Abstract
For older Caucasian women and men, the QCT (quantitative CT) lumbar spine (LS) bone mineral density (BMD) threshold for classifying osteoporosis is 80 mg/ml. It was recently proposed that, for older East Asian women, the QCT LS BMD value equivalent to the Caucasian women’s threshold of 80 mg/mL is about 45∼50 mg/ml. For a data of 328 cases of Chinese men (age: 73.6 ± 4.4 years) who had QCT LS BMD and DXA LS BMD at the same time and with the DXA BMD value of ≤ 0.613 g/cm2 to classify osteoporosis, the corresponding QCT LS BMD threshold is 53 mg/ml. Osteoporotic-like vertebral fracture sum score (OLVFss) ≤ -2.5 has been proposed to diagnose osteoporosis. For 316 cases of Chinese men (age:73.7±4.5 years), OLVFss ≤ -2.5 defines an osteoporosis prevalence of 4.4%; to achieve this osteoporosis prevalence, the corresponding QCT LS BMD value is < 47.5 mg/ml. In the China Action on Spine and Hip Status study, a Genant grades 2/3 radiographic ‘osteoporotic vertebral fracture’ prevalence was 2.84% for Chinese men (total n = 1267, age: 62.77 ± 9.20 years); to achieve this osteoporosis prevalence, the corresponding BMD value was < 42.5 mg/ml. In a study of 357 Beijing older men, according to the clinical fragility fracture prevalence and femoral neck DXA T-score, the QCT LS BMD value to classify osteoporosis was between 39.45 mg/ml and 51.38 mg/ml. For older Chinese men (≥ 50 years), we recommend the cutpoint for the QCT LS BMD definition of osteoporosis to be 45∼50 mg/ml which is the same as the value for Chinese women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Osteoporosis is a systemic skeletal disease characterised by a reduction in bone mass (measured by bone mineral density: BMD) and qualitative skeletal changes that cause an increase in bone fragility and a higher fracture risk. The clinical significance of osteoporosis lies in the fragility fractures (FF) that occur. Numerous studies have demonstrated that the skeleton of East Asians has microstructural and mechanical advantages [1, 2]. For example, Walker et al. [3, 4] reported that postmenopausal Chinese women have a higher trabecular plate-to-rod ratio and greater whole bone stiffness, translating into greater trabecular mechanical competence despite smaller bone size compared to Caucasian women. For the spine, compared with older Caucasians, older Chinese are less likely to have disc space narrowing, thoracic spine hyper-kyphosis, vertebral osteoarthritic wedging, Schmorl nodes defect, and degenerative spondylolisthesis [5, 6]. Compared with British men and women, Japanese men and women were also noted to be less likely to have lumbar spine radiographs osteoarthritic changes graded as Kellgren-Lawrence 4 severity [7]. Compared with Caucasians, East Asians are known to have a lower incidence rate of back pain [5]. Waterman et al. [8] queried the National Electronic Injury Surveillance System (USA) for all cases of low back pain presented to emergency departments between 2004 and 2008. They found that the per 1,000 person-years low back pain incident rates were 1.23 among whites, while only 0.20 among Asians. Almost all of the published results comparing East Asians and Caucasians show nearly all FF prevalences, including hip fracture, vertebral fracture, and humerus fracture, are no more than half that of older Caucasians, both for men and women (reviewed in [9, 10]). Figure 1).
Lower hip fragility fracture (FF) in Asian men relative to Caucasian men (A, B), lower clinical vertebral FF in men relative to women (C), and lower clinical vertebral FF in East Asian men relative to Caucasian men (D). A: Hip Fracture Rates in Hong Kong and the United States, 1988 through 1989. Data re-plotted from [17]. B: Age-standardized hip fracture incidence in men from 2002 to 2008 for US Medicare beneficiaries (≥ 65 years old). Data re-plotted from Wright et al. J Bone Miner Res 2012;27:2325–32. Data in (C) and (D) are from ‘Osteoporosis Fracture in Men (Hong Kong)’ study, ‘Osteoporosis Fracture in Women (Hong Kong)’ study, Freitas et al. Osteoporos Int 2008;19:615–23 (MrOS USA study), Sanders et al. Osteoporos Int 1999;10:240–7 (Geelong study), and Cooper et al. J Bone Miner Res 1992;7:221–7 (Rochester study), Sakuma et al., J Bone Miner Metab 2008;26:373–8 (Japan Sado 2004), Imai et al., J Bone Miner Metab 2019;37:484–90 (Japan Sado 2015)
Quantitative CT (QCT) for BMD measurement can be performed on any CT scanner with the use of a calibration phantom. The most common form of QCT provides a trabecular bone measurement [11]. It is expected that the application of QCT for spine BMD will increase, particularly in the settings of opportunistic screening where chest/abdominal CT are conducted for an indication other than osteoporosis. Spine BMD can be simultaneously measured with these chest/abdominal CT scans [12]. For older Caucasian women and men (≥ 50 years), the QCT lumbar spine (LS) BMD cutpoint value for osteoporosis has been recommended to be 80 mg/ml [13, 14]. Instead of applying the Caucasian value of 80 mg/ml, we recently proposed that, for older East Asian women (≥ 50 years), the QCT LS BMD value equivalent to the Caucasian women’s threshold of 80 mg/mL is about 45∼50 mg/ml [15, 16]. FF in men have different features compared with FF in women. FF prevalence in men is no more than half of that in age-matched women (Fig. 1 C, D), this is the same for Caucasian populations and for Chinese population [10, 17, 18]. This article discusses whether QCT LS BMD 45∼50 mg/ml is also a suitable cutpoint value for classifying osteoporosis in older Chinese men.
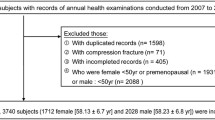
Firstly, a correlation analysis was conducted with the data of 328 cases of Chinese men (age: 73.6 ± 4.4 years) who had QCT LS BMD and DXA (dual-energy x-ray absorptiometry) LS BMD at the same time. These data are from the Osteoporotic Fracture in Men (MrOS) Hong Kong study year-2 follow-up conducted during the period of September 2003 to March 2005. The result is shown in Fig. 2A. With the Hong Kong local reference, we recommended the DXA LS BMD cutpoint value for classifying osteoporosis in Chinese men to be 0.613 g/cm2 (Hologic densitometer) [10, 19]. Following this, Fig. 2A shows the QCT LS BMD threshold for classifying osteoporosis is 53 mg/ml. This result forms the cornerstone of the analyses of the current article, and it is in agreement with other studies such as the mixed-sex cohort study of Chen et al. (Fig. 2B) [20], Lin et al. [21], and Uemura et al. [22].
Correlation analyses of LS (lumbar spine) BMD measured by QCT and LS BMD measured by DXA. A: 328 Chinese men (age: 73.6 ± 4.4 years) who had QCT LS (L1 and L2) BMD and DXA LS BMD at the same time. The data are from Osteoporotic Fracture in Men (MrOS) Hong Kong year-2 follow-up study. The DXA BMD cutpoint value to define osteoporosis is 0.613 g/cm2 (Hologic densitometer) [10], and the corresponding QCT BMD is 53 mg/ml. For QCT value of 50 mg/ml, the corresponding DXA BMD value is 0.594 g/cm2. B: Results of mixed-sex 48 primary hyperparathyroidism patients (age: 53.77 ± 11.04 years) reported by Chen et al. [20]. The blue dotted crosses show the relationship between DXA measure and QCT measure in (B) is approximately similar to that in (A)
Secondly, evidence shows QCT LS BMD 45∼50 mg/ml defined osteoporosis is approximately equal to the osteoporosis prevalence defined by radiographic FF or clinical FFs (Table 1). We have recently proposed an index, i.e., osteoporotic-like vertebral fracture sum score (OLVFss), to diagnose osteoporosis [23, 24]. For Chinese men, OLVFss ≤ -2.5 suggests the diagnosis of osteoporosis with the prevalence based on the lowest DXA T-score of femoral neck, total hip, and LS; and among Chinese population the lowest T-score is most likely being the LS T-score [19, 24]. We analysed 316 cases (age: 73.69 ± 4.46 years) of MrOS (Hong Kong) participants with QCT LS BMD and spine radiograph, and the results show OLVFss ≤ -2.5 define osteoporosis prevalence of 4.4% (Fig. 3); to achieve this osteoporosis prevalence, the corresponding QCT LS BMD value is < 47.5 mg/ml. This result is supported by a number of other approximated evidences. Deng et al. [25] reported that, for the 70–79 years old group MrOS (Hong Kong) participants (n = 1128), the prevalence of Genant grades 2/3 radiographic ‘osteoporotic’ vertebral fracture is 5.23%. In the CASH (China Action on Spine and Hip Status) study, Liu et al. [26] reported a Genant grades 2/3 radiographic ‘osteoporotic’ vertebral fracture prevalence of 2.84% for their sample (total n = 1267, age: 62.77 ± 9.20 years); and to achieve this osteoporosis prevalence, the corresponding QCT LS BMD value was < 42.5 mg/ml. Yuan et al. [27] studied 357 older men in Beijing, and according to the clinical FF prevalence (i.e., 6.7%) and femoral neck DXA T-score defined osteoporosis prevalence (i.e., 12.3%), the corresponding QCT LS BMD value to classify osteoporosis was between 39.45 mg/ml and 51.38 mg/ml.
Percentage of osteoporosis defined by OLVFss (osteoporotic-like vertebral fracture sum score) and QCT LS (lumbar spine L1 and L2) BMD. OLVFss ≤ -3, ≤ -2.5, ≤ -2.0, ≤ -1.5, ≤ -1.0, ≤ -0.5 defines 2.52%, 4.43%, 6.01%, 12.65%, 17.41%, and 35.44% of the study subjects (n = 316, mean age: 73.7 years) being osteoporotic, respectively. The recommended OLVFss for defining osteoporosis is ≤ -2.5 [24], and this defines osteoporosis prevalence being 4.43% for this sample. QCT LS BMD of 47.5 mg/ml, 50 mg/ml, 80 mg/ml defines 4.43%, 5.06%, and 31.32% of the subjects being osteoporotic, respectively. Data are from MrOS(Hong Kong) study for Chinese men (Table 1)
There are limitations to the analyses in this article. The main limitation is that analyses of DXA LS BMD and OLVFss in this study are based on the extrapolation (with adjustment according to FF risk profile of Chinese men) of the definition that DXA T-score of Caucasian men for classifying osteoporosis is the same as that of for Caucasian women, i.e. both being -2.5 [10, 24]. There have been some controversies on whether it is appropriate for men and women to share the same osteoporosis diagnosis T-score [28]. However, DXA lumbar spine and femoral neck T-score of Caucasian men for classifying osteoporosis is the same as that of for Caucasian women, i.e. ≤ -2.5, is the currently accepted threshold and has been endorsed by various guidelines [14]. BMD is only one of the contributors to bone strength and bone strength is one of the contributors to fragility fracture risk. Moreover, there is evidence that the association between lower BMD and FF risk is stronger in women than in men [24]. However, a ‘working’ cutpoint value, despite maybe being imperfect, is urgently needed in the current clinical practice.
In conclusion, while there have been fewer results available for men than for women, the data analyses in this article based on DXA LS BMD and QCT LS BMD correlation and supported by the relationship between lower QCT LS BMD and prevalence of fragility fracture consistently suggest that, for older Chinese men (≥ 50 years), the cutpoint for the QCT LS BMD classification of osteoporosis is 45∼50 mg/ml which is the same value as for Chinese women. It is desirable that studies with higher power will be available in the future to further confirm this new osteoporosis cutpoint value. It will be practically convenient if the same cutpoint value is used for both Chinese women and men, i.e., the same as the approach for Caucasians where the same value is applied for women and men. It is likely inappropriate to apply QCT LS BMD 80 mg/ml as a cutpoint value for defining osteoporosis to all ethnic groups worldwide. With the value for Caucasians as the reference, it may be worthwhile to review this cutpoint value for other ethnic groups from Africa and Latin America as well. An ethnic group specific diagnostic criterion will allow a more meaningful comparison of disease burden among different countries, and allow comparable medication intervention thresholds for different ethnic groups.
References
Cong E, Walker MD. The Chinese skeleton: insights into microstructure that help to explain the epidemiology of fracture. Bone Res. 2014;2:14009.
Himič V, Syrmos N, Ligarotti GKI, Kato S, Fehlings MG, Ganau M. The role of genetic and epigenetic factors in determining the risk of spinal fragility fractures: new insights in the management of spinal osteoporosis. Quant Imaging Med Surg. 2023;13:7632–45.
Walker MD, Liu XS, Zhou B, Agarwal S, Liu G, McMahon DJ, Bilezikian JP, Guo XE. Premenopausal and postmenopausal differences in bone microstructure and mechanical competence in Chinese-American and white women. J Bone Miner Res. 2013;28:1308–18.
Walker MD, Shi S, Russo JJ, Liu XS, Zhou B, Zhang C, Liu G, McMahon DJ, Bilezikian JP, Guo XE. A trabecular plate-like phenotype is overrepresented in Chinese-American versus Caucasian women. Osteoporos Int. 2014;25:2787–95.
Wáng YXJ, Deng M, Griffith JF, Kwok AWL, Leung JCS, Lam PMS, Yu BWM, Leung PC, Kwok TCY. “Healthier Chinese spine”: an update of osteoporotic fractures in men (MrOS) and in women (MsOS) Hong Kong spine radiograph studies. Quant Imaging Med Surg. 2022;12:2090–105.
Wáng YXJ, Diacinti D, Iannacone A, Kripa E, Leung JCS, Kwok TCY, Diacinti D. A comparison of radiographic degeneration features of older Chinese women and older Italian Caucasian women with a focus on thoracic spine. Aging Clin Exp Res. 2023;35:2583–91.
Yoshimura N, Dennison E, Wilman C, Hashimoto T, Cooper C. Epidemiology of chronic disc degeneration and osteoarthritis of the lumbar spine in Britain and Japan: a comparative study. J Rheumatol. 2000;27:429–33.
Waterman BR, Belmont PJ Jr, Schoenfeld AJ. Low back pain in the United States: incidence and risk factors for presentation in the emergency setting. Spine J. 2012;12:63–70.
Wáng YXJ. Fragility fracture prevalence among elderly Chinese is no more than half of that of elderly Caucasians. Quant Imaging Med Surg. 2022;12:874–81.
Wáng YXJ, Xiao BH. Estimations of bone mineral density defined osteoporosis prevalence and cutpoint T-score for defining osteoporosis among older Chinese population: a framework based on relative fragility fracture risks. Quant Imaging Med Surg. 2022;12:4346–60.
Link TM, Lang TF. Axial QCT: clinical applications and new developments. J Clin Densitom. 2014;17:438–48.
Engelke K, Chaudry O, Bartenschlager S. Opportunistic screening techniques for analysis of CT scans. Curr Osteoporos Rep. 2023;21:65–76.
Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, et al. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD Official Positions. J Clin Densitom. 2008;11:123–62.
Expert Panel on Musculoskeletal Imaging; Yu JS, Krishna NG, Fox MG, Blankenbaker DG, Frick MA, Jawetz ST, Li G, Reitman C, Said N, Stensby JD, Subhas N, Tulchinsky M, Walker EA, Beaman FD. ACR Appropriateness Criteria Osteoporosis and Bone Mineral Density: 2022 Update. J Am CollRadiol 2022;19:S417-S432
Wáng YXJ, Blake GM, Tang SN, Guermazi A, Griffith JF. Quantitative CT lumbar spine BMD cutpoint value for classifying osteoporosis among older East Asian women should be lower than the value for Caucasians. Skeletal Radiol. 2024. https://doi.org/10.1007/s00256-024-04632-4.
Wáng YXJ, Yu W, Leung JCS, Griffith JF, Xiao BH, Diacinti D, Guermazi A, Chan WP, Blake GM. More evidence to support a lower quantitative computed tomography (QCT) lumbar spine bone mineral density (BMD) cutpoint value for classifying osteoporosis among older East Asian women than for Caucasians. Quant Imaging Med Surg. 2024;14:3239–47.
Ho SC, Bacon WE, Harris T, Looker A, Maggi S. Hip fracture rates in Hong Kong and the United States, 1988 through 1989. Am J Public Health. 1993;83:694–7.
Bow CH, Cheung E, Cheung CL, Xiao SM, Loong C, Soong C, Tan KC, Luckey MM, Cauley JA, Fujiwara S, Kung AW. Ethnic difference of clinical vertebral fracture risk. Osteoporos Int. 2012;23:879–85.
Wáng YXJ, Griffith JF, Blake GM, Diacinti D, Xiao BH, Yu W, et al. Revision of the 1994 World Health Organization T-score definition of osteoporosis for use in older East Asian women and men to reconcile it with their lifetime risk of fragility fracture. Skeletal Radiol. 2024;53:609–25.
Chen L, Pan Y, Zhong F, Yuan TJ, Wang H, Chen T, Lv H, Cheng X, Liu JM, Lu Y. Using QCT to evaluate bone mineral and abdominal adipose changes in patients with primary hyperparathyroidism and comparing it to DXA for bone status assessment: a retrospective case-control study. Ann Transl Med. 2022;10:606.
Lin W, He C, Xie F, Chen T, Zheng G, Yin H, Chen H, Wang Z. Quantitative CT screening improved lumbar BMD evaluation in older patients compared to dual-energy X-ray absorptiometry. BMC Geriatr. 2023;23:231.
Uemura K, Fujimori T, Otake Y, Shimomoto Y, Kono S, Takashima K, et al. Development of a system to assess the two- and three-dimensional bone mineral density of the lumbar vertebrae from clinical quantitative CT images. Arch Osteoporos. 2023;18:22.
Wáng YXJ, Diacinti D, Aparisi Gómez MP, Santiago FR, Becce F, Tagliafico AS, Prakash M, Isaac A, Dalili D, Griffith JF, Guglielmi G, Bazzocchi A. Radiological diagnosis of prevalent osteoporotic vertebral fracture on radiographs: an interim consensus from a group of experts of the ESSR osteoporosis and metabolism subcommittee. Skeletal Radiol. 2024. https://doi.org/10.1007/s00256-024-04678-4.
Wáng YXJ, Leung JCS, Lam PMS, Kwok TCY. Conversion of osteoporotic-like vertebral fracture severity score to osteoporosis T-score equivalent status: A framework study for older Chinese men. Osteoporos Sarcopenia. 2023;9:14–21.
Deng M, Zeng XJ, He LC, Leung JCS, Kwok AWL, Griffith JF, et al. Osteoporotic Vertebral Fracture Prevalence in Elderly Chinese Men and Women: A Comparison of Endplate/Cortex Fracture-Based and Morphometrical Deformity-Based Methods. J Clin Densitom. 2019;22:409–19.
Liu Y, Yu A, Li K, Wang L, Huang P, Geng J, Zhang Y, Duanmu YY, Blake GM, Cheng X. Differences in spine volumetric bone mineral density between grade 1 vertebral fracture and non-fractured participants in the China action on spine and hip status study. Front Endocrinol (Lausanne). 2022;13:1013597.
Yuan Y, Zhang P, Tian W, Deng X, Yue R, Ge X, Li X. Application of bone turnover markers and DXA and QCT in an elderly Chinese male population. Ann Palliat Med. 2021;10:6351–8.
Kanis JA, Melton LJ, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9:1137–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
A.G. is a Shareholder of BICL, LLC and Consultant to Pfizer, ICM, TrialSpark, TissueGene, Coval, Medipost, and Novartis. Other authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wáng, Y.X.J., Chan, W.P., Yu, W. et al. Quantitative CT lumbar spine BMD cutpoint value for classifying osteoporosis among older Chinese men can be the same as that of older Chinese women, both much lower than the value for Caucasians. Skeletal Radiol (2024). https://doi.org/10.1007/s00256-024-04722-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00256-024-04722-3