Abstract
Purpose
Accurate preoperative localization is imperative to guide surgery in primary hyperparathyroidism (pHPT). It remains unclear which second-line imaging technique is most effective after negative first-line imaging. In this study, we compare the diagnostic effectiveness of [11C]methionine PET/CT, [11C]choline PET/CT, and four dimensional (4D)-CT head-to-head in patients with pHPT, to explore which of these imaging techniques to use as a second-line scan.
Methods
We conducted a powered, prospective, blinded cohort study in patients with biochemically proven pHPT and prior negative or discordant first-line imaging consisting of ultrasonography and 99mTc-sestamibi. All patients underwent [11C]methionine PET/CT, [11C]choline PET/CT, and 4D-CT. At first, all scans were interpreted by a nuclear medicine physician, and a radiologist who were blinded from patient data and all imaging results. Next, a non-blinded scan reading was performed. The scan results were correlated with surgical and histopathological findings. Serum calcium values at least 6 months after surgery were used as gold standard for curation of HPT.
Results
A total of 32 patients were included in the study. With blinded evaluation, [11C]choline PET/CT was positive in 28 patients (88%), [11C]methionine PET/CT in 23 (72%), and 4D-CT in 15 patients (47%), respectively. In total, 30 patients have undergone surgery and 32 parathyroid lesions were histologically confirmed as parathyroid adenomas. Based on the blinded evaluation, lesion-based sensitivity of [11C]choline PET/CT, [11C]methionine PET/CT, and 4D-CT was respectively 85%, 67%, and 39%. The sensitivity of [11C]choline PET/CT differed significantly from that of [11C]methionine PET/CT and 4D-CT (p = 0.031 and p < 0.0005, respectively).
Conclusion
In the setting of pHPT with negative first-line imaging, [11C]choline PET/CT is superior to [11C]methionine PET/CT and 4D-CT in localizing parathyroid adenomas, allowing correct localization in 85% of adenomas. Further studies are needed to determine cost–benefit and efficacy of these scans, including the timing of these scans as first- or second-line imaging techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (pHPT) is a common endocrine disorder, with the highest incidence in post-menopausal women [1]. The incidence of pHPT is estimated to be 65.5 per 100,000 person-years among women and 24.7 per 100,000 person-years among men [1].
Surgery is the only curative treatment for patients with pHPT, and is associated with a decreased risk of fractures and nephrolithiasis, and long-term improvement in quality of life [2,3,4]. As in 90% of patients, only one parathyroid adenoma is present, a minimally invasive parathyroidectomy (MIP) is the preferred surgical approach [5]. In comparison to a bilateral neck exploration, a MIP is associated with less postoperative morbidity with similar cure rates [6, 7]. In order to perform a MIP, accurate preoperative imaging is essential. Worldwide, the currently advised first-line preoperative imaging approach consists of cervical ultrasonography (cUS) combined with 99mTc-methoxyisobutylisonitrile-single-photon emission computed tomography/computed tomography ([99mTc]Tc-MIBI-SPECT/CT) [8,9,10]. This combination of scans has proven to be the most cost-effective strategy and is widely available [9]. However, both modalities have limited sensitivity [10,11,12,13]. Unsuccessful preoperative localization of the adenoma would subsequently mandate traditional bilateral neck exploration, exposing both recurrent laryngeal nerves, risking postoperative hypoparathyroidism and increased scarring in the neck.
Recently, there has been increased interest in the use of positron emission tomography/computed tomography (PET/CT) for parathyroid imaging. Both [11C]methionine PET/CT and [18F/11C]choline PET/CT can be used as second-line scans after prior negative first-line localization [14,15,16]. Furthermore, four-dimensional CT (4D-CT) can be used for the localization of parathyroid adenomas [17]. 4D-CT consists of serial CT scans acquired at different stages of enhancement and washout of contrast media in the parathyroid glands, and its neighboring organs and tissues [18]. The sensitivity of [11C]methionine PET/CT is reported between 60 and 86% [19,20,21], of [18F/11C]choline PET/CT between 87 and 96% [15, 21,22,23,24,25] and of 4D-CT between 80 and 90% [13, 26, 27]. However, no studies are available comparing these three techniques directly. Therefore, it remains unclear which of these imaging techniques is most effective after negative first-line imaging. Consequently, in routine daily care, the preoperative imaging workup is managed in a heterogeneous manner [28].
There is a clear clinical need for more accurate localization of parathyroid adenomas preoperatively when first-line imaging fails. This will enable more targeted, less extensive, and more effective surgical strategies. Therefore, the main aim of this study was to directly compare the sensitivity of [11C]methionine PET/CT with [11C]choline PET/CT. Furthermore, the study aimed to assess the sensitivity of 4D-CT, and which of these three imaging techniques to use as a second-line scan in the setting of pHPT.
Methods
Study design and patients
This is a single-center prospective, blinded interventional study primarily designed to compare the sensitivity of [11C]methionine PET/CT with [11C]choline PET/CT and secondarily 4D-CT in patients with biochemically proven pHPT and prior negative, inconclusive or discordant first-line imaging consisting of cUS and [99mTc]Tc-MIBI−SPECT/CT in a tertiary teaching referral hospital in the Netherlands between March 2019 and August 2022.
Patients eligible for inclusion were (i) ≥ 18 years old, (ii) had biochemically confirmed pHPT (defined as elevated serum calcium adjusted for albumin in the presence of an elevated or inappropriately normal PTH, or normal adjusted total calcium and normal ionized calcium levels along with elevated PTH on at least two occasions [29]), (iii) underwent a [99mTc]Tc-MIBI-SPECT/CT and cUS with negative or discordant results, (iv) had an indication for parathyroidectomy, and (v) were eligible for surgery. Patients were excluded (i) if they were known to have a germline mutation predisposing for multiple gland disease, (ii) if an alternative diagnosis (e.g., parathyroid carcinoma) was suspected before surgery, if they had (iii) a previous negative neck exploration for pHPT, (iv) persistent pHPT after previous negative neck exploration, if they had (v) an eGFR < 30 ml/min × 1.73 m2, (vi) or an allergy for iodinated contrast, or (vii) if they were pregnant.
First-line imaging results were categorized as negative when they failed to visualize any parathyroid adenoma, or when read as inconclusive, not convincingly showing an adenoma. First-line imaging results were classified as discordant if a potential adenoma was identified on only one imaging modality (e.g., negative [99mTc]Tc-MIBI-SPECT/CT and positive cUS) or if both imaging modalities showed an adenoma but in different locations. Subsequently, all patients in this study underwent [11C]methionine PET/CT, [11C]choline PET/CT, and 4D-CT. The main outcome was the sensitivity of [11C]methionine PET/CT and [11C]choline PET/CT. Secondary outcomes were the sensitivity of 4D-CT and the positive predictive value (PPV) of [11C]methionine PET/CT, [11C]choline PET/CT and 4D-CT.
The study was registered at the Netherlands Trial Register (NTR7423) and approved by the Research Ethics Board of the University Medical Center Groningen, The Netherlands (METc 2018/330). This study was performed in line with the principles of the Declaration of Helsinki. Written informed consent was obtained from all subjects.
Scan interpretation
For the methods of all imaging techniques, refer to the Supplemental Material in Online Resource 1. All patients underwent all three imaging techniques ([11C]methionine PET/CT, [11C]choline PET/CT, and 4D-CT).
All scans ([11C]methionine PET/CT, [11C]choline PET/CT, and 4D-CT) were blinded from patient data and previous imaging modalities, and subsequently separately evaluated by one dedicated nuclear medicine physician (A. H. B.) for the PET/CT scans and one of two dedicated radiologists (A. P. A. A. or A. H.) for the 4D-CT. During the blind evaluation, no clinical or other imaging results were available to the readers. Hereafter, the radiologist and nuclear medicine physician came to a non-blinded consensus regarding the localization of the parathyroid adenoma. In this setting, the readers could make use of all available clinical and imaging data, including the original imaging reports of all scans. Scan outcomes were classified as negative (not, or not convincingly showing an adenoma), or as positive (suspected adenoma with its respective location). The location of the suspected adenoma was described in relation to the position of the thyroid midline/trachea. This resulted in the following possible locations: right cranial, right caudal, left cranial, left caudal, or ectopic (e.g., mandibular angle; paratracheal, paratracheal-esophageal, or mediastinal).
Surgery
A MIP was performed via a lateral keyhole incision of 2.5 cm medial of the sternocleidomastoid muscle and lateral of the anterior strap muscles. When needed, a bilateral neck exploration was performed via a Kocher incision (usually 3 cm) over the thyroid parallel to the skin folds. The aim of surgery was to identify and remove the parathyroid adenoma, if possible concordant with preoperative imaging (based on the non-blinded consensus reading). Final localization of the adenoma during surgery was retrieved from the anatomic description in the surgical report. The pathology report was reviewed for the final diagnosis. Cure was defined as normal serum albumin-corrected calcium level (< 2.55 mmol/L) 6 months after surgery [30].
Preoperative adenoma localization of both the blinded and non-blinded scan evaluations were defined as true positive, false positive, and false negative, depending on both the surgical and pathology report and serum calcium levels at 6 months post-surgery. We do not report on true negative results since the surgeon did not systematically explore all potential embryological locations to exclude a parathyroid adenoma. A true positive lesion was defined as pathological proven adenoma localized to the correct quadrant on pre-operative imaging. A false positive lesion was defined as a suspected adenoma localized to the incorrect quadrant, or a suspected lesion in a quadrant while surgically no pathological parathyroid gland was found in this quadrant. Lastly, a false negative lesion was classified as removal of a pathological proven parathyroid adenoma during surgery, although the scan had not demonstrated the presence of hyperactive parathyroid tissue in this quadrant.
Statistical analysis
A power analysis, before we executed this prospective study, using the method of Connor et al. was performed on the main outcome (sensitivity of [11C]methionine PET/CT of 72%[19] and of [11C]choline PET/CT of 97%[25]), and with these sensitivities as our aim, sample size calculation with a two-sided significance level of 0.05 and power of 80%, revealed a needed requirement (higher bound) of 29 patients [31].
Data were analyzed using descriptive statistics. Continuous variables with normal distribution or abnormal distribution are displayed by mean ± standard deviation (SD) or median with interquartile range (IQR), respectively. Sensitivity and PPV were calculated lesion-based. To compare the sensitivity across the different imaging techniques, the McNemar’s test was performed [32]. A two-sided p-value < 0.05 was considered statistically significant. Statistical analyses were performed using IBM SPSS Statistics version 27.0 (IBM Corp., Armonk, NY, USA).
Results
Study group
A total of 32 patients were included, of whom two were replaced according to protocol because these patients did eventually not want to undergo parathyroid surgery. These patients were included in the scan interpretation analyses (n = 32 patients), but could not be evaluated in the surgical lesion-based analysis (n = 30 patients). In total, twenty-four patients were female (75%) and the median age was 64.0 (IQR 16.5) years (Table 1). Median preoperative corrected calcium levels were 2.70 (IQR 0.17) mmol/L and PTH levels 10.3 (IQR 5.8) pmol/L. All included patients (100%) were hypercalcemic, and no patient was normocalcemic.
Scan interpretation
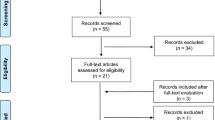
For results of the first-line imaging techniques, refer to the Supplemental Material in Online Resource 1. For results of the non-blinded scan interpretation, refer to the Supplemental Material in Online Resource 1. Figure 1 shows the images of a representative patient. When the scans were blinded from patient data and previous imaging modalities, [11C]methionine PET/CT was positive in 23 patients (72%) and identified 23 lesions suspicious for a parathyroid adenoma (Fig. 2). For [11C]choline PET/CT, this was the case in 28 patients (88%) identifying 32 lesions, whereas 4D-CT was positive in 15 patients (47%) identifying 16 lesions. For the overlap between the three imaging techniques, refer to Fig. 3.
Preoperative parathyroid imaging of a representative patient. Planar anterior image of the neck with [99mTc]Tc-MIBI (a early, b late) does not localize the parathyroid adenoma. The [11C]methionine PET/CT (c ldCT image, d fused PET/CT image, and e PET only image) also does not clearly locate a parathyroid adenoma (negative at both the blinded and non-blinded interpretation). On the [11C]choline PET/CT (f ldCT image, g fused PET/CT image, and h PET only image), a lesion suspicious for a parathyroid adenoma was shown caudally to the left thyroid lobe (red arrow in h). During parathyroidectomy, a parathyroid adenoma (0.9 cm and 0.18 g at pathology) was removed from this exact location. The 4D-CT scan (i nonenhanced phase, j arterial phase, k venous phase) did not evidently show the classic characteristic contrast enhancement pattern of parathyroid adenoma and was therefore declared as negative based on the blinded and non-blinded interpretation
Interestingly, 14 patients (44%) underwent a [18F]choline PET/CT prior to inclusion in our study. The [18F]choline PET/CT was negative in 12 patients and inconclusive in two patients, whereas at the blinded scan interpretation, [11C]methionine PET/CT, [11C]choline PET/CT, and 4D-CT could identify a lesion suspicious for a parathyroid adenoma in 10 (71%), 12 (86%), and 7 (58%) of these patients. Figures 6 and 7 in Online Resource 1 display examples of such cases with a previous negative [18F]choline PET/CT.
Surgery
Thirty patients (94%) underwent a surgical procedure and were included for the final analysis of the diagnostic effectiveness. Twenty-five patients (83%) underwent a focused parathyroidectomy, and five patients (17%) a bilateral exploration. In total, 32 parathyroid lesions were histologically confirmed as parathyroid adenomas. Median weight and diameter of parathyroid adenomas were 0.35 g (IQR 0.46 g) and 13.0 mm in largest diameter (IQR 6 mm). Three patients had multi-gland disease (n = 6 lesions) presumably not associated with multiple endocrine neoplasia syndrome. In 26 patients, one parathyroid adenoma was removed, and in one patient, no parathyroid tissue was removed during surgery.
In 29 patients (97%), 6-month follow-up calcium levels were available and biochemical cure was confirmed in 27/29 patients (93%). One patient had follow-up shorter than 6 months because he died due to a cardiac arrest; however, he was cured on day one postoperatively. In the two patients in whom biochemical cure was not achieved 6 months after surgery, in one patient, no parathyroid tissue was removed during surgery. The [11C]methionine PET/CT, [11C]choline PET/CT, and 4D-CT suggested a lesion caudal to the left submandibular gland (level IB). During surgery, exploration of the area of the submandibular gland was performed, but the presence of parathyroid tissue could not be confirmed by the pathologist. This patient was diagnosed with persistent hyperparathyroidism. In the lesion-based analysis, it was classified as both a false positive and a false negative lesion. The other non-cured patient was a patient with multiple gland disease. During surgery, two parathyroid glands were removed and were both confirmed as parathyroid hyperplasia. This patient was normocalcemic on postoperative day one; however, unfortunately, 6 months after surgery, the patient became hypercalcemic again. All scans in this patient were false negative. In the lesion-based analysis, they were classified as two false negative lesions. For additional results of the surgical procedure, refer to the Supplemental Material in Online Resource 1.
Accuracy of study imaging modalities
For results of the non-blinded scan interpretation, refer to the Supplemental Material in Online Resource 1. In the patients with multi-gland disease (n = 3 patients and n = 6 lesions), [11C]methionine PET/CT and 4D-CT were true positive in one lesion (17%), while [11C]choline PET/CT was true positive in four lesions (75%) at the blinded scan interpretation.
After blinded scan interpretation, [11C]methionine PET/CT resulted in a lesion-based sensitivity and PPV of 67% (95% CI: 48% to 82%) and 96% (95% CI: 76% to 100%), [11C]choline PET/CT in a sensitivity of 85% (95% CI: 68% to 95%) and PPV of 90% (95% CI: 73% to 98%), and 4D-CT in 39% (95% CI: 23% to 58%) and 87% (95% CI: 58% to 98%), respectively (Fig. 4). The sensitivity of [11C]methionine PET/CT was higher when the scans were blindly interpreted, whereas for 4D-CT, it was evidently lower and for [11C]choline PET/CT, it was similar (Table 2 and Table 1 in Online Resource 1). For the overlap between scan interpretation and histological results, refer to Fig. 4 in the Supplemental Material in Online Resource 1.
Effectiveness of the three studied imaging modalities for parathyroid adenoma localization with blinded scan interpretation (lesion-based). Adenoma localization on preoperative imaging was correlated with intraoperative surgeon localization and histopathological findings (reference standard). The total number of reference standard lesions (true positive + false negative) consists of n = 32 pathology-proven parathyroid lesions and one patient with a negative exploration (n = 1 lesion) in n = 30 operated patients
The sensitivity of [11C]choline PET/CT differed significantly from [11C]methionine PET/CT and 4D-CT for the blinded interpretations (p = 0.031 and p < 0.0005, respectively). The sensitivity of [11C]methionine PET/CT and also 4D-CT differed significantly for the blinded interpretations (p = 0.012).
Discussion
This study prospectively compared the diagnostic accuracy of [11C]methionine PET/CT, [11C]choline PET/CT, and 4D-CT head-to-head in patients with pHPT. Our results show that [11C]choline PET/CT is superior to [11C]methionine PET/CT and 4D-CT in localizing parathyroid adenomas.
Interestingly, the sensitivity for [11C]methionine PET/CT imaging decreased when the scans were interpreted non-blindly, as compared to the blinded interpretation. Contrarywise, the sensitivity and PPV for 4D-CT imaging evidently increased during the non-blinded scan interpretation. This finding may be the result of intra-observer variability and can be used as an additional argument to primarily employ ([11C]choline) PET/CT over 4D-CT imaging, since PET imaging initially resulted in more accurate findings, whereas for 4D-CT, more information from other imaging modalities was required. The blinded scan interpretation more closely resembles current practice, as these three imaging modalities will likely not all be performed in a patient with pHPT. Even though in the blinded scan interpretation [11C]methionine was superior to 4D-CT, one may consider performing 4D-CT after a negative [11C]choline PET/CT to obtain more information from an anatomical perspective (in addition to the ultrasound).
Several studies found that [11C]methionine PET/CT, [11C/18F]choline PET/CT, and 4D-CT are able to localize parathyroid lesions when conventional imaging failed to do so [13, 19,20,21, 23,24,25, 27, 33, 34]. A recent study prospectively comparing [11C]methionine PET/CT and [18F]choline PET/CT in 26 patients that underwent parathyroid surgery found that in patients with negative or inconclusive [99mTc]Tc-MIBI, [18F]choline PET/CT had a significant better performance than [11C]methionine PET/CT for the detection of pathological parathyroid tissue [21]. A recent meta-analysis showed that [18F]choline PET/CT had a higher sensitivity than 4D-CT, although only one of the included studies performed a head-to-head comparison [35]. This meta-analysis therefore also concluded that more comparative studies on the diagnostic performance of these imaging methods are needed. To the best of our knowledge, this is the first study comparing the three imaging techniques prospectively in the same patient for the preoperative detection and localization of hyperfunctioning parathyroid tissue.
The uptake of [11C]methionine most likely depends on expression and activity of amino-acid transporters such as LAT1, and secondarily on its incorporation in the protein pre-pro-PTH [21]. [11C]methionine is therefore closely related to the synthesis and excretion of PTH. Choline-labeled radiopharmaceuticals, thanks to their positive electric charge, enter through a membrane transporter and accumulate in the mitochondria of both oxyphilic and chief cells. Furthermore, in the chief cells, choline is also phosphorylated by choline-kinase, which is overexpressed in patients with HPT, and used as a component of cell membranes [21]. This double uptake of choline-labeled radiopharmaceuticals mechanism could represent the advantage of choline PET/CT to methionine PET/CT [36, 37].
The choice for [11C]choline rather than for 4D-CT, next to its superior diagnostic effectiveness, may also be supported by the consideration that 4D-CT generally involves a higher radiation exposure than [11C]choline PET/CT [24, 38,39,40,41,42]. Additionally, there is slight chance of an allergic reaction to the iodinated contrast of the 4D-CT scan. However, the main advantage of 4D-CT lies in its wide availability in most clinical environments, its detailed anatomical information, the absence of the need for tracer production, and due to more accessible patient preparation, no uptake time (and related waiting time) of tracer is necessary. The performance of 4D-CT in this study is relatively poor compared to previous studies (sensitivity of 75 to 80%) [43,44,45]. We hypothesize that this is due to the highly selected group of patients with previous negative imaging results.
Interestingly, in 12 out of 14 patients in whom [18F]choline PET/CT was negative or inconclusive before enrollment in the study, [11C]choline PET/CT could identify a lesion suspicious of a hyperfunctioning parathyroid gland. Therefore, in this study, [11C]choline PET/CT seemed to be superior to [18F]choline PET/CT for localization of parathyroid lesions. The cause of this finding unfortunately remains speculative. [18F]Choline, a tracer comparable to [11C]choline, is a more widely available tracer because of its longer half-life (110 min). We hypothesize that the improved identification with [11C]choline is mainly caused by differences in scan protocols between centers. For [11C]choline, we always employ an uptake time of 20 min and a scan duration of 10 min, after optimization of the protocol [46]. Most centers that use [18F]choline scan after 2, 30, and 60 min with a maximum scan duration of 5 min [25, 47,48,49,50,51]. Also, differences in biodistribution of the tracers cannot be ruled out. Since a direct comparison between the two choline tracers will likely not be performed in patients, only ex vivo experiments using both choline tracers may shed more light on this issue.
Based on the current results, [11C]choline PET/CT is the preferred choice for second-line imaging in our clinical setting. We are aware that in other clinics this tracer has drawbacks. These drawbacks consist of the need for an on-site cyclotron for the production of the short-lived isotope [11C] (20 min half-life), and a GMP radiopharmacy facility for the production of [11C]choline. Although [11C]choline PET/CT has shown superior results, data from large cohorts and on cost-efficacy are not currently available. Therefore, more research is warranted into the cost–benefit and efficacy of the three studied imaging techniques, also in the setting as first-line imaging techniques.
In this study, we chose to exclude patients with a germline mutation predisposing for multiple gland disease to maintain homogeneity within the study group. Therefore, we cannot elaborate on the diagnostic performance of these imaging modalities in this subgroup of patients. We did previously study the diagnostic performance of [11C]choline PET/CT in a small group of patients with multiple endocrine neoplasia and found a sensitivity of 67% [25]. However, more research is still warranted into additional preoperative imaging in these patients.
A limitation of this study could be that the preoperative work-up (including cUS and [99mTc]Tc-MIBI-SPECT/CT) prior to inclusion in the study was partly performed heterogeneously at outside institutions and reviewed by different nuclear medicine physicians, reflecting the real world setting. However, after inclusion, the work-up was homogenously performed as all imaging techniques were performed in the same hospital according to standardized protocols and reviewed by experts in the field. Also, the external [99mTc]Tc-MIBI-SPECT/CT were reviewed prior to inclusion into the study by an expert in the field. The major strength of this study is its prospective head-to-head design with an appropriate power calculation, and the performance of blinded and non-blinded evaluations of the scans by one dedicated nuclear medicine physician and two dedicated radiologists. Patients (n = 21) from several hospitals (n = 6) were referred for this study when initial imaging (cUS, [99mTc]Tc-MIBI-SPECT/CT, and/or [18F]choline PET/CT) failed to localize the parathyroid adenoma. Even in this highly selected group of patients with previous negative imaging, [11C]choline PET/CT achieved a high sensitivity of 85%. Moreover, [11C]choline PET/CT was able to better localize multi-gland lesions compared with [11C]methionine and 4D-CT although in a small patient number.
Conclusion
This study prospectively compared the diagnostic effectiveness of [11C]methionine PET/CT, [11C]choline PET/CT, and 4D-CT head-to-head in patients with pHPT after failure of first-line imaging. Our results show that [11C]choline PET/CT is superior to [11C]methionine PET/CT and 4D-CT in localizing parathyroid adenomas, allowing correct localization in 85% of parathyroid adenomas. Further studies are needed to determine cost–benefit and efficacy of the three studied imaging techniques for the localization of parathyroid adenomas, and to study their feasibility as potential first-line imaging techniques.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. Dr A. H. B and S. K. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
Yeh M, Ituarte P, Zhou H, Nishimoto S, Liu I, Harari A, Haigh P, Adams A. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. Clin Endocrinol Metab. 2013;98:1122–9.
Yeh MW, Zhou H, Adams AL, Ituarte PH, Li N, Liu IL, Haigh PI. The relationship of parathyroidectomy and bisphosphonates with fracture risk in primary hyperparathyroidism: an observational study. Ann Intern Med. 2016;164:715–23.
Mollerup CL, Vestergaard P, Frøkjaer VG, Mosekilde L, Christiansen P, Blichert-Toft M. Risk of renal stone events in primary hyperparathyroidism before and after parathyroid surgery: controlled retrospective follow up study. BMJ. 2002;325:807.
Pasieka JL, Parsons L, Jones J. The long-term benefit of parathyroidectomy in primary hyperparathyroidism: a 10-year prospective surgical outcome study. Surgery. 2009;146:1006–13.
Ruda J, Hollenbeak C, Stack B. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg. 2005;132:359–72.
Singh Ospina NM, Rodriguez-Gutierrez R, Maraka S, Espinosa de Ycaza AE, Jasim S, Castaneda-Guarderas A, Gionfriddo MR, Al Nofal A, Brito JP, Erwin P, Richards M, Wermers R, Montori VM. Outcomes of parathyroidectomy in patients with primary hyperparathyroidism: a systematic review and meta-analysis. World J Surg. 2016;40:2359–77.
Jinih M, O’Connell E, O’Leary DP, Liew A, Redmond HP. Focused versus bilateral parathyroid exploration for primary hyperparathyroidism: a systematic review and meta-analysis. Ann Surg Oncol. 2017;24:1924–34.
Bergenfelz AO, Hellman P, Harrison B, Sitges-Serra A, Dralle H, European Society of Endocrine Surgeons. Positional statement of the European Society of Endocrine Surgeons (ESES) on modern techniques in pHPT surgery. Langenbecks Arch Surg. 2009;394:761–4.
Wilhelm S, Wang T, Ruan D, Lee J, Asa S, Duh Q, Doherty G, Herrera M, Pasieka J, Perrier N, Silverberg S, Solórzano C, Sturgeon C, Tublin M, Udelsman R, Carty S. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg. 2016;151:959–68.
Petranović Ovčariček P, Giovanella L, Carrió Gasset I, Hindié E, Huellner MW, Luster M, Piccardo A, Weber T, Talbot JN, Verburg FA. The EANM practice guidelines for parathyroid imaging. Eur J Nucl Med Mol Imaging. 2021. https://doi.org/10.1007/s00259-021-05334-y.
Patel C, Salahudeen H, Lansdown M, Scarsbrook A. Clinical utility of ultrasound and 99mTc sestamibi SPECT/CT for preoperative localization of parathyroid adenoma in patients with primary hyperparathyroidism. Clin Radiol. 2010;65:278–87.
Akbaba G, Berker D, Isik S, Aydin Y, Ciliz D, Peksoy I, Ozuguz U, Tutuncu Y, Guler S. A comparative study of pre-operative imaging methods in patients with primary hyperparathyroidism: ultrasonography, 99mTc sestamibi, single photon emission computed tomography, and magnetic resonance imaging. J Endocrinol Investig. 2012;35:359–64.
Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19:577–83.
Caldarella C, Treglia G, Isgrò M, Giordano A. Diagnostic performance of positron emission tomography using 11C-methionine in patients with suspected parathyroid adenoma: a meta-analysis. Endocrine. 2013;43:78–83.
Kim S, Lee S, Jeong S, Pak K, Kim K. Diagnostic performance of F-18 fluorocholine PET/CT for parathyroid localization in hyperparathyroidism: a systematic review and meta-analysis. Horm Cancer. 2018;9:440–7.
Orevi M, Freedman N, Mishani E, Bocher M, Jacobson O, Krausz Y. Localization of parathyroid adenoma by 11C-choline PET/CT: preliminary results. Clin Nucl Med. 2014;39:1033–8.
Rodgers SE, Hunter GJ, Hamberg LM, Schellingerhout D, Doherty DB, Ayers GD, Shapiro SE, Edeiken BS, Truong MT, Evans DB, Lee JE, Perrier ND. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140:932–41.
Lundstroem AK, Trolle W, Soerensen CH, Myschetzky PS. Preoperative localization of hyperfunctioning parathyroid glands with 4D-CT. Eur Arch Otorhinolaryngol. 2016;273:1253–9.
Noltes M, Coester A, van der Horst-Schrivers A, Dorgelo B, Jansen L, Noordzij W, Lemstra C, Brouwers A, Kruijff S. Localization of parathyroid adenomas using 11C-methionine pet after prior inconclusive imaging. Langenbecks Arch Surg. 2017;402:1109–17.
Yuan L, Liu J, Kan Y, Yang J, Wang X. The diagnostic value of 11C-methionine PET in hyperparathyroidism with negative 99mTc-MIBISPECT: a meta-analysis. Acta Radiol. 2017;58:558–64.
Mathey C, Keyzer C, Blocklet D, Van Simaeys G, Trotta N, Lacroix S, Corvilain B, Goldman S, Moreno-Reyes R. (18)F-Fluorocholine PET/CT is more sensitive than (11)C-methionine PET/CT for the localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism. J Nucl Med. 2022. https://doi.org/10.2967/jnumed.121.262395.
Treglia G, Piccardo A, Imperiale A, Strobel K, Kaufmann P, Prior J, Giovanella L. Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2019;46:751–65.
Evangelista L, Ravelli I, Magnani F, Iacobone M, Giraudo C, Camozzi V, Spimpolo A, Cecchin D. (18)F-choline PET/CT and PET/MRI in primary and recurrent hyperparathyroidism: a systematic review of the literature. Ann Nucl Med. 2020;34:601–19.
Ismail A, Christensen JW, Krakauer M, Søndergaard SB, Zerahn B, Nygaard B, Bennedbæk FN, Kristensen B, Jensen LT. (11)C-Choline PET/CT vs. (99m)Tc-MIBI/(123) iodide subtraction SPECT/CT for preoperative detection of abnormal parathyroid glands in primary hyperparathyroidism: a prospective, single-centre clinical trial in 60 patients. Diagnostics (Basel). 2020;10:975. https://doi.org/10.3390/diagnostics10110975.
Noltes ME, Kruijff S, Jansen L, Westerlaan HE, Zandee WT, Dierckx RAJO, Brouwers AH. A retrospective analysis of the diagnostic performance of (11)C-choline PET/CT for detection of hyperfunctioning parathyroid glands after prior negative or discordant imaging in primary hyperparathyroidism. EJNMMI Res. 2021;11:32–7.
Tian Y, Tanny S, Einsiedel P, Lichtenstein M, Stella D, Phal P, Miller J. Four-dimensional computed tomography: clinical impact for patients with primary hyperparathyroidism. Ann Surg Oncol. 2018;25:117–21.
Yeh R, Tay Y, Tabacco G, Dercle L, Kuo J, Bandeira L, McManus C, Leung D, Lee J, Bilezikian J. Diagnostic performance of 4D CT and sestamibi SPECT/CT in localizing parathyroid adenomas in primary hyperparathyroidism. Radiology. 2019;291:469–76.
Noltes ME, Brands S, Dierckx RAJO, Jager PL, Kelder W, Brouwers AH, Francken AB, Kruijff S. Non-adherence to consensus guidelines on preoperative imaging in surgery for primary hyperparathyroidism. Laryngoscope Investig Otolaryngol. 2020;5:1247–53.
Bilezikian JP, Khan AA, Silverberg SJ, Fuleihan GE, Marcocci C, Minisola S, Perrier N, Sitges-Serra A, Thakker RV, Guyatt G, Mannstadt M, Potts JT, Clarke BL, Brandi ML, International Workshop on Primary Hyperparathyroidism. Evaluation and management of primary hyperparathyroidism: summary statement and guidelines from the Fifth International Workshop. J Bone Miner Res 2022. https://doi.org/10.1002/jbmr.4677.
Bollerslev J, Rejnmark L, Zahn A, Heck A, Appelman-Dijkstra NM, Cardoso L, Hannan FM, Cetani F, Sikjær T, Formenti AM, Björnsdottir S, Schalin-Jantti C, Belaya Z, Gibb FW, Lapauw B, Amrein K, Wicke C, Grasemann C, Krebs M, Ryhänen EM, Makay O, Minisola S, Gaujoux S, Bertocchio JP, Hassan-Smith ZK, Linglart A, Winter EM, Kollmann M, Zmierczak HG, Tsourdi E, Pilz S, Siggelkow H, Gittoes NJ, Marcocci C, Kamenicky P. PARAT Working Group Collaborators. European Expert Consensus on Practical Management of Specific Aspects of Parathyroid Disorders in Adults and in Pregnancy: Recommendations of the ESE Educational Program of Parathyroid Disorders Eur J Endocrinol. 2021;186(2):33–63. https://doi.org/10.1530/EJE-21-1044.
Connor RJ. Sample size for testing differences in proportions for the paired-sample design. Biometrics. 1987;43:207–11.
Newcombe RG. Interval estimation for the difference between independent proportions: comparison of eleven methods. Stat Med. 1998;17:873–90.
Chun IK, Cheon GJ, Paeng JC, Kang KW, Chung JK, Lee DS. Detection and characterization of parathyroid adenoma/hyperplasia for preoperative localization: comparison between (11)C-methionine PET/CT and (99m)Tc-sestamibi scintigraphy. Nucl Med Mol Imaging. 2013;47:166–72.
Beheshti M, Hehenwarter L, Paymani Z, Rendl G, Imamovic L, Rettenbacher R, Tsybrovskyy O, Langsteger W, Pirich C. (18)F-Fluorocholine PET/CT in the assessment of primary hyperparathyroidism compared with (99m)Tc-MIBI or (99m)Tc-tetrofosmin SPECT/CT: a prospective dual-centre study in 100 patients. Eur J Nucl Med Mol Imaging. 2018;45:1762–71.
Piccardo A, Bottoni G, Boccalatte LA, Camponovo C, Musumeci M, Bacigalupo L, Collaud C, Ugolini M, Fiz F, Trimboli P. Head-to-head comparison among (18)F-choline PET/CT, 4D contrast-enhanced CT, and (18)F-choline PET/4D contrast-enhanced CT in the detection of hyperfunctioning parathyroid glands: a systematic review and meta-analysis. Endocrine. 2021;74:404–12.
Ferrari C, Santo G, Mammucci P, Pisani AR, Sardaro A, Rubini G. Diagnostic value of choline PET in the preoperative localization of hyperfunctioning parathyroid gland(s): a comprehensive overview. Biomedicines. 2021;9:231. https://doi.org/10.3390/biomedicines9030231.
Zajíčková K, Zogala D, Kubinyi J. Parathyroid imaging by (18)F-fluorocholine PET/CT in patients with primary hyperparathyroidism and inconclusive conventional methods: clinico-pathological correlations. Physiol Res. 2018;67:S551–7.
Mahajan A, Starker LF, Ghita M, Udelsman R, Brink JA, Carling T. Parathyroid four-dimensional computed tomography: evaluation of radiation dose exposure during preoperative localization of parathyroid tumors in primary hyperparathyroidism. World J Surg. 2012;36:1335–9.
Hoang JK, Reiman RE, Nguyen GB, Januzis N, Chin BB, Lowry C, Yoshizumi TT. Lifetime attributable risk of cancer from radiation exposure during parathyroid imaging: comparison of 4D CT and parathyroid scintigraphy. AJR Am J Roentgenol. 2015;204:579.
Raeymaeckers S, De Brucker Y, Vanderhasselt T, Buls N, De Mey J. Detection of parathyroid adenomas with multiphase 4DCT: towards a true four-dimensional technique. BMC Med Imaging. 2021. https://doi.org/10.1186/s12880-021-00597-1.
Moosvi SR, Smith S, Hathorn J, Groot-Wassink T. Evaluation of the radiation dose exposure and associated cancer risks in patients having preoperative parathyroid localization. Ann R Coll Surg Engl. 2017. https://doi.org/10.1308/rcsann.2017.0014.
Hinson AM, Lee DR, Hobbs BA, Fitzgerald RT, Bodenner DL, Stack BC Jr. Preoperative 4D CT localization of nonlocalizing parathyroid adenomas by ultrasound and SPECT-CT. Otolaryngol Head Neck Surg. 2015. https://doi.org/10.1177/0194599815599372.
Kluijfhout WP, Pasternak JD, Beninato T, Drake FT, Gosnell JE, Shen WT, Duh Q, Allen IE, Vriens MR, de Keizer B, Hope TA, Suh I. Diagnostic performance of computed tomography for parathyroid adenoma localization; a systematic review and meta-analysis. Eur J Radiol. 2017. https://doi.org/10.1016/j.ejrad.2017.01.004.
Sun L, Yao J, Hao P, Yang Y, Liu Z, Peng R. Diagnostic role of four-dimensional computed tomography for preoperative parathyroid localization in patients with primary hyperparathyroidism: a systematic review and meta-analysis. Diagnostics (Basel). 2021. https://doi.org/10.3390/diagnostics11040664.
Kattar N, Migneron M, Debakey MS, Haidari M, Pou AM, McCoul ED. Advanced computed tomographic localization techniques for primary hyperparathyroidism: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2022. https://doi.org/10.1001/jamaoto.2022.0271.
Noltes M, Kruijff S, Noordzij W, Telenga E, Vállez García D, Trofimiuk-Müldner M, Opalińska M, Hubalewska-Dydejczyk A, Luurtsema G, Dierckx R, El Moumni M, Boellaard R, Brouwers A. Optimization of parathyroid 11C-choline PET protocol for localization of parathyroid adenomas in patients with primary hyperparathyroidism. EJNMMI Res. 2019;31:9–73.
Evangelista L, Ravelli I, Magnani F, Iacobone M, Giraudo C, Camozzi V, Spimpolo A, Cecchin D. (18)F-choline PET/CT and PET/MRI in primary and recurrent hyperparathyroidism: a systematic review of the literature. Ann Nucl Med. 2020. https://doi.org/10.1007/s12149-020-01507-1.
Prabhu M, Kumari G, Damle NA, Arora G, Kumar P, Kumar R, Tripathi M, Bal C, Khadgawat R, Kumar C, Agarwal S. Assessment of the role of early dynamic PET/CT with 18F-fluorocholine in detection of parathyroid lesions in patients with primary hyperparathyroidism. Nucl Med Commun. 2018. https://doi.org/10.1097/MNM.0000000000000924.
Broos WAM, Wondergem M, Knol RJJ, van der Zant FM. Parathyroid imaging with (18)F-fluorocholine PET/CT as a first-line imaging modality in primary hyperparathyroidism: a retrospective cohort study. EJNMMI Res. 2019. https://doi.org/10.1186/s13550-019-0544-3.
Cuderman A, Senica K, Rep S, Hocevar M, Kocjan T, Sever MJ, Zaletel K, Lezaic L. (18)F-Fluorocholine PET/CT in primary hyperparathyroidism: superior diagnostic performance to conventional scintigraphic imaging for localization of hyperfunctioning parathyroid glands. J Nucl Med. 2020. https://doi.org/10.2967/jnumed.119.229914.
Broos WAM, Wondergem M, van der Zant FM, Knol RJJ. Dual-Time-Point (18)F-Fluorocholine PET/CT in parathyroid imaging. J Nucl Med. 2019. https://doi.org/10.2967/jnumed.118.225599.
Funding
This research has received funding from the Foundation de Cock-Hadders (project number 2019–51).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by M. E. N, S. K., A. P. A. A., A. H., and A. H. B. The first draft of the manuscript was written by M. E. N., and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was registered at the Netherlands Trial Register (NTR7423) and approved by the Research Ethics Board of the University Medical Center Groningen, The Netherlands (METc 2018/330). This study was performed in line with the principles of the Declaration of Helsinki. Written informed consent was obtained from all subjects.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Noltes, M.E., Kruijff, S., Appelman, A.P.A. et al. Head-to-head comparison of [11C]methionine PET, [11C]choline PET, and 4-dimensional CT as second-line scans for detection of parathyroid adenomas in primary hyperparathyroidism. Eur J Nucl Med Mol Imaging 51, 1050–1059 (2024). https://doi.org/10.1007/s00259-023-06488-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06488-7