) Outpatient anterior cervical discectomy and fusion is associated with fewer short-term complications in one- and two-level cases: a propensity-adjusted analysis. Spine 42:1044–1049. https://doi.org/10.1097/BRS.0000000000001988
Debono B, Sabatier P, Garnault V et al (2017) Outpatient lumbar microdiscectomy in France: from an economic imperative to a clinical standard—an observational study of 201 cases. World Neurosurg 106:891–897. https://doi.org/10.1016/j.wneu.2017.07.065
Kehlet H, Delaney CP, Hill AG (2015) Perioperative medicine—the second round will need a change of tactics. Br J Anaesth 115:13–14. https://doi.org/10.1093/bja/aev098
Bradywood A, Farrokhi F, Williams B et al (2017) Reduction of inpatient hospital length of stay in lumbar fusion patients with implementation of an evidence-based clinical care pathway. Spine 42:169–176. https://doi.org/10.1097/BRS.0000000000001703
Debono B, Corniola MV, Pietton R et al (2019) Benefits of enhanced recovery after surgery for fusion in degenerative spine surgery: impact on outcome, length of stay, and patient satisfaction. Neurosurg Focus 46:E6. https://doi.org/10.3171/2019.1.FOCUS18669
Acknowledgements
The authors are grateful to Antoine Guillain for his collaboration with the preparation of the manuscript and for the organization of the phone survey.
Funding
No funds were received in support of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical approval
The manuscript submitted does not contain information about medical device(s)/drug(s).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Debono, B., Sabatier, P., Boniface, G. et al. Implementation of enhanced recovery after surgery (ERAS) protocol for anterior cervical discectomy and fusion: a propensity score-matched analysis. Eur Spine J 30, 560–567 (2021). https://doi.org/10.1007/s00586-020-06445-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06445-0