Abstract
Purpose
To evaluate the chondrotoxic effects of intra-articular use of TXA 20 mg/kg and/or 0.35% PVPI on knee joint cartilage in an experimental model of rabbits.
Methods
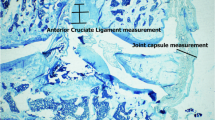
Forty-four male New Zealand adult rabbits were randomly assigned to four groups (control, tranexamic acid (TXA), povidone-iodine (PVPI), and PVPI + TXA). The knee joint cartilage was accessed through an arthrotomy and exposed to physiological saline SF 0.9% (control group), TXA, PVPI, and PVPI followed by TXA. Sixty days after surgical procedure, the animals were sacrificed and osteochondral specimens of the distal femur were obtained. Histological sections of cartilage from this area were stained with hematoxylin/eosin and toluidine blue. The following cartilage parameters were evaluated by the Mankin histological/histochemical grading system: structure, cellularity, glycosaminoglycan content in the extracellular matrix, and integrity of the tidemark.
Results
The isolated use of PVPI causes statistically significant changes in cartilage cellularity (p-value = 0.005) and decrease glycosaminoglycan content (p = 0.001), whereas the isolated use of TXA decreased significantly the glycosaminoglycan content (p = 0.031). The sequential use of PVPI + TXA causes more pronounced alterations in the structure (p = 0.039) and cellularity (p = 0.002) and decreased content of glycosaminoglycans (p < 0.001) all with statistical significance.
Conclusion
Data suggest that intra-articular use of tranexamic acid 20 mg/kg and intraoperative lavage with 0.35% povidone-iodine solution for three min are toxic to the articular cartilage of the knee in an experimental in vivo study in rabbits.




Similar content being viewed by others
Data availability
All data and materials are copyright of the author.
References
Pabinger C, Lothaller H, Geissler A (2015) Utilization rates of knee- arthroplasty in OECD countries. Osteoarthr Cartil 23(10):1664–1673
Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S (2017) Projected increase in total knee arthroplasty in the United States - an alternative projection model Osteoarthritis and Cartilage. Osteoarthr Cartil 25(11):1797–1803
Huitema GC, de Vries LMA, Verboom TW, Spekenbrink-Spooren A, Steens J (2022) Patella related problems as common reason for revision of NexGen PS® total knee arthroplasty without patella resurfacing: an analysis of 5911 primary total knee arthroplasties registered in the Dutch Arthroplasty Register. Knee 34:217–222
Gandhi R, Evans HM, Mahomed SR, Mahomed NN (2013) Tranexamic acid and the reduction of blood loss in total knee and hip arthroplasty: a meta-analysis. BMC Res Notes 6:184
Raut S, Mertes SC, Muniz-Terrera G, Khanduja V (2012) Factors associated with prolonged length of stay following a total knee replacement in patients aged over 75. Int Orthop 36:1601–1608
Konig G, Hamlin BR, Waters JH (2013) Topical tranexamic acid reduces blood loss and transfusion rates in total hip and total knee arthroplasty. J Arthroplasty 28(9):1473–1476
Fillingham YA, Ramkumar DB, Jevsevar DS, Yates AJ, Shores PD, Valle CJ (2018) The safety of tranexamic acid in total joint arthroplasty: a direct meta-analysis. J Arthroplasty 33(10):3070–3082
Chimento GF, Huff T, Ochsner JL Jr, Meyer M, Brandner L, Babin S (2013) An evaluation of the use of topical tranexamic acid in total knee arthroplasty. J Arthroplasty 28(8 suppl):74–77
Digas G, Koutsogiannis I, Meletiadis G (2015) Intra-articular injection of tranexamic acid reduce blood loss in cemented total knee arthroplasty. Eur J Orthop Surg Traumatol 25(7):1181–1188
Xu S, Chen JY, Zheng Q, Lo NN, Chia SL, Tay KJ, Pang HN, Shi L, Chan ES, Yeo SJ (2019) The safest and most efficacious route of tranexamic acid administration in total joint arthroplasty. A systemic review and network meta-analysis. Thromb Res 176:61–66
Morrison JJ, Dubose JJ, Rasmussen TE, Midwinter MJ (2012) Military application of tranexamic acid in trauma emergency resuscitation (MATTERs) study. Arch Surg 147(2):113–119
Goyal N, Chen DB, Harris IA (2017) Intravenous vs. intra-articular tranexamic acid in total knee arthroplasty: a randomized, double-blind trial. J Arthroplasty 32(1):28–32
Aguilera-Roig X, Jordan-Sales M, Natera-Cisneros L, Monllau-Garcia JC, Martinez-Zapata MJ (2014) Tranexamic acid in orthopedic surgery [in Spanish]. Rev Esp Cir Ortop Traumatol 58(1):52–56
Wong J, Abrishami A, El Beheiry H (2010) Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. J Bone Joint Surg Am 92(15):2503–2513
Georgiadis AG, Muh SJ, Silverton CD, Weir RM, Laker MW (2013) A prospective double-blind placebo controlled trial of topical tranexamic acid in total knee arthroplasty. J Arthroplasty 28(8 suppl):78–82
McLean M, McCall K, Smith IDM (2019) Tranexamic acid toxicity in human periarticular tissues. Bone Joint Res 8(1):11–18
Matar HE, Bloch BV, Snape SE (2021) Outcomes of single- and two-stage revision total knee arthroplasty for chronic periprosthetic joint infection: long-term outcomes of changing clinical practice in a specialist centre. Bone Joint J Aug 103-B(8):1373–1379
Mihalko WM, Manaswi A, Cui Q (2008) Diagnosis and treatment of the infected primary total knee arthroplasty. Instr Course Lect 57:327
Brown NM, Cipriano CA, Moric M (2012) Dilute betadine lavage before closure for the prevention of acute postoperative deep periprosthetic joint infection. J Arthroplasty 27:27
Chundamala J, Wright JG (2007) The efficacy and risks of using povidone–iodine irrigation to prevent surgical site infection: an evidence-based review. Can J Surg 50:473
Cheng MT, Chang MC, Wang ST (2005) Efficacy of dilute betadine solution irrigation in the prevention of postoperative infection of spinal surgery. Spine (Phila Pa 1976) 30:1689
Kim C-H, Kim H, Lee SJ, Yoon JY, Moon J-K, Lee S, Yoon PW (2020) The effect of povidone-iodine lavage in preventing infection after total hip and knee arthroplasties: systematic review and meta-analysis. J Arthroplasty 35(8):2267–2273
Shohat N, Goh GS, Harrer SL, Brown S (2022) Dilute povidone-iodine irrigation reduces the rate of periprosthetic joint infection following hip and knee arthroplasty: an analysis of 31,331 Cases. J Arthroplasty 37(2):226–231.e1
Jutai W, Feng S, Chen X, Lv Z, Zhe Q, Chen H, Xue C, Zhu M, Guo K-J, Wu P (2019) Intra-articular injection of tranexamic acid on perioperative blood loss during unicompartimental knee arthroplasty. Med Sci Monit 25:5068–5074
Tuttle JR, Feltman PR, Ritterman SA, Ehrlich MG (2015) Effects of tranexamic acid cytotoxicity on in vitro chondrocytes. Am J Orthop (Belle Mead NJ) 44(12):E497–E502
von Keudell A, Canseco JA, Gomoll AH (2013) Deleterious effects of diluted povidone–iodine on articular cartilage. J Arthroplasty 28:918–921
Mankin HJ, LippIello L (1970) Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips. J Bone and Joint Surg 52-A:424–434
Pauli C, Whiteside R, Heras FL, Nesic D, Koziol J, Grogan SP (2012) Comparison of cartilage histopathology assessment systems on human knee joints at all stages of osteoarthritis development. Osteoarthr Cartil 20(6):476–485
Mankin HJ, Dorfman H, Lippiello L, Zarins A (1971) Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips. II. Correlation of morphology with biochemical and metabolic data. J Bone Joint Surg 53-A:523–537
Van der Sluijs JA, Geesink RG, van der Linden AJ (1992) The reliability of the Mankin score for osteoarthritis. J Orthop Res 10:58–61
Paterson SI, Eltawil NM, Simpson AH, Amin AK, Hall AC (2016) Drying of open animal joints in vivo subsequently causes cartilage degeneration. Bone Joint Res 5(4):137–144
Özcan MS, Kalem M, Ozçelik M, Sahin E (2015) O efeito de levobupivacaína intra-articularsobre a cartilagem do ombro em doses diferentes - Estudo experimental. Rev Bras Anestesiol 67(1):42–49
Hollander M, Wolfe DA (1999) Nonparametric statistical methods, 2nd edn. John Wiley & Sons, New York
Agresti A (2000) Categorical analysis. John Wiley, New York
Jaescke R, Singer J, Guyatt GH (1989) Measurement of health status. Ascertaining the minimal clinically important difference. In: Controlled Clinical Trials
Copay AG, Subach BR, Glassman SD, Polly DW, Schuler TC (2007) Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 7(5):541–546
Kuhn K, D'Lima DD, Hashimoto S (2004) Cell death in cartilage. Osteoarthr Cartil 12:1
Blanco FJ, Guitian R, Vazquez-Martul E (1998) Osteoarthritis chondrocytes die by apoptosis. A possible pathway for osteoarthritis pathology. Arthritis Rheum 41:284
Kim HA, Lee YJ, Seong SC (2000) Apoptotic chondrocyte death in human osteoarthritis. J Rheumatol 27:455
Parker JD, Lim KS, Kieser DC, Woodfield TBF, Hooper GJ (2018) Is tranexamic acid toxic to articular cartilage when administered topically? Bone Joint J 100-B(3):404–412
Schaumburger J, Beckmann J, Springorum HR (2010) Toxicity of antiseptics on chondrocytes in vitro. Z Orthop Unfall 148:39
Kataoka M, Tsumura H, Kaku N (2006) Toxic effects of povidone–iodine on synovial cell and articular cartilage. Clin Rheumatol 25:632
Boyd JI III, Wongworawat MD (2004) High-pressure pulsatile lavage causes soft tissue damage. Clin Orthop Relat Res 427:13–17
Hassinger SM, Harding G, Wongworawat MD (2005) High-pressure pulsatile lavage propagates bacteria into soft tissue. Clin Orthop Relat Res 439:27–31
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Frederico Silva Pimenta, Marco Antônio Percope de Andrade, Cristiana Buzelin Nunes, Tulio Vinicius de Oliveira Campos, Guilherme Moreira de Abreu e Silva and Marcelo Araújo Buzelin. The first draft of the manuscript was written by Frederico Silva Pimenta and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent to participate
The research involved animals.
Consent to publish
The research involved animals.
Competing Interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pimenta, F.S., de Oliveira Campos, T.V., de Abreu e Silva, G.M. et al. Chondrotoxic effects of tranexamic acid and povidone-iodine on the articular cartilage of rabbits. International Orthopaedics (SICOT) 47, 2429–2437 (2023). https://doi.org/10.1007/s00264-023-05820-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05820-y