Abstract
Purpose
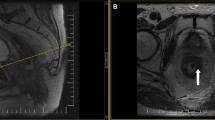
To compare the sensitivity, specificity and intra-observer and inter-observer agreement of pelvic magnetic resonance imaging (MRI) b800 and b1500 s/mm2 sequences in the detection of residual adenocarcinoma after neoadjuvant chemoradiation (CRT) for locally advanced rectal cancer (LARC).
Introduction
Detection of residual adenocarcinoma after neoadjuvant CRT for LARC has become increasingly important and relies on both MRI and endoscopic surveillance. Optimal MRI diffusion b values have yet to be established for this clinical purpose.
Methods
From our MRI database between 2018 and 2019, we identified a cohort of 28 patients after exclusions who underwent MRI of the rectum before and after neoadjuvant chemoradiation with a protocol that included both b800 and b1500 s/mm2 diffusion sequences. Four radiologists experienced in rectal MRI interpreted the post-CRT MRI studies with either b800 DWI or b1500 DWI, and a minimum of 2 weeks later re-interpreted the same studies using the other b value sequence. Surgical pathology or endoscopic follow-up for 1 year without tumor re-growth was used as the reference standard. Descriptive statistics compared accuracy for each reader and for all readers combined between b values. Inter-observer agreement was assessed using kappa statistics. A p value of 0.05 or less was considered significant.
Results
Within the cohort, 19/28 (67.9%) had residual tumor, while 9/28 (32.1%) had a complete response. Among four readers, one reader had increased sensitivity for detection of residual tumor at b1500 s/mm2 (0.737 vs. 0.526, p = 0.046). There was no significant difference between detection of residual tumor at b800 and at b1500 for the rest of the readers. With all readers combined, the pooled sensitivity was 0.724 at b1500 versus 0.605 at b800, but this was not significant (p = 0.119). There was no difference in agreement between readers at the two b value settings (67.8% at b800 vs. 72.0% at b1500), or for any combination of individual readers.
Conclusion
Aside from one reader demonstrating increased sensitivity, no significant difference in accuracy parameters or inter-observer agreement was found between MR using b800 and b1500 for the detection of residual tumor after neoadjuvant CRT for LARC. However, there was a suggestion of a trend towards increased sensitivity with b1500, and further studies using larger cohorts may be needed to further investigate this topic.

Similar content being viewed by others
References
Napoletano M, Mazzucca D, Prosperi E, Aisa MC, Lupattelli M, Aristei C, Scialpi M (2019) Locally advanced rectal cancer: qualitative and quantitative evaluation of diffusion-weighted magnetic resonance imaging in restaging after neoadjuvant chemo-radiotherapy. Abdom Radiol (NY). https://doi.org/10.1007/s00261-019-02012-4
Amodeo S, Rosman AS, Desiato V, Hindman NM, Newman E, Berman R, Pachter HL, Melis M (2018) MRI-Based Apparent Diffusion Coefficient for Predicting Pathologic Response of Rectal Cancer After Neoadjuvant Therapy: Systematic Review and Meta-Analysis. AJR Am J Roentgenol 211 (5):W205-W216. https://doi.org/10.2214/ajr.17.19135
De Felice F, Magnante AL, Musio D, Ciolina M, De Cecco CN, Rengo M, Laghi A, Tombolini V (2017) Diffusion-weighted magnetic resonance imaging in locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Eur J Surg Oncol 43 (7):1324-1329. https://doi.org/10.1016/j.ejso.2017.03.010
Blazic IM, Lilic GB, Gajic MM (2017) Quantitative Assessment of Rectal Cancer Response to Neoadjuvant Combined Chemotherapy and Radiation Therapy: Comparison of Three Methods of Positioning Region of Interest for ADC Measurements at Diffusion-weighted MR Imaging. Radiology 282 (2):418-428. https://doi.org/10.1148/radiol.2016151908
Foti PV, Privitera G, Piana S, Palmucci S, Spatola C, Bevilacqua R, Raffaele L, Salamone V, Caltabiano R, Magro G, Li Destri G, Milone P, Ettorre GC (2016) Locally advanced rectal cancer: Qualitative and quantitative evaluation of diffusion-weighted MR imaging in the response assessment after neoadjuvant chemo-radiotherapy. Eur J Radiol Open 3:145-152. https://doi.org/10.1016/j.ejro.2016.06.003
Cai PQ, Wu YP, An X, Qiu X, Kong LH, Liu GC, Xie CM, Pan ZZ, Wu PH, Ding PR (2014) Simple measurements on diffusion-weighted MR imaging for assessment of complete response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Eur Radiol 24 (11):2962-2970. https://doi.org/10.1007/s00330-014-3251-5
Lu W, Jing H, Ju-Mei Z, Shao-Lin N, Fang C, Xiao-Ping Y, Qiang L, Biao Z, Su-Yu Z, Ying H (2017) Intravoxel incoherent motion diffusion-weighted imaging for discriminating the pathological response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Sci Rep 7 (1):8496. https://doi.org/10.1038/s41598-017-09227-9
Yu J, Xu Q, Song JC, Li Y, Dai X, Huang DY, Zhang L, Li Y, Shi HB (2017) The value of diffusion kurtosis magnetic resonance imaging for assessing treatment response of neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Eur Radiol 27 (5):1848-1857. https://doi.org/10.1007/s00330-016-4529-6
Joye I, Deroose CM, Vandecaveye V, Haustermans K (2014) The role of diffusion-weighted MRI and (18)F-FDG PET/CT in the prediction of pathologic complete response after radiochemotherapy for rectal cancer: a systematic review. Radiother Oncol 113 (2):158-165. https://doi.org/10.1016/j.radonc.2014.11.026
Adubeiro N, Nogueira ML, Nunes RG, Ferreira HA, Ribeiro E, La Fuente JMF (2018) Apparent diffusion coefficient in the analysis of prostate cancer: determination of optimal b value pair to differentiate normal from malignant tissue. Clin Imaging 47:90-95. https://doi.org/10.1016/j.clinimag.2017.09.004
Agarwal HK, Mertan FV, Sankineni S, Bernardo M, Senegas J, Keupp J, Daar D, Merino M, Wood BJ, Pinto PA, Choyke PL, Turkbey B (2017) Optimal high b value for diffusion-weighted MRI in diagnosing high risk prostate cancers in the peripheral zone. J Magn Reson Imaging 45 (1):125-131. https://doi.org/10.1002/jmri.25353
Manenti G, Nezzo M, Chegai F, Vasili E, Bonanno E, Simonetti G (2014) DWI of Prostate Cancer: Optimal b Value in Clinical Practice. Prostate Cancer 2014:868269. https://doi.org/10.1155/2014/868269
Tamura T, Murakami S, Naito K, Yamada T, Fujimoto T, Kikkawa T (2014) Investigation of the optimal b value to detect breast tumors with diffusion-weighted imaging by 1.5-T MRI. Cancer Imaging 14:11. https://doi.org/10.1186/1470-7330-14-11
Karki K, Hugo GD, Ford JC, Olsen KM, Saraiya S, Groves R, Weiss E (2015) Estimation of optimal b value sets for obtaining apparent diffusion coefficient free from perfusion in non-small cell lung cancer. Phys Med Biol 60 (20):7877-7891. https://doi.org/10.1088/0031-9155/60/20/7877
Kaya B, Koc Z (2014) Diffusion-weighted MRI and optimal b value for characterization of liver lesions. Acta Radiol 55 (5):532-542. https://doi.org/10.1177/0284185113502017
Beets-Tan RGH, Lambregts DMJ, Maas M, Bipat S, Barbaro B, Curvo-Semedo L, Fenlon HM, Gollub MJ, Gourtsoyianni S, Halligan S, Hoeffel C, Kim SH, Laghi A, Maier A, Rafaelsen SR, Stoker J, Taylor SA, Torkzad MR, Blomqvist L (2018) Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol 28 (4):1465-1475. https://doi.org/10.1007/s00330-017-5026-2
Horvat N, Carlos Tavares Rocha C, Clemente Oliveira B, Petkovska I, Gollub MJ (2019) MRI of Rectal Cancer: Tumor Staging, Imaging Techniques, and Management. Radiographics 39 (2):367-387. https://doi.org/10.1148/rg.2019180114
Wei IH, Garcia-Aguilar J (2018) Non-operative management of rectal cancer: understanding tumor biology. Minerva Chir 73 (6):601-618. https://doi.org/10.23736/s0026-4733.18.07743-x
Smith JJ, Chow OS, Gollub MJ, Nash GM, Temple LK, Weiser MR, Guillem JG, Paty PB, Avila K, Garcia-Aguilar J, Rectal Cancer C (2015) Organ Preservation in Rectal Adenocarcinoma: a phase II randomized controlled trial evaluating 3-year disease-free survival in patients with locally advanced rectal cancer treated with chemoradiation plus induction or consolidation chemotherapy, and total mesorectal excision or nonoperative management. BMC Cancer 15:767. https://doi.org/10.1186/s12885-015-1632-z
Maas M, Lambregts DM, Nelemans PJ, Heijnen LA, Martens MH, Leijtens JW, Sosef M, Hulsewe KW, Hoff C, Breukink SO, Stassen L, Beets-Tan RG, Beets GL (2015) Assessment of Clinical Complete Response After Chemoradiation for Rectal Cancer with Digital Rectal Examination, Endoscopy, and MRI: Selection for Organ-Saving Treatment. Ann Surg Oncol 22 (12):3873-3880. https://doi.org/10.1245/s10434-015-4687-9
Koo JH, Kim CK, Choi D, Park BK, Kwon GY, Kim B (2013) Diffusion-weighted magnetic resonance imaging for the evaluation of prostate cancer: optimal B value at 3T. Korean J Radiol 14 (1):61-69. https://doi.org/10.3348/kjr.2013.14.1.61
Cercek A, Goodman KA, Hajj C, Weisberger E, Segal NH, Reidy-Lagunes DL, Stadler ZK, Wu AJ, Weiser MR, Paty PB, Guillem JG, Nash GM, Temple LK, Garcia-Aguilar J, Saltz LB (2014) Neoadjuvant chemotherapy first, followed by chemoradiation and then surgery, in the management of locally advanced rectal cancer. J Natl Compr Canc Netw 12 (4):513-519
Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U, Jr., Silva e Sousa AH, Jr., Campos FG, Kiss DR, Gama-Rodrigues J (2004) Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg 240 (4):711-717; discussion 717-718. https://doi.org/10.1097/01.sla.0000141194.27992.32
Parikh R, Mathai A, Parikh S, Chandra Sekhar G, Thomas R (2008) Understanding and using sensitivity, specificity and predictive values. Indian J Ophthalmol 56 (1):45-50. https://doi.org/10.4103/0301-4738.37595
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bates, D.D.B., Golia Pernicka, J.S., Fuqua, J.L. et al. Diagnostic accuracy of b800 and b1500 DWI-MRI of the pelvis to detect residual rectal adenocarcinoma: a multi-reader study. Abdom Radiol 45, 293–300 (2020). https://doi.org/10.1007/s00261-019-02283-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02283-x