Abstract
Purpose
This scoping review aims to systematically map and summarise the available evidence on the management of chronic Achilles ruptures, whilst identifying prognostic factors and areas of future research.
Methods
A scoping review was performed according to the frameworks of Arksey and O’Malley, Levac and Peters. A computer-based search was performed in PubMed, Embase, EmCare, CINAHL, ISI Web of Science and Scopus, for articles reporting treatment of chronic Achilles ruptures. Two reviewers independently performed title/abstract and full text screening according to pre-defined selection criteria.
Results
A total of 747 unique articles were identified, of which 73 (9.8%) met all inclusion criteria. A variety of methods are described, with flexor hallucis longus tendon transfer being the most common. The most commonly reported outcome is the American Orthopaedic Foot and Ankle Society (AOFAS) score, although 16 other measures were reported in the literatures. All studies comparing pre- and post-operative outcomes reported significant post-treatment improvement. Complications were reported in 50 studies, with an overall pooled complication rate of 168/1065 (15.8%).
Conclusion
Although beneficial results were reported following a variety of techniques, comparison between these is challenging due to the low-level study designs used and confounding factors such as treatment delay and tendon gap size. Further research comparing the efficacy of different techniques is required in order to facilitate the development of an evidence-based treatment protocol. Such work would allow clinicians to better understand the suitability of the large variety of reported techniques and select the optimal strategy for each individual patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rupture of the Achilles tendon is a relatively common injury, with around 4500 Achilles ruptures occurring in the UK every year. Recent epidemiological data demonstrates a significant 39% rise in incidence, from 1.8 per 100,000 person years in the USA in 2012 to 2.5 per 100,000 person years in 2016. A similar trend is also reported in a number of other countries [1,2,3,4]. Given that the majority of Achilles ruptures occur during participation in sports such as basketball, numerous authors suggest that this increasing incidence may be due to an increase in participation in recreation sports, particularly in older adults. Other potential factors include an increased awareness and therefore diagnosis of ruptures by emergency doctors, although there is currently no strong evidence to support either hypothesis.
Treatment of acute ruptures is widely debated with previous research describing both operative and conservative (functional dynamic regime) methods [5,6,7]. Traditionally, open operative repair has been the favoured option with authors showing lower re-rupture rates compared to nonoperative methods [8, 9]. More recently, however, a number of authors have reported excellent outcomes and lower re-rupture rates, with the use of nonoperative functional orthotic treatment, such as the Leicester Achilles Management Protocol (LAMP) and Swansea Morriston Achilles Rupture Treatment (SMART) protocol. Research also suggests that nonoperative management is associated with fewer short-term complications. The emergence of this new evidence has led to non-operative treatment becoming the mainstay of contemporary treatment protocols. If the initial tendon rupture is not diagnosed promptly, as is the case in up to 20% of patients, the injury may then be termed chronic or neglected [10]. Authors disagree as to the exact definition of a chronic lesion; however, a recent systematic review by Flint et al. suggests that the term chronic should be used to define a rupture presenting at least four weeks after the initial injury [11].
A wide variety of techniques such as flexor hallucis longus tendon transfer and V–Y plasty [12,13,14] have been described in the management of chronic Achilles ruptures. To the best of our knowledge, the only previous scoping/systematic review investigating the full breadth of treatment options was published in 2013, with 34 studies included. However, since that date, there has been a surge in publications reporting treatment of chronic Achilles ruptures, using various techniques. There is therefore a gap in the current literature for an up-to-date review of management techniques. This scoping review addresses this by systematically mapping and summarising current evidence regarding the management of chronic Achilles ruptures, whilst identifying areas for future research. This aims to improve readers’ knowledge of the available treatment strategies and associated outcomes, and aid clinicians in optimising treatment protocols.
Methods
A scoping review methodology was chosen for this article due to the broad aim of systematically mapping and summarising the full breadth of literature regarding the treatment of chronic Achilles ruptures. Methodological guidelines for the conductance of scoping reviews have been developed by Arksey and O’Malley, Levac and The Joanna Briggs Institute [15,16,17]. This review adheres to these guidelines, which all describe five key stages in the conductance of a scoping review, as detailed below.
Identifying the research question
The following research questions were developed to guide this review:
-
What management options are currently reported for the management of chronic Achilles ruptures and what are their outcomes?
-
If possible to compare outcomes, which techniques have the greatest efficacy?
-
What prognostic factors may influence treatment outcome?
Identification of relevant studies
A thorough computer-based search was performed in six electronic databases including: PubMed, Embase, EmCare, CINAHL, ISI Web of Science and Scopus. A combination of free text and medical subject heading (MeSH) terms such as ‘Achilles’, ‘tendoachill*’, ‘calcaneal tendon’, ‘rupture’, ‘chronic’ and ‘neglected’ was used (see online resource 1 for full details). The Boolean operators ‘and’ and ‘or’ were used to combine terms in full search strings. All searches were performed with an English language restriction (as the research team lacks translation capabilities) and no date restrictions. Searches were conducted on 15 February 2021. Manual reference list analysis of review articles was performed to ensure retrieval of all relevant articles.
Study selection
Following article retrieval, all studies were imported into Rayyan systematic reviews web application to aid the screening process [18]. Two authors performed two-stage screening, initially involving title/abstract screening and then full text screening, guided by the selection criteria below:
-
1.
Population: Patients of all ages with chronic Achilles ruptures. Due to the large variation in the time period used to define a chronic rupture, no restriction as to the minimum duration between injury and diagnosis/treatment was imposed. All studies describing treatment of ‘chronic’ or ‘neglected’ Achilles ruptures were included.
-
2.
Intervention: Any intervention for the management of chronic Achilles rupture.
-
3.
Comparison: A comparison group was not required for inclusion in this review.
-
4.
Outcomes: Studies reporting outcomes using any validated or non-validated scores were included. Examples of scores include American Foot and Ankle Society (AOFAS) score, Achilles Tendon Total Rupture Score (ATRS), Leppilahti score, Tegner Score, Hooker scale and 36-item short-form survey (SF-36). Studies reporting outcomes only in terms of patient-reported satisfaction or symptom improvement were excluded.
-
5.
Study design: Original research studies (observational studies, cohort studies, randomised controlled trials) were included. Review articles, case reports, commentaries and abstracts were excluded. Studies failing to report treatment outcomes for Achilles rupture separately from other conditions, for example, Achilles tendinosis, were excluded.
-
6.
Date: No publication date inclusion criteria were imposed at either the search or screening stage.
-
7.
Language: Studies published in the English language were included. Due to the lack of funding and linguistic capabilities of the research team, studies published in all other languages were excluded.
Charting the data
A pilot data extraction form was created following discussion between the review team. This sheet contained the following headings:
-
Author
-
Year of publication
-
Type of study
-
Number of patients
-
Mean age
-
Male: female ratio
-
Treatment method
-
Mean size of tendon defect
-
Mean treatment delay
-
Outcome scores, e.g. AOFAS, SF-36, ATRS, etc.
-
Significant difference between pre- and post-operative score
-
Any comparison group and outcome comparison?
-
Re-rupture rate
-
Complications
-
Follow-up period
Two reviewers independently used this form to extract data from the first ten relevant studies. Discussion then took place as to the suitability of the form [19], at which point the decision was taken to add two further headings, ‘minimum treatment delay for inclusion’ and ‘prognostic factors’. Once these headings were added, the final sheet was used to extract relevant data from all studies.
Collating, summarising and reporting the results
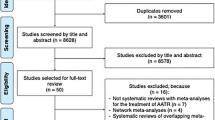
Study results are reported in a qualitative thematic manner, with distinct sections focussing on key themes such as the outcome measures used, treatment results and complications. Basic study characteristics including year of publication, number of patients, mean age, male:female ratio and follow-up period are displayed in Table 1. The number of studies retrieved using the search strategy and excluded at both the title/abstract and full text screening stage is detailed in a PRISMA flow diagram [20]. Outcome scores were pooled across studies reporting the same treatment technique if there were at least five studies reporting a particular technique and if at least three of these studies reported both pre- and post-operative outcome scores. Pooling was performed in R 4.0.0 software (R foundation for statistical computing, Vienna, Austria), using DerSimonian and Laird random effects weighting. Missing standard deviation values were imputed according to the method of Walter and Yao [21]. The pooled pre-operative outcome score was subtracted from the equivalent pooled post-operative score to calculate an unstandardised mean difference. Studies which did not record both a pre- and post-operative score were not included in this analysis.
Results
A total of 747 unique articles were identified, of which 73 (10.3%) were included in the final review (Fig. 1). Summary statistics of all included studies are presented in Table 1.
Treatment techniques
A wide variety of treatment methods were reported in the included literature, as detailed in Fig. 2. The most common technique is flexor hallucis longus (FHL) tendon transfer, reported in a total of 22 studies. Of these, two studies used both a single and a double incision approach in different patients, seven exclusively used a single incision, nine a double incision, two an endoscopic approach and two did not specify the exact approach. Other tendon transfer methods, such as semitendinosus tendon transfer (ST transfer), peroneus brevis tendon transfer (PB transfer) and hamstring tendon transfer, were reported in seven, six and two studies, respectively. Percutaneous techniques, including a figure of eight stitch repair or modified Bunnell repair, were reported in two studies [30, 52]. A total of ten studies used gastrocnemius flaps with no augmentation, whilst six studies describe additional FHL augmentation (Fig. 2). Techniques such as V–Y and Z plasty were reported both as stand-alone techniques or combined with a synthetic acellular human dermal tissue matrix graft jacket (Wright Medical Technology, Inc., Arlington, TN) or FHL transfer [53]. Other less commonly reported techniques include use of the Ligament Advanced Reinforcement System (LARS) graft (JK Orthomedic, Dollard-des-Ormeaux, Quebec, Canada), polyester tape, scar tissue interposition and Duthie’s biological repair [10, 43, 45, 91]. Only one study described nonoperative treatment, using an orthosis as part of the SMART protocol [89].
Flowchart detailing the number of studies using a particular treatment technique. FHL flexor hallucis longus, FDL: flexor digitorum longus: Semitendinosus, LARS: Ligament Advanced Reinforcement System (LARS) graft (JK Orthomedic, Dollard-des-Ormeaux, Quebec, Canada. *Two studies used both a single and a double incision FHL transfer approach in different patients, seven exclusively used a single incision, nine a double incision, two an endoscopic approach and two did not specify the exact approach
Outcome measures
A similarly wide variety was seen in the outcome measures used to assess treatment outcomes. AOFAS is the most commonly used score, followed by ATRS, Leppilahti score and VAS (Table 2).
Treatment outcome
The outcomes of treatment using different techniques are detailed in Table 3. All 32 studies reporting both pre- and post-operative outcome measures found significant improvements in all measures used, with the exception of Koh et al., which found a significant improvement in AOFAS and VAS and SF-36 physical subscale but not SF-36 mental subscale score [50].
Only two treatment techniques met the outlined pooling criteria. A total of eight studies describing FHL transfer showed a mean pre-operative AOFAS of 62.3 (95% CI: 57.1–67.4) and mean post-operative AOFAS of 94.2 (95% CI: 90.9–97.4), giving an unstandardised mean difference of 31.9 [22, 50, 63, 66, 75, 78, 88, 92]. Unfortunately, there were an insufficient number of studies reporting the same treatment outcome to specifically compare outcomes seen using a single or double incision approach. Three studies describing semitendinosus transfer show a pooled mean ATRS of 40.8 (95% CI: 30.4–51.1), post-operative ATRS of 88.5 (95% CI: 84.2–92.9) and mean difference of 47.7 [57, 61, 79]. No formal comparison of these mean differences was performed, due to the heterogeneity in outcome measure and low-level case series study design used and inability to control for potential confounding factors such as treatment delay, length of tendon gap, patient age and follow-up period.
Complications
A total of 50 studies involving 1063 patients (1065 feet) clearly reported treatment complications (Table 4). Complications were categorised as infection (superficial wound infection, deep infection), wound healing (wound dehiscence, delayed wound closure, hypertrophic scar, wound breakdown, wound gaping), tendon re-rupture and others. The overall pooled complication rate was 168/1065 (15.8%), with the most common complication being infection (58/1065, 5.5%).
Discussion
The aim of this scoping review was to systematically map and summarise current literature describing the treatment of chronic Achilles tendon ruptures. A previous systematic review on the same subject, performed in 2012 by Hadi et al., included 34 studies [12]. Since then, there appears to have been a surge in publications on the topic, with 43 of the 73 (58.9%) included in this review published in 2013 onwards (Table 1). Unfortunately, despite this surge in the number of publications, the quality and level of evidence has not risen. As in the review of Hadi et al., the majority of included studies are level IV evidence case series, with only seven comparative cohort studies identified [12].
There is a large degree of heterogeneity in treatment methods for chronic Achilles ruptures, with studies reporting a variety of tendon transfer, turndown flap, tendon lengthening and synthetic repair techniques. A number of authors also described the use of dual techniques involving a combination of more than one of the above methods. All techniques described appeared to show good post-operative results, with all relevant included studies reporting a statistically significant increase in pre- to post-operative scores such as AOFAS and ATRS (Table 3). However, ascertaining the most efficacious technique is challenging, due to the poor quality of the existing literature. A formal meta-analysis comparing pooled outcomes of different treatment strategies was not possible due to a number of factors including large number of different techniques, large variety in outcome measures reported, low-level case series study design and inability to control for factors which may influence outcomes such as patient age, length of treatment delay and length of tendon gap. Comparison is also currently hampered by the widespread use of non-validated outcome measures. The most commonly used measure was the AOFAS (Table 2), which is not validated for use in Achilles ruptures and its use is no longer recommended by The American Orthopaedic Foot and Ankle Society [93]. Future research should therefore endeavour to use outcome measures specifically validated for Achilles ruptures such as the ATRS.
However, even if such a comparison between treatment techniques was possible, it is likely that there is no a single optimal operative strategy for all patients. Instead, it may be more important to develop an evidence-based optimal treatment protocol, identifying stratification criteria that takes into account unique patient factors, such as length of treatment delay and tendon gap size, which may determine the suitability of a particular technique. Some authors have described such treatment protocols. For example, Myerson recommends primary repair in cases with < 2 cm gap, V–Y plasty in the case of a 2–5 cm gap and tendon transfer with or without V–Y plasty in cases with gap > 5 cm [94]. Maffulli et al. use peroneus brevis transfer for gaps < 6 cm, semitendinosus graft for gaps > 6 cm and FHL transfer for gaps > 5 cm [61]. Similar gap size-based protocols are also described by Kuwada, Den Hartog and Krahe [95,96,97]. However, these protocols are not based on definitive evidence as there is currently a lack of literature comparing different treatment methods. Although Elias et al., who described FHL transfer, did not find any significant difference in outcomes according to age or length of delay, worse outcomes were seen in those with larger tendon gaps of 7–8 cm [97]. However, firm conclusions cannot be drawn from the findings of these 15-patient case series describing only one technique. It is therefore important that further high-quality research, comparing different treatment techniques in patients of varying age, tendon gap length, treatment delay, injury aetiology and degree of tendon degeneration, is performed. Such works would aid the development of an evidence-based treatment protocol, which would allow clinicians to select the optimal technique for each specific patient, taking into account the above factors.
Furthermore, although there is a growing body of evidence supporting the role of conservative treatment in acute Achilles rupture, there is a paucity of literature investigating the same in chronic ruptures [9]. This is likely due to the traditional view that operative treatment yields superior outcomes for chronic ruptures. However, again, this seems to be derived from anectodical evidence rather than high-quality research. Only one included study investigates the role of conservative treatment and, to the best of our knowledge, the only article directly comparing operative versus conservative treatment in chronic ruptures is the 1953 study of Christensen [89, 98]. This study does indeed suggest superiority of operative treatment; however, it is not possible to draw conclusions from a single small case series. Further research is therefore required in ascertaining the suitability of conservative treatment and specific factors which may predict response to such treatment. Even if it is the case that operative treatment is superior, there may be certain patients who decline, or are not suitable for operative intervention. Although Achilles tendon rupture most frequently occurs in adults aged between 30 and 40, there are a group of older patients sustaining Achilles tendon rupture who may not be able to tolerate surgery and the mean age at which rupture occurs has increased by at least 0.721 years every five years since 1953 [99]. This suggests that clinicians are likely to come across an increasing number of patients for whom operative intervention is not suitable, further emphasising the importance of research into the development of effective conservative therapies.
Despite the rigorous methodology employed in this review, it must be acknowledged that certain biases do exist. For example, due to the limited linguistic capabilities of the research team, only studies published in the English language were included. Furthermore, as described, there are a number of confounding factors such as treatment delay and tendon gap length, which may differ between individual studies and affect reported outcomes. As outlined in Table 1, the large majority of studies utilise a level IV retrospective case series design. Such studies are particularly prone to selection bias, drawing patients from a relatively narrow sample population. Lastly, it was decided to include studies reporting both validated and non-validated outcome scores, as well as patient reported, and researcher assessed scores. This may cause some bias in outcome scores, with only 21 of 73 included studies using the validated ATRS outcome scale.
Conclusion
The current literature describes a number of different operative strategies for the management of chronic Achilles rupture, all of which demonstrate beneficial outcomes. However, comparison of specific techniques is currently hampered by the low-level evidence and inability to control for potential confounding factors. Future research directly comparing treatment strategies in patients stratified according to specific injury characteristics may aid in the development of an evidence-based optimal treatment protocol. This would allow clinicians to determine which of the multitude of available techniques is most suitable for each unique patient.
Data availability
All data is freely available online.
References
Boyd RP, Dimock R, Solan MC, Porter E (2015) Achilles tendon rupture: How to avoid missing the diagnosis. Br J Gen Pract. https://doi.org/10.3399/bjgp15x688069
Lemme NJ, Li NY, DeFroda SF et al (2018) Epidemiology of Achilles Tendon Ruptures in the United States: Athletic and Nonathletic Injuries From 2012 to 2016. Orthop J Sport Med. https://doi.org/10.1177/2325967118808238
Möller A, Åström M, Westlin NE (1996) Increasing incidence of Achilles tendon rupture. Acta Orthop Scand. https://doi.org/10.3109/17453679608996672
Maffulli N, Waterston SW, Squair J et al (1999) Changing incidence of Achilles tendon rupture in Scotland: A 15-year study. Clin J Sport Med. https://doi.org/10.1097/00042752-199907000-00007
Nilsson-Helander K, Grävare Silbernagel K, Thomeé R et al (2010) Acute achilles tendon rupture: A randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. https://doi.org/10.1177/0363546510376052
Deng S, Sun Z, Zhang C, et al (2017) Surgical Treatment Versus Conservative Management for Acute Achilles Tendon Rupture: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Foot Ankle Surg 56(6):1236–1243. https://doi.org/10.1053/j.jfas.2017.05.036
Yang X, Meng H, Quan Q, et al (2018) Management of acute Achilles tendon ruptures. Bone Jt Res 7:561–569. https://doi.org/10.1302/2046-3758.710.BJR-2018-0004.R2
Khan RJ, Fick DP, Keogh A, Carey Smith RL (2009) Interventions for treating acute Achilles tendon ruptures. In: Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD003674.pub3
Ochen Y, Beks RB, Van Heijl M, et al (2019) Operative treatment versus nonoperative treatment of Achilles tendon ruptures: Systematic review and meta-analysis. BMJ 364:k5120. https://doi.org/10.1136/bmj.k5120
Ibrahim SAR (2009) Surgical treatment of chronic Achilles tendon rupture. J foot ankle Surg Off Publ Am Coll Foot Ankle Surg 48:340–346. https://doi.org/10.1053/j.jfas.2009.02.007
Flint JH, Wade AM, Giuliani J, Rue J-P (2014) Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med 42:235–241. https://doi.org/10.1177/0363546513490656
Hadi M, Young J, Cooper L et al (2013) Surgical management of chronic ruptures of the Achilles tendon remains unclear: a systematic review of the management options. Br Med Bull 108:95–114. https://doi.org/10.1093/bmb/ldt019
Lin Y, Yang L, Yin L, Duan X (2016) Surgical Strategy for the Chronic Achilles Tendon Rupture. Biomed Res Int 2016:1416971. https://doi.org/10.1155/2016/1416971
Maffulli N, Ajis A (2008) Management of chronic ruptures of the Achilles tendon. J Bone Joint Surg Am 90:1348–1360. https://doi.org/10.2106/JBJS.G.01241
Arksey H, O’Malley L (2005) Scoping studies: Towards a methodological framework. Int J Soc Res Methodol Theory Pract. https://doi.org/10.1080/1364557032000119616
Levac D, Colquhoun H, O’Brien KK (2010) Scoping studies: Advancing the methodology. Implement Sci. https://doi.org/10.1186/1748-5908-5-69
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil, H (2020) Chapter 11: scoping reviews (2020 version). In: Aromataris E, Munn Z (eds) JBI manual for evidence synthesis, JBI. Available from https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-12
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev. https://doi.org/10.1186/s13643-016-0384-4
Kastner M, Tricco AC, Soobiah C, et al (2012) What is the most appropriate knowledge synthesis method to conduct a review? Protocol for a scoping review. BMC Med Res Methodol. https://doi.org/10.1186/1471-2288-12-114
Moher D, Liberati A, Tetzlaff J, et al (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLos Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Walter S, Yao X (2007) Effect sizes can be calculated for studies reporting ranges for outcome variables in systematic reviews. J Clin Epidemiol 60:849–852. https://doi.org/10.1016/j.jclinepi.2006.11.003
Abubeih H, Khaled M, Saleh WR, Said GZ (2018) Flexor hallucis longus transfer clinical outcome through a single incision for chronic Achilles tendon rupture. Int Orthop 42:2699–2704. https://doi.org/10.1007/s00264-018-3976-x
Ahmad J, Jones K, Raikin SM (2016) Treatment of Chronic Achilles Tendon Ruptures With Large Defects. Foot Ankle Spec 9:400–408. https://doi.org/10.1177/1938640016640895
Alhaug OK, Berdal G, Husebye EE, Hvaal K (2019) Flexor hallucis longus tendon transfer for chronic Achilles tendon rupture. A retrospective study. Foot ankle Surg Off J Eur Soc Foot Ankle Surg 25:630–635. https://doi.org/10.1016/j.fas.2018.07.002
Arthur JM, Venrick CB, Ryan PM (2020) “don’t Make the Gap” Surgical Technique and Case Series for Chronic Achilles Rupture. Tech Foot Ankle Surg. https://doi.org/10.1097/BTF.0000000000000296
Badalihan A, Aihemaiti A, Shawutali N et al (2015) Outcome of a one-stage tensile stress surgical technique and early postoperative rehabilitation in the treatment of neglected achilles tendon rupture. J foot ankle Surg Off Publ Am Coll Foot Ankle Surg 54:153–159. https://doi.org/10.1053/j.jfas.2014.12.002
Bai L, Guan S, You T et al (2019) Comparison of Gastrocnemius Turn Flap and Hamstring Graft for the Treatment of Kuwada Type 3 Chronic Ruptures of the Achilles Tendon: A Retrospective Study. Orthop J Sport Med 7:2325967119887673. https://doi.org/10.1177/2325967119887673
Baumfeld D, Baumfeld T, Figueiredo AR, et al (2017) Endoscopic Flexor Halluces Longus transfer for Chronic Achilles Tendon rupture - technique description and early post-operative results. Muscles Ligaments Tendons J 7:341–346. https://doi.org/10.11138/mltj/2017.7.2.341
Becher C, Donner S, Brucker J et al (2018) Outcome after operative treatment for chronic versus acute Achilles tendon rupture - A comparative analysis. Foot ankle Surg Off J Eur Soc Foot Ankle Surg 24:110–114. https://doi.org/10.1016/j.fas.2016.12.003
Bertelli R, Gaiani L, Palmonari M (2009) Neglected rupture of the Achilles tendon treated with a percutaneous technique. Foot ankle Surg Off J Eur Soc Foot Ankle Surg 15:169–173. https://doi.org/10.1016/j.fas.2008.12.003
Borah DN, Rai S, Frank HC, Dutta A (2020) Repair of chronic Achilles tendon rupture using Bosworth’s technique. J Orthop Trauma Rehabil. https://doi.org/10.1177/2210491720972713
Coull R, Flavin R, Stephens MM (2003) Flexor hallucis longus tendon transfer: evaluation of postoperative morbidity. Foot ankle Int 24:931–934. https://doi.org/10.1177/107110070302401211
Elgohary HEA, Elmoghazy NA, Abd Ellatif MS (2016) Combined flexor hallucis longus tendon transfer and gastrocnemius recession for reconstruction of gapped chronic achilles tendon ruptures. Injury 47:2833–2837. https://doi.org/10.1016/j.injury.2016.10.029
El Shazly O, Abou El Soud MM, El Mikkawy DME et al (2014) Endoscopic-assisted achilles tendon reconstruction with free hamstring tendon autograft for chronic rupture of achilles tendon: clinical and isokinetic evaluation. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc North Am Int Arthrosc Assoc 30:622–628. https://doi.org/10.1016/j.arthro.2014.02.019
El Shewy MT, El Barbary HM, Abdel-Ghani H (2009) Repair of chronic rupture of the achilles tendon using 2 intratendinous flaps from the proximal gastrocnemius-soleus complex. Am J Sports Med 37:1570–1577. https://doi.org/10.1177/0363546509333009
Elias I, Besser M, Nazarian LN, Raikin SM (2007) Reconstruction for missed or neglected Achilles tendon rupture with V-Y lengthening and flexor hallucis longus tendon transfer through one incision. Foot ankle Int 28:1238–1248. https://doi.org/10.3113/FAI.2007.1238
Esenyel CZ, Tekin C, Cakar M et al (2014) Surgical treatment of the neglected achilles tendon rupture with Hyalonect. J Am Podiatr Med Assoc 104:434–443. https://doi.org/10.7547/0003-0538-104.5.434
Fotiadis E, Chatzisimeon A, Samoladas E et al (2008) A Combined Repair Technique for Early Neglected Achilles Tendon Ruptures. Eur J trauma Emerg Surg Off Publ Eur Trauma Soc 34:37–42. https://doi.org/10.1007/s00068-007-7038-0
Gedam PN, Rushnaiwala FM (2016) Endoscopy-Assisted Achilles Tendon Reconstruction With a Central Turndown Flap and Semitendinosus Augmentation. Foot ankle Int 37:1333–1342. https://doi.org/10.1177/1071100716666365
Guclu B, Basat HC, Yildirim T et al (2016) Long-term Results of Chronic Achilles Tendon Ruptures Repaired With V-Y Tendon Plasty and Fascia Turndown. Foot ankle Int 37:737–742. https://doi.org/10.1177/1071100716642753
Hahn F, Meyer P, Maiwald C et al (2008) Treatment of chronic achilles tendinopathy and ruptures with flexor hallucis tendon transfer: clinical outcome and MRI findings. Foot ankle Int 29:794–802. https://doi.org/10.3113/FAI.2008.0794
Hollawell S, Baione W (2015) Chronic Achilles Tendon Rupture Reconstructed With Achilles Tendon Allograft and Xenograft Combination. J foot ankle Surg Off Publ Am Coll Foot Ankle Surg 54:1146–1150. https://doi.org/10.1053/j.jfas.2014.09.006
Ibrahim SA, Hamido F, Al Misfer ARK et al (2007) Chronic rupture of Achillis tendon operative management using two in one operation. Foot Ankle Surg 13:140–142. https://doi.org/10.1016/j.fas.2007.04.001
Jain M, Tripathy SK, Behera S, et al (2020) Functional outcome of gastrocnemius advancement flap augmented with short flexor hallucis longus tendon transfer in chronic Achilles tear. Foot 45:N.PAG-N.PAG. https://doi.org/10.1016/j.foot.2020.101704
Jennings AG, Sefton GK (2002) Chronic rupture of tendo Achillis. Long-term results of operative management using polyester tape. J Bone Joint Surg Br 84:361–363. https://doi.org/10.1302/0301-620x.84b3.11559
Jiang X-J, Shen J-J, Huang J-F, Tong P-J (2019) Reconstruction of Myerson type III chronic Achilles tendon ruptures using semitendinosus tendon and gracilis tendon autograft. J Orthop Surg (Hong Kong) 27:2309499019832717. https://doi.org/10.1177/2309499019832717
Jielile J, Badalihan A, Qianman B et al (2016) Clinical outcome of exercise therapy and early post-operative rehabilitation for treatment of neglected Achilles tendon rupture: a randomized study. Knee Surg Sports Traumatol Arthrosc 24:2148–2155. https://doi.org/10.1007/s00167-015-3598-4
Khalid MA, Weiss WM, Iloanya M, Panchbhavi VK (2019) Dual Purpose Use of Flexor Hallucis Longus Tendon for Management of Chronic Achilles Tendon Ruptures. Foot Ankle Spec 12:345–349. https://doi.org/10.1177/1938640018803695
Khiami F, Di Schino M, Sariali E et al (2013) Treatment of chronic Achilles tendon rupture by shortening suture and free sural triceps aponeurosis graft. Orthop Traumatol Surg Res 99:585–591. https://doi.org/10.1016/j.otsr.2013.03.021
Koh D, Lim J, Chen JY et al (2019) Flexor hallucis longus transfer versus turndown flaps augmented with flexor hallucis longus transfer in the repair of chronic Achilles tendon rupture. Foot ankle Surg Off J Eur Soc Foot Ankle Surg 25:221–225. https://doi.org/10.1016/j.fas.2017.10.019
Kosaka T, Yamamoto K (2011) Long-term effects of chronic Achilles tendon rupture treatment, using reconstruction with peroneus brevis transfer, on sports activities. West Indian Med J 60:628–635
Kosanović M, Brilej D (2008) Chronic rupture of Achilles tendon: is the percutaneous suture technique effective? Arch Orthop Trauma Surg 128:211–216. https://doi.org/10.1007/s00402-007-0514-5
Lee DK (2007) Achilles tendon repair with acellular tissue graft augmentation in neglected ruptures. J foot ankle Surg Off Publ Am Coll Foot Ankle Surg 46:451–455. https://doi.org/10.1053/j.jfas.2007.05.007
Lin Y-J, Duan X-J, Yang L (2019) V-Y Tendon Plasty for Reconstruction of Chronic Achilles Tendon Rupture: A Medium-term and Long-term Follow-up. Orthop Surg 11:109–116. https://doi.org/10.1111/os.12429
Lins C, Ninomya AF, Bittar CK et al (2013) Kinetic and kinematic evaluation of the ankle joint after achilles tendon reconstruction with free semitendinosus tendon graft: preliminary results. Artif Organs 37:291–297. https://doi.org/10.1111/j.1525-1594.2012.01559.x
Maffulli N, Spiezia F, Testa V et al (2012) Free gracilis tendon graft for reconstruction of chronic tears of the Achilles tendon. J Bone Joint Surg Am 94:906–910. https://doi.org/10.2106/JBJS.K.00869
Maffulli N, Del Buono A, Loppini M, Denaro V (2014) Ipsilateral free semitendinosus tendon graft with interference screw fixation for minimally invasive reconstruction of chronic tears of the Achilles tendon. Oper Orthop Traumatol 26:513–519. https://doi.org/10.1007/s00064-012-0228-x
Maffulli N, Spiezia F, Longo UG, Denaro V (2010) Less-invasive reconstruction of chronic achilles tendon ruptures using a peroneus brevis tendon transfer. Am J Sports Med 38:2304–2312. https://doi.org/10.1177/0363546510376619
Maffulli N, Del Buono A, Spiezia F et al (2013) Less-invasive semitendinosus tendon graft augmentation for the reconstruction of chronic tears of the Achilles tendon. Am J Sports Med 41:865–871. https://doi.org/10.1177/0363546512473819
Maffulli N, Spiezia F, Pintore E et al (2012) Peroneus brevis tendon transfer for reconstruction of chronic tears of the Achilles tendon: a long-term follow-up study. J Bone Joint Surg Am 94:901–905. https://doi.org/10.2106/JBJS.K.00200
Maffulli N, Aicale R, Tarantino D (2017) Autograft Reconstruction for Chronic Achilles Tendon Disorders. Tech FOOT ANKLE Surg 16:117–123. https://doi.org/10.1097/BTF.0000000000000154
Maffulli N, Leadbetter WB (2005) Free gracilis tendon graft in neglected tears of the achilles tendon. Clin J Sport Med Off J Can Acad Sport Med 15:56–61. https://doi.org/10.1097/01.jsm.0000152714.05097.ef
Mahajan RH, Dalal RB (2009) Flexor hallucis longus tendon transfer for reconstruction of chronically ruptured Achilles tendons. J Orthop Surg (Hong Kong) 17:194–198. https://doi.org/10.1177/230949900901700215
Mann RA, Holmes GBJ, Seale KS, Collins DN (1991) Chronic rupture of the Achilles tendon: a new technique of repair. J Bone Joint Surg Am 73:214–219
Mao H, Shi Z, Xu D, Liu Z (2015) Neglected Achilles Tendon Rupture Treated with Flexor Hallucis Longus transfer with two turndown gastrocnemius fascia flap and reinforced with plantaris tendon. Acta Orthop Belg 81:553–560
Miao X, Wu Y, Tao H et al (2016) Reconstruction of Kuwada grade IV chronic achilles tendon rupture by minimally invasive technique. Indian J Orthop 50:523–528. https://doi.org/10.4103/0019-5413.189599
Miskulin M, Miskulin A, Klobucar H, Kuvalja S (2005) Neglected rupture of the Achilles tendon treated with peroneus brevis transfer: a functional assessment of 5 cases. J foot ankle Surg Off Publ Am Coll Foot Ankle Surg 44:49–56. https://doi.org/10.1053/j.jfas.2004.11.003
Mulier T, Rummens E, Dereymaeker G (2007) Risk of neurovascular injuries in flexor hallucis longus tendon transfers: an anatomic cadaver study. Foot ankle Int 28:910–915. https://doi.org/10.3113/FAI.2007.0910
Nambi GI, Salunke AA, Pathak S et al (2020) “Repair and Flap technique”: A Retrospective Analysis of Single Stage Reconstruction Method for Treatment of Chronic Open Achilles Tendon Defect with Proximal Turndown Flap and Reverse Sural Flap. Indian J Orthop. https://doi.org/10.1007/s43465-020-00278-1
Oksanen MM, Haapasalo HH, Elo PP, Laine H-J (2014) Hypertrophy of the flexor hallucis longus muscle after tendon transfer in patients with chronic Achilles tendon rupture. Foot ankle Surg Off J Eur Soc Foot Ankle Surg 20:253–257. https://doi.org/10.1016/j.fas.2014.06.003
Ozan F, Dogar F, Gurbuz K, et al (2017) Chronic Achilles Tendon Rupture Reconstruction Using the Lindholm Method and the Vulpius Method. J Clin Med Res 9:573–578. https://doi.org/10.14740/jocmr2943w
Ozer H, Ergisi Y, Harput G et al (2018) Short-Term Results of Flexor Hallucis Longus Transfer in Delayed and Neglected Achilles Tendon Repair. J foot ankle Surg Off Publ Am Coll Foot Ankle Surg 57:1042–1047. https://doi.org/10.1053/j.jfas.2018.03.005
Park Y-S, Sung K-S (2012) Surgical reconstruction of chronic achilles tendon ruptures using various methods. Orthopedics 35:e213–e218. https://doi.org/10.3928/01477447-20120123-13
Parsons JR, Weiss AB, Schenk RS et al (1989) Long-term follow-up of achilles tendon repair with an absorbable polymer carbon fiber composite. Foot Ankle 9:179–184. https://doi.org/10.1177/107110078900900406
Pendse A, Kankate R (2019) Reconstruction of chronic achilles tendon ruptures in elderly patients, with vascularized flexor hallucis longus tendon transfer using single incision technique. Acta Orthop Belg 85:137–143
Pintore E, Barra V, Pintore R, Maffulli N (2001) Peroneus brevis tendon transfer in neglected tears of the Achilles tendon. J Trauma 50:71–78. https://doi.org/10.1097/00005373-200101000-00013
Pavan Kumar A, Shashikiran R, Raghuram C (2013) A novel modification of Bosworth’s technique to repair zone I Achilles tendon ruptures. J Orthop Traumatol Off J Ital Soc Orthop Traumatol 14:59–65. https://doi.org/10.1007/s10195-012-0222-y
Rahm S, Spross C, Gerber F et al (2013) Operative treatment of chronic irreparable Achilles tendon ruptures with large flexor hallucis longus tendon transfers. Foot ankle Int 34:1100–1110. https://doi.org/10.1177/1071100713487725
Sarzaeem MM, Lemraski MMB, Safdari F (2012) Chronic Achilles tendon rupture reconstruction using a free semitendinosus tendon graft transfer. Knee Surg Sports Traumatol Arthrosc 20:1386–1391. https://doi.org/10.1007/s00167-011-1703-x
Seker A, Kara A, Armagan R et al (2016) Reconstruction of neglected achilles tendon ruptures with gastrocnemius flaps: excellent results in long-term follow-up. Arch Orthop Trauma Surg 136:1417–1423. https://doi.org/10.1007/s00402-016-2506-9
Shoaib A, Mishra V, A. S, (2017) Surgical repair of symptomatic chronic achilles tendon rupture using synthetic graft augmentation. Foot Ankle Surg 23:179–182. https://doi.org/10.1016/j.fas.2016.04.006
Song Y-J, Chen G, Jia S-H et al (2020) Good outcomes at mid-term following the reconstruction of chronic Achilles tendon rupture with semitendinosus allograft. Knee Surg Sports Traumatol Arthrosc 28:1619–1624. https://doi.org/10.1007/s00167-018-5113-1
Takao M, Ochi M, Naito K et al (2003) Repair of neglected Achilles tendon rupture using gastrocnemius fascial flaps. Arch Orthop Trauma Surg 123:471–474. https://doi.org/10.1007/s00402-002-0443-2
Tay D, Lin HA, Tan BS et al (2010) Chronic Achilles tendon rupture treated with two turndown flaps and flexor hallucis longus augmentation - two-year clinical outcome. Ann Acad Med Singapore 39:58–60
Usuelli FG, D’Ambrosi R, Manzi L et al (2017) Clinical Outcomes and Return to Sports in Patients with Chronic Achilles Tendon Rupture after Minimally Invasive Reconstruction with Semitendinosus Tendon Graft Transfer. Joints 5:212–216. https://doi.org/10.1055/s-0037-1608661
Vega J, Vilá J, Batista J et al (2018) Endoscopic Flexor Hallucis Longus Transfer for Chronic Noninsertional Achilles Tendon Rupture. Foot ankle Int 39:1464–1472. https://doi.org/10.1177/1071100718793172
Wapner KL, Pavlock GS, Hecht PJ et al (1993) Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot Ankle 14:443–449. https://doi.org/10.1177/107110079301400803
Wegrzyn J, Luciani J-F, Philippot R et al (2010) Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int Orthop 34:1187–1192. https://doi.org/10.1007/s00264-009-0859-1
Winson DMG, MacNair R, Hutchinson A-M, et al (2020) Delayed Achilles tendon rupture presentation: Non-operative management may be the SMART choice. Foot (Edinb) 101724. https://doi.org/10.1016/j.foot.2020.101724
Yasuda T, Shima H, Mori K et al (2016) Direct Repair of Chronic Achilles Tendon Ruptures Using Scar Tissue Located Between the Tendon Stumps. J Bone Joint Surg Am 98:1168–1175. https://doi.org/10.2106/JBJS.15.00865
Yasuda T, Kinoshita M, Okuda R (2007) Reconstruction of chronic achilles tendon rupture with the use of interposed tissue between the stumps. Am J Sports Med 35:582–588. https://doi.org/10.1177/0363546506295939
Yeoman TFM, Brown MJC, Pillai A (2012) Early post-operative results of neglected tendo-Achilles rupture reconstruction using short flexor hallucis longus tendon transfer: a prospective review. Foot (Edinb) 22:219–223. https://doi.org/10.1016/j.foot.2012.05.004
Pinsker E, Daniels TR (2011) AOFAS Position Statement Regarding the Future of the AOFAS Clinical Rating Systems. Foot Ankle Int 32:841–842. https://doi.org/10.3113/FAI.2011.0841
Myerson MS (1999) Achilles tendon ruptures. Instr Course Lect 48:219–230
Den Hartog BD (2008) Surgical strategies: delayed diagnosis or neglected achilles’ tendon ruptures. Foot ankle Int 29:456–463. https://doi.org/10.3113/FAI.2008.0456
Kuwada G (1999) An update on repair of Achilles tendon rupture. Acute and delayed. J Am Podiatr Med Assoc 89:302–306. https://doi.org/10.7547/87507315-89-6-302
Krahe MA, Berlet GC (2009) Achilles tendon ruptures, re rupture with revision surgery, tendinosis, and insertional disease. Foot Ankle Clin 14:247–275. https://doi.org/10.1016/j.fcl.2009.04.003
Christensen I (1953) Rupture of the Achilles tendon; analysis of 57 cases. Acta Chir Scand 106(1):50–60
Ho G, Tantigate D, Kirschenbaum J et al (2017) Increasing age in Achilles rupture patients over time. Injury. https://doi.org/10.1016/j.injury.2017.04.007
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent for publication
All authors agree with the submission of this article to ‘international orthopaedics’.
Conflicts of interest
The senior author, Mr Maneesh Bhatia, is a member of the scientific committee of the European Foot and Ankle Society.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 20 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arshad, Z., Lau, E.J.S., Leow, S.H. et al. Management of chronic Achilles ruptures: a scoping review. International Orthopaedics (SICOT) 45, 2543–2559 (2021). https://doi.org/10.1007/s00264-021-05102-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05102-5