Abstract
Background
The combination of immune checkpoint inhibitors and antiangiogenic agents has been effective in treating multiple cancers. This was further explored in an open-label, multicenter phase 2 basket study (NCT04346381), which evaluated the antitumor activity and safety of camrelizumab (an anti-PD-1 antibody) plus famitinib (a receptor tyrosine kinase inhibitor) in patients with advanced solid tumors. We herein report the findings from the cohort of advanced NSCLC patients who progressed after treatment with platinum-doublet chemotherapy and immunotherapy.
Methods
Eligible patients were enrolled and treated with camrelizumab (200 mg once every 3 weeks via intravenous infusion) and oral famitinib (20 mg once daily). The primary endpoint was the objective response rate (ORR). Secondary endpoints included the disease control rate (DCR), duration of response (DoR), progression-free survival (PFS), overall survival (OS), and safety.
Results
Forty patients were enrolled in this cohort, with a median follow-up duration of 11.5 months. Three patients (7.5%) achieved a partial response, and 29 patients (72.5%) achieved stable disease. The ORR and DCR with this combination regimen were 7.5% (95% CI, 1.6–20.4) and 80.0% (95% CI, 64.4–90.9), respectively. The median DoR was 12.1 months (95% CI, 10.3-not reached). The median PFS was 5.4 months (95% CI, 4.1–7.5), and the median OS was 12.1 months (95% CI, 9.1–16.7). The estimated 12-month OS rate was 51.5% (95% CI, 34.9–65.9). The most frequent grade 3 or higher treatment-related adverse events occurring in more than 5% of patients included hypertension (27.5%), palmar-plantar erythrodysesthesia syndrome (10%), decreased neutrophil count (10%), and proteinuria (7.5%).
Conclusion
Camrelizumab plus famitinib demonstrated favorable benefits in PFS and OS, along with manageable safety profiles, in patients with advanced NSCLC who progressed after platinum-doublet chemotherapy and immunotherapy. This finding warrants further exploration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The emergence of checkpoint inhibitors (ICIs), specifically monoclonal antibodies targeting programmed cell death 1 (PD-1) and its ligand (PD-L1), has revolutionized the therapeutic landscape for advanced non-small cell lung cancer (NSCLC) in cases without targetable driver mutations [1]. Although first-line ICIs, either alone or in combination with chemotherapy, have achieved extraordinary results in treating this patient population, the majority of them ultimately develop resistance to immunotherapy. However, even though the phase 3 REVEL [2] and LUME-Lung 1 trials [3] established the role of ramucirumab plus docetaxel (for all histology) and nintedanib in combination with docetaxel (only for adenocarcinoma histology) as second-line treatments in advanced NSCLC, the benefits of these regimens were marginal, with a median overall survival (OS) prolongation of about 1.4 months. Currently, single-agent docetaxel remains the standard option for patients with advanced NSCLC who progress after first-line platinum-doublet chemotherapy [4,5,6,7], yet it yields unsatisfactory clinical outcomes, with an objective response rate (ORR) of approximately 10% and a median OS of about 10 months. Therefore, novel and effective treatment options for pretreated NSCLC patients remain an unmet need in this setting.
Previous studies have shown that antiangiogenic agents can alleviate hypoxia in the tumor microenvironment (TME), promote the infiltration of immune CD8 + T cells, and enhance the efficacy of immunotherapy [8,9,10]. Lung-MAP S1800A, a phase 2 randomized trial, has reported that the combination of pembrolizumab and ramucirumab significantly prolonged OS compared to the docetaxel plus ramucirumab regimen [11]. In addition, the CONTACT 01 phase 3 trial investigated the efficacy and safety of atezolizumab combined with cabozantinib, compared to docetaxel monotherapy, in patients with metastatic NSCLC who had previously been treated with checkpoint inhibitors and chemotherapy. The trial observed a trend toward OS prolongation with a hazard ratio (HR) of 0.88, indicating the potential of antiangiogenesis to overcome resistance to immunotherapy [12]. Furthermore, another ongoing phase 3 trial (LEAP-008, NCT03976375) is evaluating the efficacy and safety of pembrolizumab plus lenvatinib compared to docetaxel in the treatment of NSCLC previously treated with chemo-immunotherapy [13].
The anti-PD-1 antibody camrelizumab, in combination with chemotherapy, has become the standard first-line regimen in China for patients with advanced NSCLC without EGFR or ALK genomic tumor aberrations [14, 15]. Famitinib (SHR1210), a novel and promising multitargeted tyrosine kinase inhibitor (TKI), inhibits the activity of c-kit, VEGFR-2, and PDGFRβ [16]. Previously, the combination of camrelizumab and famitinib has shown potent antitumor activity and tolerability in patients with advanced gynecologic and genitourinary malignancies [17,18,19]. Therefore, a basket phase 2 trial was initiated to further evaluate the efficacy and safety of the combination of camrelizumab and famitinib in various solid tumors. In this study, we report the results from cohort 7, which consisted of patients with advanced NSCLC who progressed after treatment with platinum-doublet chemotherapy and immunotherapy.
Materials and methods
Study design and patients
This is an open-label, multicentre, phase 2 basket study (NCT04346381, registered April 15, 2020) of camrelizumab plus famitinib for the treatment of patients with advanced solid tumors. Here, we present the data from cohort 7, consisting of patients with advanced NSCLC, previously treated with chemo-immunotherapy, regardless of histology type (squamous or non-squamous). Eligible patients had recurrent or metastatic NSCLC, confirmed by pathology or cytology, with wild-type EGFR and ALK. They were previously treated with platinum-doublet chemotherapy and anti-PD-1 or anti-PD-L1 agents (either combined or sequentially) and had progressed after no more than two lines of systemic therapy. Patients also met the following inclusion criteria: (1) age between 18 and 75 years; (2) Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1; (3) at least one measurable lesion as defined by the Response Evaluation Criteria in Solid Tumors (RECIST) v1.1; (4) a life expectancy of no less than 12 weeks, and 5) adequate organ function. The key exclusion criteria for this cohort were as follows: (1) any active autoimmune diseases or a history of such diseases; (2) concurrent use of immune-suppressants or systemic corticosteroids for immunosuppression within 2 weeks prior to the first dose of the study treatment; (3) poorly controlled hypertension; (4) untreated central nervous system metastases; (5) clinically significant cardiovascular disease; (6) concurrent treatment with anticoagulation therapies or a tendency for bleeding; (7) radiographic imaging indicating tumor invasion of a major blood vessel, unclear boundary with a blood vessel, or cavitation in lung lesions that might cause fatal bleeding, as determined by the investigator; (8) history of pulmonary embolism, stroke, or deep venous thrombosis within 6 months prior to the first dose of the study treatment; (9) active infection; or (10) diagnosis of other malignancies within the past 5 years.
This trial was conducted in strict adherence to the Declaration of Helsinki, Good Clinical Practice guidelines, and applicable local laws and regulatory requirements. The study protocol, along with any amendments, received approval from the independent Institutional Review Board or ethics committee at each participating study site. All participating patients provided their written informed consent. This trial was registered with ClinicalTrials.gov, number NCT04346381.
Procedures
All patients enrolled in cohort 7 received a fixed dose of camrelizumab 200 mg via intravenous infusion over 30–60 min once every 3 weeks (Q3W) on Day 1 of each 3-week treatment cycle, and oral famitinib, at a starting dose of 20 mg once daily (QD), before or after a meal. Study treatment was continued until the occurrence of any of the following: intolerable toxicity, confirmed disease progression as per RECIST v1.1, decision by the investigator or patient, withdrawal of consent, poor adherence, or loss to follow-up, whichever came first. Patients with initial documented evidence of disease progression based on RECIST v1.1 could continue receiving study treatment if the investigator assessed the treatment as tolerable and providing clinical benefit. The study treatment was to continue until the next radiological confirmation of disease progression at least 4 weeks later. For camrelizumab, dose modifications were not permitted; however, dose interruptions of up to 12 weeks were allowed. The total duration of camrelizumab exposure should not exceed 24 months. Dose modifications of famitinib were permitted, including dose interruption, dose reduction (from the starting dose of 20 mg once daily to 15 mg once daily), and alteration in the dosing schedule to a 14 days on-7 days off regimen. However, once reduced or altered, the famitinib dose or dosing frequency could not be resumed to the original schedule.
Endpoints
The primary endpoint was the ORR, as assessed by the investigator according to RECIST v1.1. ORR was defined as the proportion of patients whose best overall response (BOR) included either a confirmed complete response (CR) or a partial response (PR). Secondary endpoints included disease control rate (DCR), duration of response (DoR), time to treatment response (TTR), progression-free survival (PFS), OS, 6-, 9-, and 12-month OS rates, as well as the safety profile. DCR was defined as the proportion of patients whose BOR was either a CR, PR, or durable stable disease (SD). DoR was defined as the time from the first documented objective response until the first radiographic documentation of disease progression or death from any cause, whichever occurred first. PFS was defined as the time from the first dose of study treatment until the first documented disease progression per RECIST v1.1 or death from any cause, whichever occurred first. OS was defined as the time from the first dose of the study treatment until death from any cause. Exploratory endpoints involved exploring the correlations between efficacy (ORR and PFS) and potential biomarkers, such as PD-L1 tumor proportion score (TPS) and total tumor mutational burden (tTMB).
Assessments
Tumor response assessments, per RECIST v1.1, were initially conducted at baseline and then every 9 weeks, as determined by the investigator's discretion. The first documentation of a CR or PR needed to be confirmed at least 4 weeks later. Additionally, an imaging examination was required for the confirmation of disease progression ≥ 4 weeks after the initial documented radiographic disease progression per RECIST v1.1, except in cases of rapid radiological or clinical progression. For patients who discontinued study treatment without radiological evidence of disease progression, tumor response assessment was performed every 3 months until documented disease progression, initiation of first subsequent anti-cancer therapy, loss to follow-up, death, or study termination by the sponsor, whichever occurred first. The survival status of patients was monitored and collected through clinical or remote follow-ups every 2 months until death. Safety evaluations included the monitoring of adverse events (AEs), measurement of vital signs, clinical laboratory tests, and 12-lead electrocardiogram assessments. AEs were recorded and monitored until at least 30 days after the last dose of study treatment. Patients were monitored for serious AEs and immune-mediated AEs until 90 days after the last dose of camrelizumab. The severity of AEs was assessed and graded based on the NCI Common Terminology Criteria for Adverse Events, version 5.0.
PD-L1 expression was obtained from some patients in clinical practice and measured using the IHC 22C3 pharmDx kit (Agilent Technologies, Santa Clara, CA). PD-L1 positivity was defined as a TPS of 1% or higher. TMB measurement in pretreatment tumor biopsy or archival tissue was typically conducted using the BGI Oseq pancancer panel, which covers 636 genes and 1.95 Mb, on the MGISEQ-2000 platform developed by MGI Tech Co. Ltd. (a subsidiary of the BGI Group). TMB was defined as the total number of somatic, coding, base substitutions, and indel mutations per megabase of the genome examined, and it was classified into TMB-high (≥ 10 mutations/Mb) and TMB-low (< 10 mutations/Mb) categories [20, 21].
Statistical analyses
In the cohort 7, the desirable target ORR was set at 25%, while the uninteresting level of ORR under the null hypothesis was set at 10%. Based on these assumptions, with a one-sided α-error of 5% and a power of 70%, cohort 7 required the treatment of 19 evaluable patients during stage I. Stage II would proceed if at least 2 responders were obtained during stage I, subsequently involving the treatment of an additional 8 evaluable patients. Overall, the combination regimen would be considered active if 6 or more responders were observed among the 27 patients. In cohort 7, 2 out of the 19 patients enrolled in stage I achieved objective responses, and the actual sample size for the stage 2 was 21 patients. Overall, if a total of 9 or more responders were observed during the entire study period, the combination regimen in cohort 7 would be considered active. This critical value was estimated using the method described by Koyama and Chen [22].
Efficacy analyses were performed in all enrolled patients who had received at least one dose of study treatment, defined as the full analysis set (FAS). Safety was assessed in all patients who had received at least one study treatment and had at least one post-baseline safety evaluation. ORR and DCR, along with their 95% confidence intervals (CIs), were calculated using the Clopper-Pearson exact method based on the binomial distribution. The medians of time-to-event endpoints (DoR, PFS, and OS) were calculated using the Kaplan–Meier method, with their 95% CIs estimated using the Brookmeyer-Crowley method. The Kaplan–Meier method was used to estimate the OS probabilities at 6, 9, and 12 months. The corresponding 95% CIs were calculated using the log–log transformation (based on the normal approximation method) with back transformation to a CI on the untransformed scale. TTR was summarized using median, minimum and maximum. All statistical analyses were conducted using SAS, version 9.4.
Results
Patients
Between September 4, 2020, and July 12, 2021, a total of 40 patients with advanced NSCLC, who had previously been treated with platinum-doublet chemotherapy and ICIs (anti-PD-1 or anti-PD-L1) and progressed after ≤ 2 lines of systemic therapy, were enrolled in cohort 7 from 12 study centers in China. All patients enrolled in this cohort were treated with the combination regimen of camrelizumab plus famitinib and included in both the full analysis set and the safety analysis set.
The baseline demographics and clinical characteristics of patients are shown in Table 1. The median age of the patients was 62 years (range, 41–73), 90% (36/40) of whom were male, and 67.5% (27/40) were current or former smokers. The majority of patients had an ECOG PS of 1 (36/40; 90%). Regarding histology, 23 (57.5%) patients had non-squamous carcinomas, and 17 (42.5%) had squamous carcinomas. Thirty-nine (97.5%) patients had metastases irrespective of the organs involved, with brain metastasis observed in 2 (5.0%) and liver metastases in 3 (7.5%) patients. Additionally, 17 patients (42.5%) had received two prior lines of systemic therapy.
According to laboratory assessment, tumor PD-L1 expression data were available for 38 patients; of these, 11 (27.5%) patients had a PD-L1 TPS of ≥ 1%, and 5 (12.5%) patients had a PD-L1 TPS of ≥ 50%. As of the cutoff date (June 22, 2022), the median follow-up duration was 11.5 months (range, 1.7–18.1). Among the 40 patients, 2 (5.0%) were still receiving study treatment at the time of analysis. The reasons for discontinuing treatment with camrelizumab or famitinib included disease progression (either radiographic or clinic) in 27 (67.5%) patients, AEs in 3 (7.5%) patients, death in 3 (7.5%) patients, patient withdrawal in 3 (7.5%) patients, and protocol violations in 2 (5.0%) patients (Fig. 1).
Anti-tumor activity in all patients
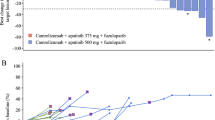
Among the 40 patients in the FAS, 3 (7.5%) achieved a PR, and 29 (72.5%) achieved SD as their best response. The confirmed ORR and DCR with this combination regimen were 7.5% (95% CI, 1.6–20.4) and 80.0% (95% CI, 64.4–90.9), respectively (Table 2). Overall, the best change in the sum of diameter of target lesion from baseline for each patient is plotted in Fig. 2A, with a decrease in tumor burden observed in 26 (65.0%) patients. Tumor responses since the initial dose of the study treatment, as shown in Fig. 2B, indicated that reductions in tumor burden were observed over several assessments. The median TTR was 2.1 months (range, 2.0–2.1), and the median DoR was 12.1 months (95% CI, 10.3-not reached [NR]; Fig. 2C).
Antitumor activity of camrelizumab plus famitinib in cohort 7 patients. A Best percentage change from baseline in the size of target lesions. Red asterisks indicated confirmed responses. B Percentage change in the tumor burden of the target lesion from baseline over time. C Treatment response and duration of response
At the data cutoff, 34 (85.0%) patients experienced events of investigator-assessed disease progression or death. The median PFS, estimated using the Kaplan–Meier method, was 5.4 months (95% CI, 4.1–7.5; Fig. 3A). The 6-, 9-, and 12-month PFS rates were 47.8% (95%CI, 31.4–62.5), 19.7% (95% CI, 8.7–33.8), and 13.5% (95% CI, 4.7–26.9), respectively. In cohort 7, a total of 24 patients (60.0%) had died. The median OS was 12.1 months (95% CI, 9.1–16.7; Fig. 3B), with the Kaplan–Meier estimated 6-, 9-, and 12-month OS rates being 80.0% (95% CI, 64.0–89.5), 67.5% (95% CI, 50.7–79.7), and 51.5% (95% CI, 34.9–65.9), respectively.
Anti-tumor activity by PD-L1 TPS or tTMB status
Anti-tumor activity outcomes by PD-L1 TPS or tTMB are shown in the Table S1. Among the 40 patients, 38 (95.0%) had available data on tumor PD-L1 expression. The ORR was 7.4% (95% CI, 0.9–24.3) in 27 patients with PD-L1 TPS < 1% vs. 9.1% (95% CI, 0.2–41.3) in 11 patients with PD-L1 TPS ≥ 1%. The median PFS was 5.3 months (95% CI, 4.1–8.3) for patients with PD-L1 TPS < 1%, and 6.1 months (95% CI, 1.7-NR) for those with PD-L1 TPS ≥ 1%. TMB data were available for 24 (60.0%) of the patients, among whom 7 had low tTMB (< 10 mutations/Mb) and 17 had high tTMB (≥ 10 mutations/Mb). Subgroup analysis revealed an ORR of 0% (95% CI, 0.0–41.0) in patients with low tTMB compared to 11.8% (95% CI, 1.5–36.4) in those with high tTMB. The median PFS was 5.3 months (95% CI, 0.7–7.7) for patients with low tTMB and 6.2 months (95% CI, 3.5–12.4) for those with high tTMB.
Safety
The median duration of exposure to camrelizumab was 5.9 months (range, 0.7–17.2), with a relative dose intensity of 99.6% (range, 66.7–108.6). The median duration of exposure to famitinib was 5.4 months (range, 0.4–17.0), with a median relative dose intensity of 82.4% (range, 52.0–100.0).
Thirty-eight patients experienced one or more TRAEs of any grade (Table 3), with the most frequent TRAEs being decreased platelet count (n = 24, 60.0%), hypertension (n = 23, 57.5%), proteinuria (n = 22, 55.0%), and decreased neutrophil count (n = 21, 52.5%). Twenty-six (60.0%) patients had grade 3 or higher TRAEs, with the most frequent occurring in more than 5% of patients being hypertension (n = 11, 27.5%), palmar-plantar erythrodysesthesia syndrome (n = 4, 10%), decreased neutrophil count (n = 4, 10%), and proteinuria (n = 3, 7.5%). Reactive cutaneous capillary endothelial proliferation (RCCEP), a clinically manageable and self-resolving TRAE associated with camrelizumab monotherapy, occurred in only one patient (2.5%, grade 1) of this cohort treated with the combination of camrelizumab and famitinib.
In cohort 7, serious TRAEs of grade 3 or higher occurred in 9 (22.5%) patients, including increased alanine aminotransferase, hemoptysis, sudden death, acute kidney injury, renal impairment, herpes zoster, urinary tract infection, pneumonia fungal, drug-induced liver injury, cerebral infarction, cerebral hemorrhage, arthralgia, hyperthyroidism, and hypertension (n = 1 for each; 2.4%) (Table S2. Four (10.0%) deaths were considered as treatment-related, including one sudden death, one hemoptysis, one from cerebral infarction and cerebral hemorrhage, and one from acute kidney injury and drug-induced liver injury.
Three (7.5%) patients discontinued camrelizumab due to TRAEs, which included cerebral hemorrhage, cerebral infarction, acute kidney injury, urinary tract infection, renal impairment, and drug-induced liver injury (n = 1 for each, 2.5%). Three (7.5%) patients discontinued famitinib because of TRAEs that were cerebral infarction, cerebral hemorrhage, acute kidney injury, renal impairment, and drug-induced liver injury (n = 1 for each, 2.5%). TRAEs leading to dose interruption or dose modification (of famitinib) are shown in the Table S3. Eleven (27.5%) patients experienced at least one TRAE leading to camrelizumab interruption, with increased alanine aminotransferase (n = 3, 7.5%) and increased aspartate aminotransferase (n = 2, 5.0%) occurring in more than one patient. Dose interruptions of famitinib due to TRAEs occurred in 26 (65.0%) patients, with proteinuria (n = 6, 15.0%), decreased platelet count (n = 6, 15.0%), decreased white blood cell count (n = 5, 12.5%), hypertension (n = 4, 10.0%), and decreased neutrophil count (n = 3, 7.5%) occurring in more than 2 patients. TRAEs leading to dose reduction of famitinib were reported in 19 (47.5%) patients, with palmar-plantar erythrodysesthesia (PPE) syndrome (n = 4, 10.0%), decreased platelet count decreased (n = 3, 7.5%), proteinuria (n = 3, 7.5%), and decreased neutrophil count (n = 3, 7.5%) occurring in more than 2 patients. Five (12.5%) patients experienced at least one TRAE leading to a reduction in the dose frequency of famitinib, including increased alanine aminotransferase, hypercholesterolemia, hypertriglyceridemia, PPE syndrome, decreased white blood cell count, and proteinuria (n = 1 for each, 2.5%).
Immune-mediated AEs of any grade, regardless of attribution to study treatment as assessed by investigators, were observed in 5 (12.5%) patients (Table S4). These AEs included hypothyroidism (n = 2, 5.0%), hyperthyroidism, drug-induced liver injury, increased alpha hydroxybutyrate dehydrogenase, increased blood creatine phosphokinase, increased blood lactate dehydrogenase, and interstitial lung disease (n = 1 for each, 2.5%).
Discussion
We report for the first time on the antitumor activity and safety profile of the combination of camrelizumab and famitinib in patients with advanced NSCLC, who had progressed after treatment with platinum-doublet chemotherapy and immunotherapy. Although the primary endpoint of antitumor activity, indicated by an ORR of 7.5%, was not met, this combination regimen demonstrated meaningful clinical benefits in secondary endpoints, including PFS and OS. These findings suggest the potential efficacy of camrelizumab and famitinib for this specific group of patients with advanced NSCLC.
In this cohort, the median PFS and OS were 5.4 months and 12.1 months, respectively, with a 12-month OS rate of 51.5%. Interestingly, despite potential issues in cross-trial comparisons due to heterogeneous populations and varying study designs, the median PFS observed with camrelizumab plus famitinib was numerically longer than that achieved with docetaxel alone (2.8–4.2 months) [2, 4,5,6,7], and ramucirumab plus docetaxel (4.5 months) [2], in similar clinical settings. Moreover, the median OS in this cohort appeared to be more favorable than that achieved with docetaxel alone (6.0–9.6 months) [2, 4,5,6,7], and was comparable to the OS observed with ramucirumab plus docetaxel (10.5 months) [2]. Notably, a considerable proportion of patients enrolled in this cohort exhibited fragility due to heavy pretreatment, with 42.5% having received two prior lines of systemic therapy and receiving this combination regimen as third-line therapy. Therefore, our findings suggest that this combination regimen can provide an impressive survival benefit (both PFS and OS) in this patient population.
PD-L1 expression and TMB have emerged as promising biomarkers for response to ICI monotherapy in NSCLC [14, 20, 23,24,25]. In this cohort, we observed a numerically higher ORR (9.1% vs. 7.4%) and a slightly prolonged median PFS (6.1 vs. 5.3 months) in patients with a PD-L1 TPS of ≥ 1% compared to those with a PD-L1 TPS of < 1%. Furthermore, patients with high tTMB (≥ 10 mutations/Mb) achieved a better ORR (11.8% vs. 0%) and longer median PFS (6.2 vs. 5.3 months) than those with low tTMB (< 10 mutations/Mb). These findings suggest that adding antiangiogenic TKIs to anti-PD-1 immunotherapy may restore ICI sensitivity in patients of this cohort, particularly for those with a PD-L1 TPS of ≥ 1% or high genome instability. However, the interpretation of the correlation between these biomarkers and efficacy should be approached with caution due to the exploratory nature of the analyses and the limited number of patients in the subgroups, especially when compared to similar studies.
In this cohort, the overall incidence rate of grade 3 or higher TRAEs with camrelizumab plus famitinib was comparable to those reported in trials of advanced or metastatic urothelial carcinoma, ovarian cancer, or renal cell carcinoma [17,18,19], and no new safety signals were detected. The most common grade 3 or higher TRAEs observed with this combination treatment included hypertension, proteinuria, and PPE syndrome. These TRAEs might be related to famitinib [26,27,28] and are representative of the anti-angiogenic effects of VEGF/VEGFR TKIs [29, 30]. Meanwhile, RCCEP, a common skin adverse reaction caused by camrelizumab monotherapy, occurred in approximately 67–97% of patients with various advanced solid tumors [31]. However, in this cohort, the incidence of RCCEP with the combination of camrelizumab and famitinib was only 2.5%, significantly lower than that reported with camrelizumab monotherapy. These results aligned with previous findings involving camrelizumab combined with VEGFR TKIs [17,18,19, 32,33,34]. As a result of this combination regimen, there was a slight increase in the incidence of TRAEs leading to a dose reduction of famitinib (n = 19, 47.5%; of these, 5 patients experienced TRAEs necessitating modification in the famitinib dose frequency). Despite this, the rate of discontinuation due to TRAEs was low (5.0% for camrelizumab and 7.5% for famitinib), which might contribute to the favorable PFS and OS benefits observed in this study.
The current study has several potential limitations. First, the trial was constrained by its exploratory nature as a single-arm phase 2 design, lacking a control arm of either docetaxel or ICI monotherapy. Consequently, further prospective randomized controlled trials are necessary. Second, there is a potential for inherent bias based on the investigator’s assessment of the ORR and PFS. Third, some patients had non-evaluable samples for PD-L1 or tTMB analysis, as providing these samples was not a mandatory requirement for enrollment. Therefore, identifying predictive biomarkers to select suitable candidates for the combination of antiangiogenic agents and immunotherapy in this clinical setting still needs to be addressed.
Conclusions
The combination of camrelizumab and famitinib resulted in acceptable PFS and OS benefits which warrants further investigations; safety issues emerged in this cohort highlighting the need to explore predictive factors for serious AEs when combining antiangiogenic agents and ICIs in pretreated NSCLC patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AE:
-
Adverse event
- CI:
-
Confidence interval
- CR:
-
Complete response
- DCR:
-
Disease control rate
- DoR:
-
Duration of response
- ECOG:
-
Eastern cooperative oncology group
- EGFR:
-
Epidermal growth factor receptor
- FAS:
-
Full analysis set
- HR:
-
Hazard ratio
- ICI:
-
Immune checkpoint inhibitor
- NSCLC:
-
Non-small cell lung cancer
- NR:
-
Not reached
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PD-1:
-
Programmed cell death protein 1
- PD-L1:
-
Programmed death-ligand 1
- PFS:
-
Progression-free survival
- PPE:
-
Palmar-plantar erythrodysesthesia syndrome
- PR:
-
Partial response
- Q3W:
-
Once every 3 weeks
- QD:
-
Once daily
- RCCEP:
-
Reactive cutaneous capillary endothelial proliferation
- RECIST:
-
Response evaluation criteria in solid tumors
- SD:
-
Stable disease
- tTMB:
-
Total tumor mutational burden
- TKI:
-
Tyrosine kinase inhibitor
- TME:
-
Tumor microenvironment
- TPS:
-
Tumor proportion score
- TRAE:
-
Treatment-related adverse event
- TTR:
-
Time to treatment response
References
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A et al (2022) Non-small cell lung cancer, version 3. 2022, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 20(5):497–530
Garon EB, Ciuleanu TE, Arrieta O, Prabhash K, Syrigos KN, Goksel T et al (2014) Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet 384(9944):665–673
Reck M, Kaiser R, Mellemgaard A, Douillard JY, Orlov S, Krzakowski M et al (2014) Docetaxel plus nintedanib versus docetaxel plus placebo in patients with previously treated non-small-cell lung cancer (LUME-Lung 1): a phase 3, double-blind, randomised controlled trial. Lancet Oncol 15(2):143–155
Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WE, Poddubskaya E et al (2015) Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 373(2):123–135
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE et al (2015) Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 373(17):1627–1639
Wu YL, Lu S, Cheng Y, Zhou C, Wang J, Mok T et al (2019) Nivolumab versus docetaxel in a predominantly Chinese patient population with previously treated advanced NSCLC: CheckMate 078 randomized phase III clinical trial. J Thorac Oncol 14(5):867–875
Herbst RS, Baas P, Kim DW, Felip E, Pérez-Gracia JL, Han JY et al (2016) Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 387(10027):1540–1550
Shigeta K, Datta M, Hato T, Kitahara S, Chen IX, Matsui A et al (2020) Dual programmed death receptor-1 and vascular endothelial growth factor receptor-2 blockade promotes vascular normalization and enhances antitumor immune responses in hepatocellular carcinoma. Hepatology 71(4):1247–1261
Shrimali RK, Yu Z, Theoret MR, Chinnasamy D, Restifo NP, Rosenberg SA (2010) Antiangiogenic agents can increase lymphocyte infiltration into tumor and enhance the effectiveness of adoptive immunotherapy of cancer. Cancer Res 70(15):6171–6180
Zhao S, Ren S, Jiang T, Zhu B, Li X, Zhao C et al (2019) Low-dose apatinib optimizes tumor microenvironment and potentiates antitumor effect of PD-1/PD-L1 blockade in lung cancer. Cancer Immunol Res 7(4):630–643
Reckamp KL, Redman MW, Dragnev KH, Minichiello K, Villaruz LC, Faller B et al (2022) Phase II randomized study of ramucirumab and pembrolizumab versus standard of care in advanced non-small-cell lung cancer previously treated with immunotherapy-lung-MAP S1800A. J Clin Oncol 40(21):2295–2306
Makker V, Taylor MH, Aghajanian C, Oaknin A, Mier J, Cohn AL et al (2020) Lenvatinib plus pembrolizumab in patients With advanced endometrial cancer. J Clin Oncol 38(26):2981–2992
Leighl NB, Hui R, Rodríguez-Abreu D, Nishio M, Hellmann MD, Lee C et al (2020) Abstract CT289: pembrolizumab plus lenvatinib vs. docetaxel in patients with previously treated metastatic non-small-cell lung cancer (NSCLC) and PD after platinum-doublet chemotherapy and immunotherapy: phase 3, randomized, open-label LEAP-008 trial. Can Res 80(16_Supplement):289
Zhou C, Chen G, Huang Y, Zhou J, Lin L, Feng J et al (2021) Camrelizumab plus carboplatin and pemetrexed versus chemotherapy alone in chemotherapy-naive patients with advanced non-squamous non-small-cell lung cancer (CameL): a randomised, open-label, multicentre, phase 3 trial. Lancet Respir Med 9(3):305–314
Ren S, Chen J, Xu X, Jiang T, Cheng Y, Chen G et al (2022) Camrelizumab plus carboplatin and paclitaxel as first-line treatment for advanced squamous NSCLC (CameL-Sq): a phase 3 trial. J Thorac Oncol 17(4):544–557
Lou L, Mi Y, Xu Y, Xie C, Zhao H (2011) Abstract 3604: preclinical antitumor study of famitinib, an orally available multi-targeted kinase inhibitor of VEGFR/PDGFR/c-Kit in phase I clinical trials. Can Res 71(8_Supplement):3604–3604
Xia L, Peng J, Lou G, Pan M, Zhou Q, Hu W et al (2022) Antitumor activity and safety of camrelizumab plus famitinib in patients with platinum-resistant recurrent ovarian cancer: results from an open-label, multicenter phase 2 basket study. J Immunother Cancer 10(1):e003831
Qu YY, Zhang HL, Guo H, Luo H, Zou Q, Xing N et al (2021) Camrelizumab plus famitinib in patients with advanced or metastatic renal cell carcinoma: data from an open-label, multicenter phase II basket study. Clin Cancer Res 27(21):5838–5846
Qu Y-Y, Sun Z, Han W, Zou Q, Xing N, Luo H et al (2022) Camrelizumab plus famitinib for advanced or metastatic urothelial carcinoma after platinum-based therapy: data from a multicohort phase 2 study. J Immunother Cancer 10(5):e004427
Hellmann MD, Ciuleanu TE, Pluzanski A, Lee JS, Otterson GA, Audigier-Valette C et al (2018) Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med 378(22):2093–2104
Ready N, Hellmann MD, Awad MM, Otterson GA, Gutierrez M, Gainor JF et al (2019) First-line nivolumab Plus ipilimumab in advanced non-small-cell lung cancer (CheckMate 568): outcomes by programmed death ligand 1 and tumor mutational burden as biomarkers. J Clin Oncol 37(12):992–1000
Koyama T, Chen H (2008) Proper inference from Simon’s two-stage designs. Stat Med 27(16):3145–3154
Mok TSK, Wu YL, Kudaba I, Kowalski DM, Cho BC, Turna HZ et al (2019) Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 393(10183):1819–1830
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A et al (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375(19):1823–1833
Makker V, Rasco D, Vogelzang NJ, Brose MS, Cohn AL, Mier J et al (2019) Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer: an interim analysis of a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol 20(5):711–718
Xu RH, Shen L, Wang KM, Wu G, Shi CM, Ding KF et al (2017) Famitinib versus placebo in the treatment of refractory metastatic colorectal cancer: a multicenter, randomized, double-blinded, placebo-controlled, phase II clinical trial. Chin J Cancer 36(1):97
Zhou A, Zhang W, Chang C, Chen X, Zhong D, Qin Q et al (2013) Phase I study of the safety, pharmacokinetics and antitumor activity of famitinib. Cancer Chemother Pharmacol 72(5):1043–1053
Zhang W, Zhou AP, Qin Q, Chang CX, Jiang HY, Ma JH et al (2013) Famitinib in metastatic renal cell carcinoma: a single center study. Chin Med J (Engl) 126(22):4277–4281
Grothey A, Van Cutsem E, Sobrero A, Siena S, Falcone A, Ychou M et al (2013) Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 381(9863):303–312
Li J, Qin S, Xu R, Yau TC, Ma B, Pan H et al (2015) Regorafenib plus best supportive care versus placebo plus best supportive care in Asian patients with previously treated metastatic colorectal cancer (CONCUR): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 16(6):619–629
Chen X, Ma L, Wang X, Mo H, Wu D, Lan B et al (2019) Reactive capillary hemangiomas: a novel dermatologic toxicity following anti-PD-1 treatment with SHR-1210. Cancer Biol Med 16(1):173–181
Zhou C, Wang Y, Zhao J, Chen G, Liu Z, Gu K et al (2021) Efficacy and biomarker analysis of camrelizumab in combination with apatinib in patients with advanced nonsquamous NSCLC previously treated with chemotherapy. Clin Cancer Res 27(5):1296–1304
Xu J, Zhang Y, Jia R, Yue C, Chang L, Liu R et al (2019) Anti-PD-1 Antibody SHR-1210 combined with apatinib for advanced hepatocellular carcinoma, gastric, or esophagogastric junction cancer: an open-label, dose escalation and expansion study. Clin Cancer Res 25(2):515–523
Peng Z, Wei J, Wang F, Ying J, Deng Y, Gu K et al (2021) Camrelizumab combined with chemotherapy followed by camrelizumab plus apatinib as first-line therapy for advanced gastric or gastroesophageal junction adenocarcinoma. Clin Cancer Res 27(11):3069–3078
Acknowledgements
We thank all patients and their families, investigators, and research personals for participating in this study. Writing assistance was provided by Lin Dong (PhD, a Medical Writer from Jiangsu Hengrui Pharmaceuticals Co., Ltd) according to Good Publication Practice Guidelines.
Funding
The study was funded by Jiangsu Hengrui Pharmaceuticals Co., Ltd.; the Outstanding Discipline Leader Program, sponsored by the Science and Technology Commission of Shanghai Municipality (No. 21XD1423200); and the National Key Clinical Program in Thoracic Oncology (2023).
Author information
Authors and Affiliations
Contributions
Conception and design of the study: JF and CZ. Collection and assembly of clinical data: SR, AX, JY, XW, BH, YP, JZ, YC, SH, TL, YL, YC, JF, SY, SG, SG, YL, YL, CL, HD and SW. Data analysis: XY. Interpretation of results: JF and CZ. Writing and revision and final approval of the manuscript: all authors.
Corresponding authors
Ethics declarations
Conflict of interest
HD, SW, and XY report being employed by Jiangsu Hengrui Pharmaceuticals Co., Ltd. All remaining authors have declared no conflict of interest.
Ethical approval
The study protocol was approved by institutional review boards or ethic committees at each center, and the study was conducted in accordance with the protocol, Good Clinical Practice guidelines and Declaration of Helsinki.
Informed consent
Patients were required to provide written informed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ren, S., Xiong, A., Yu, J. et al. Camrelizumab plus famitinib in previously chemo-immunotherapy treated patients with advanced NSCLC: results from an open-label multicenter phase 2 basket study. Cancer Immunol Immunother 73, 124 (2024). https://doi.org/10.1007/s00262-024-03715-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00262-024-03715-4