Abstract
Purpose
We present a systematic review of the recent literatures regarding the arthroscopic and open technique in fragment fixation for osteochondritis dissecans (OCD) of the humeral capitellum and an analysis of the subjective and objective outcomes between these two procedures.
Methods
PubMed and EMBASE were reviewed for suitable articles relating to fragment fixation for OCD, both open and arthroscopic. We included all studies reporting on the clinical outcomes of these two procedures that were published in the English language. Data extracted from each study included level of evidence, number of patients, surgical techniques, length of follow-up, clinical outcome measures including outcome scores, range of motion (ROM), return to sports, osseous union and complications. We analyzed each study to determine the primary outcome measurement.
Results
A total of ten studies met our inclusion criteria. Among all studies, 35 arthroscopic procedures and 107 open procedures were performed. After the procedure, 70 patients (86.4%) in the open group returned to their sports, and 32 patients (91.4%) in the arthroscopic group returned to their sports. In the arthroscopic group, patients gained 14.1 degrees of flexion and 9.5 degrees of extension after surgery. In the open group, patients gained 8 degrees of flexion and 5.7 degrees of extension. Five patients (4.7%) had complications in the open group. No complication was found in the arthroscopic group.
Conclusions
Both open and arthroscopic lesion debridement with fragment fixation are successful in treating unstable OCD. The arthroscopic technique may be a better choice than the open procedure, but we need high-level evidence to determine the superiority of the open or arthroscopic techniques in treating elbow OCD.
Level of evidence
Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteochondritis dissecans (OCD) of the humeral capitellum is one of the leading causes of elbow disability in adolescents who participate in throwing or weight-bearing sports. The aetiology of OCD is likely multi-factorial and has not been fully elucidated. Repetitive radiocapitellar compression and subsequent micro-trauma resulting from either a valgus or an axial load appears to be an essential component of the pathogenesis of elbow OCD [1]. It commonly presents as elbow pain in conjunction with swelling and limitation of range of motion (ROM) [2, 3]. The onset of pain is usually insidious and the symptoms may become worse with activity. The presence of mechanical locking is often a sign of more advanced cartilage injury or loose body formation in the elbow joint which needs to be operated upon [4].
An OCD classification was developed by Baumgarten and later was modified by the International Cartilage Repair Society (ICRS). Grade I lesions are stable with a continuous softened area covered by intact cartilage. Grade II lesions are stable on probing but exhibit partial discontinuity. Grade III lesions have complete discontinuity but are not dislocated. Grade IV lesions have an empty defect or a dislocated fragment lying within the bed [5]. For most stable lesions (grade I or II), the management usually starts with conservative treatment such as activity modification, rest, anti-inflammatory drugs and physiotherapy. Surgery is indicated for patients who fail non-operative treatment and those with unstable lesions [6]. The surgical treatments are variable, including debridement, drilling or micro-fracture, fragment fixation, and osteochondral autograft transplantation [1, 7,8,9,10]. Among them, the debridement with fragment fixation is a time-tested procedure and one of the most widely used methods for surgical treatment of unstable capitellum OCD [11,12,13,14,15].
With development of the arthroscopic technique, most surgeons have moved toward this method. In previous studies, good and excellent outcomes were reported [6, 16,17,18]. The advantages of the arthroscopic technique are that it is minimally invasive, is able to address concomitant intra-articular pathology, and provides early functional recovery and effective relief of pain [18]. In a previous study, Jones et al. reported that both the improvement in flexion and extension were statistically significant compared with the pre-operative ROM, and 86% of 25 patients returned to participate in their sport at their pre-injury level at a mean follow-up of 48 months [16]. Uchida et al. treated the unstable osteochondral lesion with internal fixation using absorbed thread pin, and their results were good [19]. Despite this recent progress in published data, there is an overall paucity of information on the advantage of arthroscopic compared to open surgery in the treatment of unstable OCD. The purpose of this study was to compare the subjective and objective outcomes between the arthroscopic and open procedure of fragment fixation for treating unstable OCD. The null hypothesis was that the open and arthroscopic procedures were equally effective.
Methods
This study was conducted according to the methods of the Cochrane Handbook [20] and is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [21].
Identification of studies
We performed a systematic review of the results of open and arthroscopic osteochondritis dissecans surgical debridement and fixation for the management of OCD lesions in PubMed and Embase databases between 1998 and 2016. The search strategy combined the following terms: “Osteochondritis Dissecans”, “osteochondral lesion” or “OCD”; “surgical treatments”, “debridement”, “fragment fixation”, “internal fixation”; “capitellum,” and “elbow”. Medical subject headings (MeSH) and Emtree headings and subheadings were used in various combinations in Ovid and supplemented with free text to increase sensitivity. A manual search of related references and cited articles was performed to identify any additional relevant studies for inclusion. Two reviewers independently screened the titles and abstracts of all studies for eligibility using piloted screening forms. Duplicate articles were manually excluded. Both reviewers considered the full text of all potentially eligible studies identified by title and abstract screening to determine final eligibility. All discrepancies were resolved by consensus decision.
Assessment of study eligibility
The inclusion criteria consisted of outcome studies of osteochondritis dissecans debridement combined with fragment fixation for OCD lesions, using either open or arthroscopic techniques. Additional inclusion criteria comprised studies with Level IV or higher evidence published in peer-reviewed journals in the English language. Case reports, diagnostic and prognostic studies, an abstract, a review article, surgical technique guide, imaging study, medical conference abstract, cadaveric study, or biomechanical study or Level V evidence studies were excluded from this review. Studies which included multiple surgical techniques and did not give the separated clinical outcomes were also excluded.
Data extraction and analysis
Data extracted from each study included level of evidence, number of patients, surgical techniques, length of follow-up, clinical outcome measures including outcome scores, ROM, return to sports, osseous union and complications. We analyzed each study to determine the primary outcome measurement used by the different authors.
We scored each scientific article using the ten criteria of the Coleman methodology score (CMS) system [22]. The Coleman scoring system is a method of analyzing the quality of the studies reviewed, and it is accurate and reproducible in systematic reviews. The CMS ranges from 0 to 100, and each article was scored independently by two authors, with the average value considered as the score of the article.
Descriptive statistics were calculated to reflect the frequency of outcome measures. The k (kappa) statistic was used to examine inter-observer agreement for study eligibility due to the guidelines of Landis and Koch [23]. A k(kappa) value of 0.81–1.00 indicates excellent agreement, 0.61–0.80 good agreement, 0.41–0.60 moderate agreement, 0.21–0.40 fair agreement, and 0–0.20 poor agreement. Inter-observer agreement for methodological quality assessment was calculated using the intra-class correlation coefficient. Both the k and intra-class correlation coefficient were calculated using SPSS statistical analysis software (IBM, Armonk, NY).
Results
Study identification
The literature search generated 288 relevant citations. After duplicate removal and application of eligibility criteria, 267 articles underwent title and abstract screening by two independent reviewers. A total of 111 articles underwent full-text review, ultimately producing ten articles that met the inclusion criteria of this report (Fig. 1) [1, 12,13,14, 17, 19, 24,25,26,27]. The k value for overall agreement between reviewers (YJ.L. and SY.G.) for the final eligibility decision was 0.86 (95% confidence interval, 0.67–1.00), indicating excellent agreement.
Study characteristics
There were three studies that evaluated the role of arthroscopic OCD treatment and ten studies that evaluated open OCD treatment.
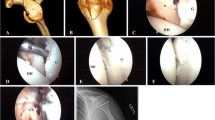
Among all studies, a total of 35 arthroscopic procedures and 107 open procedures were performed. All of the surgeons were experienced in either the arthroscopic procedure or the open procedure. The average age at the time of surgery was 14 years for the patients who underwent arthroscopic OCD treatment. For the patients who underwent open OCD treatment, the average age at the time of surgery was 14.3 years. Most of patients in the studies were male, with 91.4% in arthroscopic group and 89.8% in open group separately. In the arthroscopic group, 100% of the lesions were on the dominant side. In the open group, 93.5% of the lesions were on the dominant side. The mean follow-up period was 32.3 months for the arthroscopic group versus 48.2 months for the open OCD group. The outcomes of the studies were summarized in Table 1.
Study quality
All of the studies were Level IV evidence. Among the studies that evaluated arthroscopic OCD treatment, there was one prospective cohort study and the others were retrospective cohort studies. There were no prospective cohort studies in the open group, and all of the studies that evaluated open OCD treatment were retrospective cohort studies. The Coleman methodology score (CMS) for the included studies varied from 27 to 49, with a mean score of 35.3. In the arthroscopic group, the mean CMS was 37, and in the open group, the mean CMS was 34.6 (Table 1). The CMS was not statistically different between the two groups (P = 0.68). Agreement between reviewers in the assessment of study quality was good (intra-class correlation coefficient, 0.87; 95% confidence interval, 0.67–0.94).
Clinical results
All lesions of OCD in this study were grade II and above. In the arthroscopic group, the elbow flexion was 125.6 degree and extension was −10.4 degree on average pre-operatively. The elbow flexion increased to 139.7 degrees and extension to −0.9 degrees on average post-operatively. Patients gained 14.1 degrees of flexion and 9.5 degrees of extension on average. In the open group, the elbow flexion was 122.1 degrees and extension was −8.4 degrees on average pre-operatively. The elbow flexion became 130.1 degrees and extension −2.7 degrees on average post-operatively. Patients gained 8 degrees of flexion and 5.7 degrees of extension on average (Table 2). Although the improvement of ROM in the arthroscopic group is greater than that in the open group, the standard deviation of the elbow ROM in most papers was not mentioned, which means it is very difficult to make the comparison between the two groups.
The articles we reviewed used a variety of outcome measures, including Timmerman and Andrews scores, Tivnon’s score, Mayo Elbow scores, as well as the Disabilities of Arm, Shoulder and Hand score. The function score improvement is summarized in Table 3. After surgery, the function scores of the patients all significantly improved in both of the two groups. However, a comparison between the two groups was difficult because of the variety of outcome measures.
The overall rate of osseous union was 89.9%. In the open group, this rate was 87.4%. In the arthroscopic group, the value was 97.1%. There was no significant difference between the two groups (P = 0.117). In the arthroscopic group, the mean time to osseous union was 4.7 months, compared with 5.5 months in the open group. There is a trend toward a shorter time to osseous union in the arthroscopic group compared with the open group (Table 4).
Across all studies, 70 patients (86.4%) who underwent open procedures returned to their sports, and 32 patients (91.4%) who underwent arthroscopic procedures returned to their sports. There was no significant difference between the two groups (P = 0.45) (Table 4).
Five patients in the open group had complications and a second operation, two had surgical removal of symptomatic bioabsorbable implants, one had olecranon impingement requiring osteotomy, one had radiocapitellar plica debridement, and one had radial nerve palsy requiring decompression. No complication was found in the arthroscopic group. Although the complication rate in the open group is higher than that in the arthroscopic group (4.7% vs. 0%), this difference did not reach statistical significance (P = 0.548).
Discussion
Capitellar OCD is an intra-articular lesion and one of the leading causes of elbow disability. It may affect not only sports activities, but also activities of daily living. OCD occurs most commonly in young athletes who use their arms for throwing activities. In our review, all of the patients in the study were athletes, including such sports as baseball, gymnastics, handball, basketball, kendo, motocross and lacrosse. That is why most of the authors believed that repetitive micro-trauma and ischemia is the primary cause of OCD [2, 28].
In general, early-stage OCD or stable lesion on the joint can be managed non-operatively with good outcomes [5, 11]. In contrast, advanced OCD or unstable lesions generally require surgical management [10, 29]. A variety of surgical techniques for OCD have been reported in the literatures with satisfied outcomes, such as debridement, drilling, fragment removal, fragment fixation, and autologous osteochondral mosaicplasty [16, 26, 30,31,32,33]. Among these variety methods, fragment fixation should be considered when the fragment is amenable to being fixed. Several implants have been used to provide stable fixation with good function and 94–100% rate of healing, including Kirschner wires, cancellous screws, Herbert screws, pull-out wiring and bio-absorbable pins. In a large retrospective review, Takahara et al. reported significantly improved outcome in terms of pain in 12 patients treated with fragment fixation versus in 55 patients treated with open fragment excision alone (P < 0.05) [11]. The authors recommended bone peg fixation for all ICRS grade II lesions and fragment fixation with bone grafting for all ICRS grade III lesions. But much of the literature regarding surgical management describes open techniques. With the development of modern techniques in elbow arthroscopy, osteocondral fragment fixation can be performed with arthroscopic techniques.
Takeba et al. were the first to describe a method of arthroscopic osteochondral fixation using absorbable pins to treat OCD. In their 13 cases, good short-term results were obtained [24]. Nobuta et al. reported on 28 patients with a mean age of 22 years. They performed fragment fixation with a double-soft wire technique on the capitellar OCD site. In their series, 86% of the patients returned to their former level of sport and 89% were pain free post-operatively [27]. Koehler et al. performed arthroscopic all-inside suture fixation with iliac crest autogenous bone grafting on four patients with unstable capitellum OCD lesions. After a mean final follow-up of 2.8 years, union was achieved in all patients, and the results were satisfactory [17]. Although most authors considered the minimally invasive treatment as the desirable method to enable the patient to resume throwing activities early and to obtain good clinical results, there is no study till now to compare the fragment fixation outcomes between open and arthroscopic treatments.
The validated outcome scores showed a significant increase in both arthroscopic and open groups and were suggestive of good outcomes. Both of the two groups achieved osseous union in most of the patients. When comparing the rate of osseous union between the two groups, although no statistically significant difference was found (P = 0.10) in our study, there is a trend toward a higher rate of osseous union in the arthroscopic group compared with the open group (97.1% vs. 87.4%). Further, the mean time to osseous union was 4.72 months in the arthroscopic group and 5.5 months in the open group. As the arthroscopy procedure is a minimally-invasive technique that can protect the blood supply with less damage to soft tissue, it may provide a better environment for the osteochondral lesion to heal with earlier time.
Elbow ROM and function score were both improved in both of the two groups after the surgery. Uchida et al. performed arthroscopic fragment fixation on 18 adolescent baseball players with elbow OCD. In this study, T&A scores and MEPI were used as outcome measure. Post-operatively, T&A scores improved from 126.6 to 197.5, and MEPI improved from 68 to 98.06 [19]. Takeda et al. performed internal fixation with pull-out wiring and bone grafting on 11 male baseball players with unstable OCD lesions. After the surgery, the Tivnon’s evaluation was good or excellent in ten patients without poor outcome [1]. The differences in the clinical results between the two groups could be a reflection of the benefit of the arthroscopic procedure. However, since the articles we reviewed used a variety of outcome measures and most of the papers did not provide standard deviation of ROM, the statistical comparison between the two groups was not possible.
A high rate of return to sports was found in our study, which demonstrated good clinical outcomes after lesion debridement with fragment fixation. The overall rate of return to sports was 87.9% (66.7–100%), which means most patients were able to continue competing in their pre-injury levels by this treatment in the open or arthroscopic approach.
There were five complications in the open group and no complications in the arthroscopic group. Although this difference was not statistically significant, there is a trend toward a lower complication rate in the arthroscopic group. This can be another benefit of the arthroscopic procedure, which results in decreased postsurgical pain, reduced arthrofibrosis, easier post-operative rehabilitation, and improved intra-operative joint visualization [34,35,36,37]. With development of the arthroscopic technique, several procedures that once required open elbow arthrotomy are now commonly performed arthroscopically, such as OCD treatment. We did not find any complication in the arthroscopic group but the difference was not statistically significant. The main reason we believe this is due to small sample cases in each paper included in our study. With more clinical studies, the conclusion can be drawn further.
Our study presents some of the expected weaknesses of any systematic review. First, only Level IV studies were found in our review with small sample size. Most of the studies scored poorly in this section of the CMS. Only one study was constructed as a prospective cohort study, and all of the other studies were retrospective cohort studies. In addition, most of studies had low power, lacked randomization or the inclusion of a control group, and used different outcome measures, which made the results less comparative. However, when comparing the CMS between the open and arthroscopic groups, there were no clinical or statistical differences (P = 0.68). Second, in the present review, the characteristics of the patients in both the arthroscopic and open groups were not equivalent. The average age at the time of surgery was significantly older in the arthroscopic group compared with the open group. Significant differences were also found in the gender ratio and the ratio of dominant arm injured. This asymmetry in characteristics of the patients may cause a risk of bias. Third, too many different methods were used for functional assessment, due to the lack of standardized outcome criteria. In addition, the time of outcome assessment was not clearly stated in some studies. Last but not least, some the studies did not contain the standard deviation of elbow ROM and time to osseous union, which makes the comparison between the two groups not possible.
Conclusion
Both open and arthroscopic lesion debridement with fragment fixation are successful in treating unstable OCD. The arthroscopic technique may be a better choice than the open procedure, but we need high-level evidence to determine the superiority of the open or arthroscopic techniques in treating elbow OCD.
References
Takeda H, Watarai K, Matsushita T, Saito T, Terashima Y (2002) A surgical treatment for unstable osteochondritis dissecans lesions of the humeral Capitellum in adolescent baseball players. Am J Sports Med 5:713–717. https://doi.org/10.1177/03635465020300051501
Schenck RC Jr, Goodnight JM (1996) Osteochondritis dissecans. J Bone Joint Surg Am 78:439–456
Stubbs MJ, Field LD (2001) Osteochondritis dissecans of the elbow. Clin Sports Med 20:1–9
Smith MV, Bedi A, Chen NC (2012) Surgical treatment for osteochondritis dissecans of the capitellum. Sports Health 4:425–432. https://doi.org/10.1177/1941738112444707
Ruchelsman DE, Hall MP, Youm T (2010) Osteochondritis dissecans of the capitellum: current concepts. J Am Acad Orthop Surg 18:557–567. https://doi.org/10.5435/00124635-201009000-00007
Brownlow HC, O’Connor-Read LM, Perko M (2006) Arthroscopic treatment of osteochondritis dissecans of the capitellum. Knee Surg Sports Traumatol Arthros 14:198–202. https://doi.org/10.1007/s00167-005-0623-z
Byrd JW, Jones KS (2002) Arthroscopic surgery for isolated Capitellar Osteochondritis Dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med 30:474–478. https://doi.org/10.1177/03635465020300040401
Iwasaki N, Kato H, Ishikawa J, Masuko T, Funakoshi T, Minami A (2009) Autologous osteochondral mosaicplasty for osteochondritis dissecans of the elbow in teenage athletes. J Bone Joint Surg Am 91:2359–2366. https://doi.org/10.2106/JBJS.H.01266
Maruyama M, Takahara M, Harada M, Satake H, Takagi M (2014) Outcomes of an open autologous osteochondral plug graft for capitellar osteochondritis dissecans: time to return to sports. Am J Sports Med 42:2122–2127. https://doi.org/10.1177/0363546514538759
Yamamoto Y, Ishibashi Y, Tsuda E, Sato H, Toh S (2006) Osteochondral autograft transplantation for osteochondritis dissecans of the elbow in juvenile baseball players: minimum 2-year follow-up. Am J Sports Med 34:714–720. https://doi.org/10.1177/0363546505282620
Takahara M, Mura N, Sasaki J, Harada M, Ogino T (2007) Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am 89:1205–1214
Kuwahata Y, Inoue G (1998) Osteochondritis dissecans of the elbow managed by Herbert screw fixation. Orthopedics 21:449–451
Oka Y, Ohta K, Fukuda H (1999) Bone-peg grafting for osteochondritis dissecans of the elbow. Int Orthop 23:53–57
Harada M, Ogino T, Takahara M, Ishigaki D, Kashiwa H, Kanauchi Y (2002) Fragment fixation with a bone graft and dynamic staples for osteochondritis dissecans of the humeral capitellum. J Shoulder Elb Surg 11:368–372. https://doi.org/10.1067/mse.2002.123900
Chambers HG, Shea KG, Carey JL (2011) AAOS clinical practice guideline: diagnosis and treatment of osteochondritis dissecans. J Am Acad Orthop Surg 19:307–309
Jones KJ, Wiesel BB, Sankar WN, Ganley TJ (2010) Arthroscopic management of osteochondritis dissecans of the capitellum: mid-term results in adolescent athletes. J Pediatr Orthop 30:8–13. https://doi.org/10.1097/BPO.0b013e3181c3be83
Koehler SM, Walsh A, Lovy AJ, Pruzansky JS, Shukla DR, Hausman MR (2015) Outcomes of arthroscopic treatment of osteochondritis dissecans of the capitellum and description of the technique. J Shoulder Elb Surg 24:1607–1612. https://doi.org/10.1016/j.jse.2015.06.013
Ruch DS, Cory JW, Poehling GG (1998) The arthroscopic management of osteochondritis dissecans of the adolescent elbow. Arthroscopy 14:797–803
Uchida S, Utsunomiya H, Taketa T, Sakoda S, Hatakeyama A, Nakamura T, Sakai A (2015) Arthroscopic fragment fixation using hydroxyapatite/poly-L-lactate acid thread pins for treating elbow osteochondritis dissecans. Am J Sports Med 43:1057–1065. https://doi.org/10.1177/0363546515570871
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews for interventions, version 5.1.0. The Cochrane Collaboration, London
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med 3:e123–e130
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports 10:2–11
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Takeba J, Takahashi T, Watanabe S, Imai H, Kikuchi S, Umakoshi K, Matsumoto H, Ohshita M, Miura H, Aibiki M (2015) Short-term clinical results of arthroscopic osteochondral fixation for elbow osteochondritis dissecans in teenaged baseball players. J Shoulder Elb Surg 24:1749–1756. https://doi.org/10.1016/j.jse.2015.07.009
Hennrikus WP, Miller PE, Micheli LJ, Waters PM, Bae DS (2015) Internal fixation of unstable in situ osteochondritis dissecans lesions of the capitellum. J Pediatr Orthop 35:467–473. https://doi.org/10.1097/BPO.0000000000000308
Mihara K, Suzuki K, Makiuchi D, Nishinaka N, Yamaguchi K, Tsutsui H (2010) Surgical treatment for osteochondritis dissecans of the humeral capitellum. J Shoulder Elb Surg 19:31–37. https://doi.org/10.1016/j.jse.2009.04.007
Nobuta S, Ogawa K, Sato K, Nakagawa T, Hatori M, Itoi E (2009) Clinical outcome of fragment fixation for osteochondritis dissecans of the elbow. Ups J Med Sci 113:201–208. https://doi.org/10.3109/2000-1967-232
Nagura S (1960) The so-called osteochondritis dissecans of Konig. Clin Orthop 18:100–122
Matsuura T, Kashiwaguchi S, Iwase T, Takeda Y, Yasui N (2008) Conservative treatment for osteochondritis of the humeral capitellum. Am J Sports Med 36:868–872. https://doi.org/10.1177/0363546507312168
Kosaka M, Nakase J, Takahashi R, Toratani T, Ohashi Y, Kitaoka K, Tsuchiya H (2013) Outcomes and failure factors in surgical treatment for osteochondritis dissecans of the capitellum. J Pediatr Orthop 33:719–724. https://doi.org/10.1097/BPO.0b013e3182924662
Iwasaki N, Kato H, Ishikawa J, Saitoh S, Minami A (2006) Autologous osteochondral mosaicplasty for capitellar osteochondritis dissecans in teenaged patients. Am J Sports Med 34:1233–1239. https://doi.org/10.1177/0363546506286343
Miyake J, Masatomi T (2011) Arthroscopic debridement of the humeral capitellum for osteochondritis dissecans: radiographic and clinical outcomes. J Hand Surg 36:1333–1338. https://doi.org/10.1016/j.jhsa.2011.05.024
Bojanić I, Smoljanović T, Dokuzović S (2012) Osteochondritis dissecans of the elbow: excellent mid-term follow-up results in teenage athletes treated by arthroscopic debridement and microfracture. Croat Med J 53:40–47. https://doi.org/10.3325/cmj.2012.53.40
Leong NL, Cohen JR, Lord E, Wang JC, McAllister DR, Petrigliano FA (2015) Demographic trends and complication rates in arthroscopic elbow surgery. Arthroscopy 31:1928–1932
Elfeddali R, Schreuder MHE, Eygendaal D (2013) Arthroscopic elbow surgery, is it safe? J Shoulder Elb Surg 22:647–652
Kelly EW, Morrey BF, O’Driscoll SW (2001) Complications of elbow arthroscopy. J Bone Joint Surg Am 83:25–34
Nelson GN, Wu T, Galatz LM, Yamaguchi K, Keener JD (2014) Elbow arthroscopy: early complications and associated risk factors. J Shoulder Elb Surg 23:273–278
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no competing interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lu, Y., Li, Y.J., Guo, S.Y. et al. Is there any difference between open and arthroscopic treatment for osteochondritis dissecans (OCD) of the humeral capitellum: a systematic review and meta-analysis. International Orthopaedics (SICOT) 42, 601–607 (2018). https://doi.org/10.1007/s00264-018-3768-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3768-3