Abstract
Purpose
This study investigated the association of admission hyperglycaemia with catheter-associated urinary tract infections (CAUTIs) and catheter-unassociated urinary tract infections (CUUTIs) in elderly patients with hip fractures.
Methods
In an observational cohort study of elderly patients with hip fractures, glucose values were collected within 24 h of admission. Urinary tract infections were classified as CAUTIs and CUUTIs. Multivariate logistic regression analysis and propensity score matching obtained adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for urinary tract infections. Subgroup analyses were further explored to investigate the relationship between admission hyperglycemia and urinary tract infections.
Results
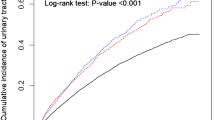
The study included 1279 elderly patients with hip fractures, 298 (23.3%) of whom had urinary tract infections upon hospitalization (including 182 CAUTIs and 116 CUUTIs). Propensity score matching indicated that patients with glucose levels exceeding 10.00 mmol/L had significantly higher odds of developing CAUTIs (OR 3.10, 95% CI 1.65–5.82) than those with glucose levels between 4.00–6.09 mmol/L. It is worth noting that patients with blood glucose levels greater than 10.00 mmol/L have a higher susceptibility for CUUTIs (OR 4.42, 95% CI 2.09–9.33) than CAUTIs. The subgroup analyses observed significant interactions between diabetes and CAUTIs (p for interaction = 0.01) and between bedridden time and CUUTIs (p for interaction = 0.04).
Conclusions
Elderly hip fracture patients with admission hyperglycaemia have an independent association with CAUTIs and CUUTIs. The association is stronger with CUUTIs and necessitates clinician intervention if blood glucose levels at admission exceed 10 mmol/L.




Similar content being viewed by others
References
Bliemel C, Buecking B, Hack J, Aigner R, Eschbach DA, Ruchholtz S, Oberkircher L (2017) Urinary tract infection in patients with hip fracture: An underestimated event? Geriatr Gerontol Int 17:2369–2375. https://doi.org/10.1111/ggi.13077
Rohold CK, Lauritzen JB, Jørgensen HL (2022) Causes of death among 93.637 hip fracture patients- data based on the Danish National Registry of causes of death. Eur J Trauma Emerg Surg 48:1861–1870. https://doi.org/10.1007/s00068-021-01791-0
Herruzo-Cabrera R, López-Giménez R, Cordero J, Munuera L (2001) Urinary infection after orthopedic procedures. Int Orthop 25:55–59. https://doi.org/10.1007/s002640000176
Chen YC, Chuang CH, Hsieh MH, Yeh HW, Yang SF, Lin CW, Yeh YT, Huang JY, Liao PL, Chan CH, Yeh CB (2021) Risk of Mortality and Readmission among Patients with Pelvic Fracture and Urinary Tract Infection: A Population-Based Cohort Study. Int J Environ Res Public Health 18(9):4868. https://doi.org/10.3390/ijerph18094868
Weber M, Cabanela ME, Sim FH, Frassica FJ, Harmsen WS (2002) Total hip replacement in patients with Parkinson’s disease. Int Orthop 26:66–68. https://doi.org/10.1007/s00264-001-0308-2
Saadat GH, Alsoof D, Ahmad B, Butler BA, Messer TA, Bokhari F (2022) Incidence, risk factors and clinical implications of postoperative urinary tract infection in geriatric hip fractures. Injury 53:2158–2162. https://doi.org/10.1016/j.injury.2022.03.012
Seyhan Ak E, Özbaş A (2018) The effect of education of nurses on preventing catheter-associated urinary tract infections in patients who undergo hip fracture surgery. J Clin Nurs 27:e1078–e1088. https://doi.org/10.1111/jocn.14160
Singh S, Angus LDG, Munnangi S, Shaikh D, Digiacomo JC, Angara VC, Brown A, Akadiri T (2021) Reducing Catheter-Associated Urinary Tract Infection: The Impact of Routine Screening in the Geriatric Hip Fracture Population. J Trauma Nurs 28:290–297. https://doi.org/10.1097/jtn.0000000000000603
Ma Y, Lu X (2019) Indwelling catheter can increase postoperative urinary tract infection and may not be required in total joint arthroplasty: a meta-analysis of randomized controlled trial. BMC Musculoskelet Disord 20:11. https://doi.org/10.1186/s12891-018-2395-x
Richards JE, Kauffmann RM, Obremskey WT, May AK (2013) Stress-induced hyperglycemia as a risk factor for surgical-site infection in nondiabetic orthopedic trauma patients admitted to the intensive care unit. J Orthop Trauma 27:16–21. https://doi.org/10.1097/BOT.0b013e31825d60e5
Talapko J, Meštrović T, Škrlec I (2022) Growing importance of urogenital candidiasis in individuals with diabetes: A narrative review. World J Diabetes 13:809–821. https://doi.org/10.4239/wjd.v13.i10.809
Murtha MJ, Eichler T, Bender K, Metheny J, Li B, Schwaderer AL, Mosquera C, James C, Schwartz L, Becknell B, Spencer JD (2018) Insulin receptor signaling regulates renal collecting duct and intercalated cell antibacterial defenses. J Clin Investig 128:5634–5646. https://doi.org/10.1172/jci98595
Nichols GA, Brodovicz KG, Kimes TM, Déruaz-Luyet A, Bartels DB (2017) Prevalence and incidence of urinary tract and genital infections among patients with and without type 2 diabetes. J Diabetes Complicat 31:1587–1591. https://doi.org/10.1016/j.jdiacomp.2017.07.018
Kamei J, Yamamoto S (2021) Complicated urinary tract infections with diabetes mellitus. J Infect Chemother 27:1131–1136. https://doi.org/10.1016/j.jiac.2021.05.012
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332. https://doi.org/10.1016/j.ajic.2008.03.002
Clarke K, Hall CL, Wiley Z, Tejedor SC, Kim JS, Reif L, Witt L, Jacob JT (2020) Catheter-Associated Urinary Tract Infections in Adults: Diagnosis, Treatment, and Prevention. J Hosp Med 15:552–556. https://doi.org/10.12788/jhm.3292
Hayati Rezvan P, Lee KJ, Simpson JA (2015) The rise of multiple imputation: a review of the reporting and implementation of the method in medical research. BMC Med Res Methodol 15:30. https://doi.org/10.1186/s12874-015-0022-1
Fu EL, Groenwold RHH, Zoccali C, Jager KJ, van Diepen M, Dekker FW (2019) Merits and caveats of propensity scores to adjust for confounding. Nephrol Dial Transplant 34:1629–1635. https://doi.org/10.1093/ndt/gfy283
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, Gabbay RA, on behalf of the American Diabetes A (2023) 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes care 46:S19-s40. https://doi.org/10.2337/dc23-S002
VanderWeele TJ, Mathur MB (2020) Commentary: Developing best-practice guidelines for the reporting of E-values. Int J Epidemiol 49:1495–1497. https://doi.org/10.1093/ije/dyaa094
Huang YW, Yin XS, Li ZP (2022) Association of the stress hyperglycemia ratio and clinical outcomes in patients with stroke: A systematic review and meta-analysis. Front Neurol 13:999536. https://doi.org/10.3389/fneur.2022.999536
Shanks AM, Woodrum DT, Kumar SS, Campbell DA Jr, Kheterpal S (2018) Intraoperative hyperglycemia is independently associated with infectious complications after non-cardiac surgery. BMC Anesthesiol 18:90. https://doi.org/10.1186/s12871-018-0546-0
Gofir A, Mulyono B, Sutarni S (2017) Hyperglycemia as a prognosis predictor of length of stay and functional outcomes in patients with acute ischemic stroke. Int J Neurosci 127:923–929. https://doi.org/10.1080/00207454.2017.1280793
Frisch A, Chandra P, Smiley D, Peng L, Rizzo M, Gatcliffe C, Hudson M, Mendoza J, Johnson R, Lin E, Umpierrez GE (2010) Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care 33:1783–1788. https://doi.org/10.2337/dc10-0304
Xie ZY, Bai H, Deng FF (2021) Relationship between Stress Hyperglycemia and Catheter-related Urinary Tract Infection in Stroke Patients. Zhongguo yi xue ke xue yuan xue bao Acta Academiae Medicinae Sinicae 43:188–192. https://doi.org/10.3881/j.issn.1000-503X.12916
McCowen KC, Malhotra A, Bistrian BR (2001) Stress-induced hyperglycemia. Crit Care Clin 17:107–124. https://doi.org/10.1016/s0749-0704(05)70154-8
Losser MR, Damoisel C, Payen D (2010) Bench-to-bedside review: Glucose and stress conditions in the intensive care unit. Crit Care (London, England) 14:231. https://doi.org/10.1186/cc9100
Karunakar MA, Staples KS (2010) Does stress-induced hyperglycemia increase the risk of perioperative infectious complications in orthopaedic trauma patients? J Orthop Trauma 24:752–756. https://doi.org/10.1097/BOT.0b013e3181d7aba5
Harrington D, D’Agostino RB Sr, Gatsonis C, Hogan JW, Hunter DJ, Normand ST, Drazen JM, Hamel MB (2019) New Guidelines for Statistical Reporting in the Journal. N Engl J Med 381:285–286. https://doi.org/10.1056/NEJMe1906559
Sun L, Liu Z, Wu H, Liu B, Zhao B (2023) Validation of the Nottingham Hip Fracture Score in Predicting Postoperative Outcomes Following Hip Fracture Surgery. Orthop Surg 15:1096–1103. https://doi.org/10.1111/os.13624
Koh GC, Tai BC, Ang LW, Heng D, Yuan JM, Koh WP (2013) All-cause and cause-specific mortality after hip fracture among Chinese women and men: the Singapore Chinese Health Study. Osteoporos Int 24:1981–1989. https://doi.org/10.1007/s00198-012-2183-7
Delgado A, Cordero GGE, Marcos S, Cordero-Ampuero J (2020) Influence of cognitive impairment on mortality, complications and functional outcome after hip fracture: Dementia as a risk factor for sepsis and urinary infection. Injury 51(Suppl 1):S19-s24. https://doi.org/10.1016/j.injury.2020.02.009
Scotland KB, Lo J, Grgic T, Lange D (2019) Ureteral stent-associated infection and sepsis: pathogenesis and prevention: a review. Biofouling 35:117–127. https://doi.org/10.1080/08927014.2018.1562549
Cumming D, Parker MJ (2007) Urinary catheterisation and deep wound infection after hip fracture surgery. Int Orthop 31:483–485. https://doi.org/10.1007/s00264-006-0227-3
Zeng G, Zhu W, Lam W, Bayramgil A (2020) Treatment of urinary tract infections in the old and fragile. World J Urol 38:2709–2720. https://doi.org/10.1007/s00345-020-03159-2
Gillespie WJ, Walenkamp GH (2010) Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. Cochrane Database Syst Rev 2010(3):Cd000244. https://doi.org/10.1002/14651858.CD000244.pub2
Langenhan R, Bushuven S, Reimers N, Probst A (2018) Peri-operative antibiotic treatment of bacteriuria reduces early deep surgical site infections in geriatric patients with proximal femur fracture. Int Orthop 42:741–746. https://doi.org/10.1007/s00264-017-3708-7
van Rijckevorsel V, de Jong L, Verhofstad MHJ, Roukema GR (2022) Influence of time to surgery on clinical outcomes in elderly hip fracture patients : an assessment of surgical postponement due to non-medical reasons. The Bone Joint J 104-b:1369–1378. https://doi.org/10.1302/0301-620x.104b12.Bjj-2022-0172.R2
Chen J, Wang X, Qian H, Ye J, Qian J, Hua J (2020) Correlation between common postoperative complications of prolonged bed rest and quality of life in hospitalized elderly hip fracture patients. Ann Palliat Med 9:1125–1133. https://doi.org/10.21037/apm-20-891
Hälleberg Nyman M, Johansson JE, Persson K, Gustafsson M (2011) A prospective study of nosocomial urinary tract infection in hip fracture patients. J Clin Nurs 20:2531–2539. https://doi.org/10.1111/j.1365-2702.2011.03769.x
Jamal Sepah Y, Umer M, Khan A, Ullah Khan Niazi A (2010) Functional outcome, mortality and in-hospital complications of operative treatment in elderly patients with hip fractures in the developing world. Int Orthop 34:431–435. https://doi.org/10.1007/s00264-009-0803-4
Lim SK, Beom J, Lee SY, Kim BR, Chun SW, Lim JY, Shin Lee E (2020) Association between sarcopenia and fall characteristics in older adults with fragility hip fracture. Injury 51:2640–2647. https://doi.org/10.1016/j.injury.2020.08.031
Agar A, Gulabi D, Sahin A, Gunes O, Hancerli CO, Kılıc B, Erturk C (2022) Acute kidney injury after hip fracture surgery in patients over 80 years of age. Arch Orthop Trauma Surg 142:2245–2252. https://doi.org/10.1007/s00402-021-03969-y
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study concept: DWB and QML. Study design: All authors. Acquisition, analysis, or interpretation of data: WY, WYT, WW, and QML. Statistical analysis: WY and WYT. Drafting of the manuscript: WY and WYT. Critical revision of the manuscript for important intellectual content: All authors.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of Dandong Central Hospital (No. DDZX-20230201) and conducted by the ethical principles outlined in the Helsinki Declaration of 1964 and its subsequent amendments. The ethics committee sought and obtained A waiver of consent for this cohort study.
Data availability
All the data used and analyzed during the current study are available from the corresponding author upon reasonable request.
Consent for publication
Not Applicable.
Competing interests
All authors state that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yao, W., Tang, W., Wang, W. et al. The relationship between admission hyperglycaemia and urinary tract infections in geriatric patients with hip fractures. International Orthopaedics (SICOT) 47, 2591–2600 (2023). https://doi.org/10.1007/s00264-023-05882-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05882-y