Abstract
Purpose
Accurate estimation of esophageal hiatus surface area (HSA) prior to surgical repair of hiatal hernia is difficult. The ability to do so may assist with following progression of hiatal hernias, choosing the optimal surgical approach and post-surgical evaluation. We developed a method for measurement of HSA using multi-planar reconstruction (MPR) of multi-detector computed tomography (MDCT) scans and sought to validate our method using intra-operative HSA measurements.
Methods
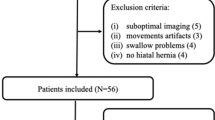
Patients with thoracic or abdominal CT scans who were scheduled to undergo hiatal hernia repair were identified. A radiologist performed MPR of each MDCT scan to obtain the measured HSA (mHSA). Estimated HSA (eHSA) was obtained using intra-operative measurements of crura length and distance between crural edges. The association between eHSA and the corresponding mHSA was assessed using Pearson correlation. The intra-class correlation coefficient was calculated to assess both intra-observer and inter-observer agreement for the MDCT–MPR technique.
Results
Of 30 subjects included, 16 (53.3%) were female and the median age was 68.5 years. All patients underwent robotic-assisted laparoscopic hiatal hernia repair. The median HSA was 8.1 cm2 based on intra-operative measurements and 9.9 cm2 based on CT measurements. The correlation coefficient for eHSA and corresponding mHSA was 0.83 (p < 0.001). The intra-class correlation coefficient was 0.97 (p < 0.001) for intra-observer agreement and 0.97 (p < 0.001) for inter-observer agreement.
Conclusion
We developed a MDCT–MPR technique that measures HSA in vivo. This technique is reproducible and can be used for pre-operative planning and post-operative follow-up of patients with symptomatic hiatal hernia.






Similar content being viewed by others
References
Gryglewski A, Pena IZ, Tomaszewski KA, Walocha JA (2014) Unsolved questions regarding the role of esophageal hiatus anatomy in the development of esophageal hiatal hernias. Adv Clin Exp Med 23(4):639-644.
Shamiyeh A, Szabo K, Granderath FA, Syre G, Wayand W, Zehetner J (2010) The esophageal hiatus: What is the normal size? Surg Endosc 4(5):988-991
Ouyang W, Dass C, Zhao H, Kim C, Criner G (2016) COPDGene Investigators. Multiplanar MDCT measurement of esophageal hiatus surface area: Association with hiatal hernia and GERD. Surg Endosc 30(6):2465-2472.
Granderath FA, Schweiger UM, Pointner R (2007) Laparoscopic antireflux surgery: Tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 21(4):542-548.
Grubnik VV, Malynovskyy AV (2013) Laparoscopic repair of hiatal hernias: New classification supported by long-term results. Surg Endosc 27(11):4337-4346.
Kao AM, Ross SW, Otero J, et al. (2019) Use of computed tomography volumetric measurements to predict operative techniques in paraesophageal hernia repair. Surg Endosc. https://doi.org/10.1007/s00464-019-06930-8.
Koch OO, Asche KU, Berger J, Weber E, Granderath FA, Pointner R (2011) Influence of the size of the hiatus on the rate of reherniation after laparoscopic fundoplication and refundopilication with mesh hiatoplasty. Surg Endosc 25(4):1024-1030.
Koch OO, Kaindlstorfer A, Antoniou SA, Asche KU, Granderath FA, Pointner R (2012) Influence of the esophageal hiatus size on the lower esophageal sphincter, on reflux activity and on symptomatology. Dis Esophagus 25(3):201-208.
Batirel HF, Uygur-Bayramicli O, Giral A, et al. (2010) The size of the esophageal hiatus in gastroesophageal reflux pathophysiology: Outcome of intraoperative measurements. J Gastrointest Surg 14(1):38-44.
Franzen T, Tibbling L (2014) Is the severity of gastroesophageal reflux dependent on hiatus hernia size? World J Gastroenterol 20(6):1582-1584.
Kohn GP, Price RR, DeMeester SR, et al. (2013) Guidelines for the management of hiatal hernia. Surg Endosc 27(12):4409-4428.
Kahrilas PJ, Kim HC, Pandolfino JE (2008) Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol 22(4):601-616.
Kavic SM, Segan RD, George IM, Turner PL, Roth JS, Park A (2006) Classification of hiatal hernias using dynamic three-dimensional reconstruction. Surg Innov 13(1):49-52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Temple University Institutional Review Board; protocol # 24196) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Moten, A.S., Ouyang, W., Hava, S. et al. In vivo measurement of esophageal hiatus surface area using MDCT: description of the methodology and clinical validation. Abdom Radiol 45, 2656–2662 (2020). https://doi.org/10.1007/s00261-019-02279-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02279-7