Abstract
Previous epidemiological study showed that most of the porcine enterotoxin Escherichia coli (ETEC) strains harbor multiple enterotoxins but lack any of the fimbriae or non-fimbrial adhesion genes. Therefore, effective ETEC vaccines need to aim directly at all the enterotoxin antigens. The objective of this study was to evaluate the simultaneous immune effect of two live attenuated E. coli strains expressing LTR192G-STaA13Q and LTR192G-STb fusion immunogen, respectively. The results showed that both local mucosal and systemic immune responses against LT, STa, STb, and F41 were induced in BALB/c mice immunized orally with the recombinant E. coli strains ER-A and ER-B simultaneously. In addition, results of cellular immune responses showed that stimulation index (SI) values of immunized mice were significantly higher than control mice (P < 0.05) and a marked shift toward type-2 helper T lymphocyte (Th 2) immunity. Moreover, the induced antibodies demonstrated neutralizing effects on LT, STa, and STb producing E. coli infection. These data indicated that the use of recombinant E. coli ER-A and ER-B could be a valuable strategy for future polyvalent vaccine development of ETEC.
Similar content being viewed by others
Introduction
Enterotoxigenic Escherichia coli (ETEC) strains cause high morbidity and mortality in piglets and therefore are one of the most economically important diseases in swine husbandry worldwide (Liu et al. 2014b). The virulence factors of ETEC strain in diarrhea include fimbriae/non-fimbrial adhesions and enterotoxins. Fimbriae/non-fimbrial adhesions mediate ETEC strains for attachment to porcine small intestinal epithelial cells and subsequent colonization, whereas enterotoxins disrupt fluid homeostasis in host small intestinal epithelial cells to cause fluid and electrolyte hypersecretion that leads to diarrhea (Ruan et al. 2011).
Vaccination of special ETEC vaccines to pigs is a better way for protecting swinery against ETEC infection (Feng et al. 2013; You et al. 2011). However, there are no effective vaccines currently available that provide broad protection against porcine ETEC infections in China (Liu et al. 2014b). Furthermore, a recent epidemiological study showed that more than half of the porcine ETEC strains did not carry any of the fimbriae or non-fimbrial adhesion genes, and these ETEC strains generally harbor multiple enterotoxins that have a synergistic effect in enhancing pathogenicity, making it challenging to control diarrhea of young pigs (Liu et al. 2014b). Additionally, the distribution and frequency of enterotoxins can vary considerably from region to region and over time in a given region (Liu et al. 2014b). Therefore, effective ETEC vaccines need to aim directly at the enterotoxin antigens, and polyvalent vaccines, designed to stimulate immune responses against all enterotoxins, including heat-labile enterotoxin (LT) and heat-stable enterotoxins (STa and STb), might be more suitable for preventing ETEC infection in piglets.
Currently, subunit vaccines available are delivery by injection, with problems of requiring a large vaccine dose, repeated administration, high cost in preparation, being less safe, inconvenience for immune, and stress reaction for animals (Zhao et al. 2012). To overcome these shortcomings, the potential development of oral vaccines to deliver heterologous antigen to the mucosal immune system has been proposed. Oral vaccines are easy to administer, safe, adequate for large-scale immunization, and stable without refrigeration (if lyophilized) (Kotton and Hohmann 2004). In addition, oral delivery vaccines could induce both systemic and mucosal immune responses. Moreover, mucosal surfaces are prominent in the gastrointestinal, urogenital, and respiratory tracts and provide portals of entry for pathogens (Qiao et al. 2009). The mucosal immune system secretes a great quantity of secretory immunoglobulin A (sIgA) antibodies, which created the critical first line of defense against invasion of deeper tissue by the pathogens (Liu et al. 2011). Therefore, oral vaccination could be an effective strategy for infection prevention by induction of systemic and mucosal immune responses.
Previously, we develop two attenuated recombinant E. coli strains expressing LT192-STa13 (Liu et al. 2014a) and LT192-STb fusion immunogen, respectively, and evaluated its potential as oral vaccines. In this study, we further evaluated the immunological effect during oral vaccination with the two recombinant E. coli strains in a mice model simultaneously. Data showed that oral immunization of the two E. coli strains elicited strong systemic and mucosal immune responses, indicating that such immune strategy may be useful for developing oral polyvalent antitoxin vaccines to control ETEC disease.
Materials and methods
Bacterial strains and cells
Recombinant E. coli strain O142(yaiT::LT192-STa13) (ER-A) was generated in previous study (Liu et al. 2014a). This strain was constructed by inserting the LT192-STa13 cassette into the yaiT pseudogene located at the genome of an attenuated wild-type E. coli, which was derived by deleting the toxin gene by using the homologous recombination method (Liu et al. 2014a). Similarly, the E. coli strain O142(yaiT:: LT192-STb) (ER-B) was constructed by inserting the LT192-STb cassette into the genome of the attenuated wild-type E. coli as mentioned above (Liu et al., unpublished data). Briefly, the E. coli O142 parent strain was a field-isolated strain and was deposited in the China Veterinary Culture Collection Center (CVCC: C83920). The LT192 toxoid was generated by mutating the 192nd amino acid (AGA to GGA) of LT toxin gene (GenBank: CP002732.1), and the STa13 toxoid was generated by mutating the 13th amino acid (GCC to CAG) of 18-amino-acid STa mature peptide gene (GenBank: V00612.1). In addition, the LT192-STa13 cassette was constructed by fusing LT192 and STa13 with a 5′-GGGCCGGGGCCC-3′ linker, and the LT192-STb cassette was constructed by fusing LT192 and STb gene (GenBank: AY028790.1) with a 5′-CGAGCTCGGTACCCGGGGATC-3′ linker. The illustration of ER-A and ER-B is shown in Fig. 1. Pig small intestine cell lines ZYM-DIEC02 were kindly provided by Prof. Yijing Li (Northeast Agricultural University, China)
Colonization study of recombinant E. coli strains in animal intestine
The recombinant E. coli strains ER-A and ER-B were induced to nalidixic acid resistance (Nal R). Six-week-old BALB/c mice were obtained from the Liaoning Changsheng Biotechnology Co., Ltd., China, and were divided into two groups. A group of 10 mice were fed approximately 109 colony-forming units (CFU) of ER-A (Nal R) and ER-B (Nal R). Another group of 10 mice was orally fed with sterile phosphate buffer saline (PBS) as the control. The fecal samples of mice were collected on days 0, 7, 14, 21, 28, 35, and 42 and incubated at LBNal agar plates. The colonies were analyzed by specific PCR to identify the ER-A(Nal R) (Liu et al. 2014a) and the ER-B(Nal R) (Liu et al., submitted) as previously described.
Oral vaccination experiments
ER-A and ER-B were resuspended in milk to a concentration of 1010 CFU/mL. Female six-week-old BALB/c mice (n = 40) were divided into four groups. The groups of A and B were orally inoculated with 109 cells of ER-A and ER-B simultaneously. The groups of C1 and C2 received 0.1-mL doses of milk. Mice in all groups were immunized on days 0, 14, and 28. Mice in groups B and C2 were coupled with equivalent male mice at day 21 and got pregnant by the male mice.
ELISA analysis for antibody levels
ELISA was performed as previously described (Jiang et al. 2014). Briefly, the plates was coated with F41 fimbriae (200 ng/well), lymphotoxin alpha (LTA) recombinant protein (50 ng/well), lymphotoxin beta (LTB) recombinant protein (50 ng/well), 4× STa recombinant protein (100 ng/well), and MBP-STb recombinant protein (200 ng/well) to titrate antibodies.
Lymphocyte proliferation assay and flow cytometry for cellular immune responses
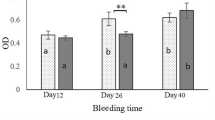
Lymphocyte proliferation assay was performed as previously described with slight modification (Hu et al. 2013; Jiang et al. 2014). Briefly, splenic lymphocytes and mesenteric lymphocytes were isolated by conventional methods by passage through sterile mesh wire screens. Cells (5 × 105/well) were added to the 96-well plates for 100 μL and stimulated in vitro with LT (10 μg/mL), STa (10 μg/mL), STb (10 μg/mL), LT192-STa13 (10 μg/mL), and LT192-STb (10 μg/mL) proteins for 100 μL, respectively. Then, 10 μg/mL of concanavalin A (con A) as a positive control was added for 100 μL. Black controls without proteins were set up. The 96-well plates were incubated at 37 °C in an incubator with 5 % CO2 for 72 h. Then, 10 μL of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) (10 mg/mL) was added into each well. After incubation for 4 h with MTT, the culture supernatant was discarded and 150 μL of dimethyl sulfoxide was added to each well and then oscillated for 15 min until the crystal dissolved. For each well, the absorbance at 570 nm (A570) was measured. The stimulation index (SI) was calculated according to the optical density (OD) values of A570 ratio and used to evaluate the proliferation of splenic lymphocytes and mesenteric lymphocytes. SIproliferation = ODsamples/ODblack control.
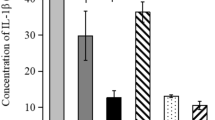
In addition, type of helper T-lymphocyte (Th)-cell-mediated immunity was determined by flow cytometry as previously described (Jiang et al. 2014). Briefly, splenic lymphocytes and mesenteric lymphocytes were prepared as mentioned above. Cells (1 × 106) were treated with FITC-anti-CD3 (Miltenyi Biotec, Germany) and APC-anti-CD8 (Miltenyi Biotec, Germany) antibody at 37 °C for 0.5 h. After washing, cells were treated with phycoerythrin (PE)-anti-IFN-γ (eBiosciences, USA) and PE-anti-IL-4 (eBiosciences, USA) antibody at 37 °C for 0.5 h, respectively. After staining, cells were washed twice with PBS and resuspended in 500 μL PBS. Finally, the proportions of Th 1 (IFN-γ) and Th 2 (IL-4) were determined by flow cytometry.
In vitro neutralization ability of the induced antibodies
Serum, intestinal mucus, splenocyte lysate, and mesenteric lymphocyte lysate samples from mice immunized with recombinant E. coli strains expressing LT192-STa13 and LT192-STb fusion proteins were evaluated to determine the neutralization ability of the induced antibodies. In brief, samples from mice fed milk were used as the negative control. The 50 μL of filter-sterilized enterotoxins (STa, STb, and LT) in twofold serial dilutions was prepared and mixed with equal volume of samples from immunized mice for 2 h at 37 °C. Then, the antibody-toxin mixture was added to the ZYM-DIEC02 cells and incubated in a 5 % CO2 incubator at 37 °C for 24 h. Then, the change of the cells was observed.
In vivo neutralization ability of the induced antibodies to STa and STb toxins
In vivo neutralization ability of the induced antibodies to STa and STb toxins was determined using the suckling mouse assay as described previously with slight modifications (You et al. 2011). Briefly, the 50 μL of STa or STb toxins in serial dilutions was mixed with equal volume of samples from immunized mice for 2 h at 37 °C, and then, soybean trypsin inhibitor (2 mg/mL; Solarbio, Beijing, China) was added (testing the toxicity of STb) or not (testing the toxicity of STa). Suckling mice of 4 days were inoculated intragastrically with 100 μL of the antibody-toxin mixture and killed after 4-h inoculation. G/C (weight ratio of gut to the remaining carcass) ratios of ≥0.090 were considered positive for toxicity of STa or STb. Samples from mice fed milk were used as the negative control. In each toxin dilution, the antibody-toxin mixtures were inoculated with four suckling mice, and mean values and standard deviations of G/C ratio were determined.
Suckling mice challenge after birth by the immunized pregnant mice
The protective efficacy of passive immunization with lac feminium from the immunized pregnant mice was evaluated using the suckling mouse assay as described above. Briefly, the 100 μL of STa or STb toxins in serial dilutions was mixed with soybean trypsin inhibitor (testing the toxicity of STb) or not (testing the toxicity of STa) and then fed to suckling mice on day 4 after birth by the immunized pregnant mice. After 4 h, the suckling mice were killed and considered for the G/C ratios. Suckling mice from the control group as the negative control was used. In each toxin dilution, the antibody-toxin mixtures were inoculated with four suckling mice, and mean values and standard deviations of G/C ratio were determined.
Statistical analysis
For comparing the significance of the difference between vaccinated and control groups, statistical analysis was performed using ANOVA of repeated measuring and two independent-samples t tests by SPSS version 19.0. P values of <0.05 were considered to be statistically significant.
Ethics statement
The present study did not involve endangered or protected species. The animal study complied with the Animal Welfare Act by following the NIH guidelines (NIH Pub. No. 85-23, revised 1996), and protocols were approved and supervised by the Animal Care and Use Committee of Northeast Agricultural University.
Results
Colonization ability of recombinant E. coli strains in animal intestine
The results of PCR showed the expected size from ER-A (Nal R) and ER-B (Nal R) (Fig. 2a). After statistical analysis, data showed that ER-A (Nal R) and ER-B (Nal R) were able to colonize the intestinal tract simultaneously; in contrast, no positive strains were isolated from the samples of the control group (Fig. 2b).
Colonization efficacy of recombinant E. coli ER-A(Nal R ) and ER-B(Nal R ) in intestinal tracts of mice. a PCR reaction for the verifying of the recombinant E. coli strain ER-A(Nal R ) and ER-B(Nal R ). M, molecular size marker; N, PCR negative control, 1, PCR product of ER-A(Nal R ) by using the primers A24 paired with A25; 2, PCR product of ER-B(Nal R ) by using the primers B27 paired with B28. b Quantitative bacterial colonization assay to measure colonization of the ER-A(Nal R ) and ER-B(Nal R ) at intestinal tracts of mice. Fecal samples collected from each mice were ground in PBS, serial diluted, and plated on LBNal agar plates. ER-A(Nal R ) and ER-B(Nal R ) were counted after overnight growth at 37 °C and identification by PCR
Systemic and mucosal immune responses in mice induced by oral vaccination
As the results show, there was no substantial difference in specific IgG level between experimental groups and control groups prior to intragastric immunization, while oral immunization of the two recombinant E. coli strains elicited an antigen-specific antibody response. At 14, 14, 14, 21, and 7 days after the first immunization, high levels of anti-LTA, anti-LTB, anti-STa, anti-STb, and anti-F41 IgG antibodies could be observed in animal groups that received the two recombinant E. coli strains in serum samples (Fig. 3a–e). Similarly, the specific IgG antibodies could be observed on day 42 post-first-immunization in lac feminium, spleens, mesenteric lymph nodes, and intestinal mucus samples, respectively (Fig. 3f–i). By contrast, no specific IgG level was observed from the control groups of mice. Likewise, the specific IgA level from immunized mice was also determined after immunization (Fig. 4a–i). By contrast, no specific IgA level was observed from the control groups of mice. Taken together, these results indicated that the oral immunization of both ER-A and ER-B was able to elicit both antigen-specific systemic and mucosal antibody responses.
The specific IgG response induced after intragastric immunization with ER-A and ER-B simultaneously. a Anti-LTA-specific IgG level in the serum of immunized mice. b Anti-LTB-specific IgG level in the serum of immunized mice. c Anti-STa-specific IgG level in the serum of immunized mice. d Anti-STb-specific IgG level in the serum of immunized mice. e Anti-F41-specific IgG level in the serum of immunized mice. f Specific IgG level in the lac feminium samples of immunized mice. g Specific IgG level in the spleen samples of immunized mice. h Specific IgG level in the mesenteric lymph node samples of immunized mice. i Specific IgG level in the intestinal mucus samples of immunized mice. Mean values are shown, and error bars represent standard deviations. *P < 0.05; **P < 0.01; ***P < 0.001
The specific IgA response induced after intragastric immunization with ER-A and ER-B simultaneously. a Anti-LTA-specific IgA level in the fecal samples of immunized mice. b Anti-LTB-specific IgA level in the fecal samples of immunized mice. c Anti-STa-specific IgA level in the fecal samples of immunized mice. d Anti-STb-specific IgA level in the fecal samples of immunized mice. e Anti-F41-specific IgA level in the fecal samples of immunized mice. f Specific IgA level in the spleen samples of immunized mice. g Specific IgA level in the lac feminium samples of immunized mice. h Specific IgA level in the mesenteric lymph node samples of immunized mice. i Specific IgA level in the intestinal mucus samples of immunized mice. Mean values are shown, and error bars represent standard deviations. *P < 0.05; **P < 0.01; ***P < 0.001
Cellular immune responses in mice induced by oral vaccination
The results indicated that lymphocyte proliferation from the immunized group were significantly higher than those of the control group when stimulated by specific antigens (P < 0.05). For splenic lymphocyte proliferation, the stimulation by LT (SI = 2.257 ± 0.166, P < 0.01) stimulated the most potent production of specific T-lymphocytes, followed by STb (SI = 2.136 ± 0.178, P < 0.01), LT192-STb (SI = 1.972 ± 0.177, P < 0.05), LT192-STa13 (SI = 1.885 ± 0.235, P < 0.05), and STa (SI = 1.769 ± 0.230, P < 0.05) (Fig. 5a). For mesenteric lymphocyte proliferation, the stimulation by STa (SI = 3.698 ± 0.583, P < 0.001) stimulated the most potent production of specific T-lymphocytes, followed by LT192-STb (SI = 3.605 ± 0.634, P < 0.001), STb (SI = 3.475 ± 0.498, P < 0.001), LT (SI = 3.008 ± 0.304, P < 0.001), and LT192-STa13 (SI = 2.755 ± 0.627, P < 0.01) (Fig. 5b).
Results of cellular immune responses in mice following oral immunization with recombinant E. coli strain ER-A and ER-B simultaneously. a Proliferative responses in splenic lymphocytes stimulated with different antigens. b Proliferative responses in mesenteric lymphocytes stimulated with different antigens. c Flow cytometry (FCM) assay for specific Th 1 (IFN-γ) and Th 2 (IL-4) cytokine production in mesenteric lymph node cells of mice immunized with ER-A and ER-B simultaneously. d FCM assay for specific Th 1 (IFN-γ) and Th 2 (IL-4) cytokine production in spleen cells of mice immunized with ER-A and ER-B simultaneously
The Th 1 (IFN-γ)/Th 2 (IL-4) ratio in mesenteric lymph node cells of immunized mice (ratio = 0.38) was obviously lower than in PBS-controlled mice (ratio = 1.04) (Fig. 5c). This finding indicated that simultaneous immunization of mice with ER-A and ER-B promotes a superior Th 2-biased immune response as compared with the PBS-controlled mice. In contrast, there was no obvious change of Th 1 (IFN-γ)/Th 2 (IL-4) ratio in spleen cells between immunized mice (ratio = 1.15) and the PBS-controlled mice (ratio = 1.00) (Fig. 5d).
Toxin-neutralizing activity in vitro
The neutralization ability of the induced antibodies was investigated to further detect whether the antibody responses were against LT, STa, or STb toxin. Results demonstrated that the presence of specific antibodies conferred obvious neutralizing effects on toxin infection. Samples from the immunized mice showed neutralization efficiency to LT toxin when compared with that from control mice in serum (1:10 vs. 1:25), intestinal mucus (1:15 vs. 1:25), splenocyte lysate (1:15 vs. 1:25), and mesenteric lymphocyte lysate (1:10 vs. 1:25) (Fig. 6a). Similarly, samples from the immunized mice also showed neutralization efficiency to STa toxin when compared with that from control mice in serum (1:5 vs. 1:10), intestinal mucus (1:5 vs. 1:10), splenocyte lysate (1:5 vs. 1:10), and mesenteric lymphocyte lysate (1:2.5 vs. 1:10) (Fig. 6b). Likewise, the minimum neutralizing ability of samples from the immunized mice for STb toxin causing ZYM-DIEC02 cells to death greater than that of control mice in serum (1:15 vs. 1:25), intestinal mucus (1:15 vs. 1:25), splenocyte lysate (1:15 vs. 1:25), and mesenteric lymphocytes lysate (1:10 vs. 1:25) (Fig. 6c).
In vitro neutralization assays on ZYM-DIEC02 cells. a Serum, intestinal mucus, splenocyte lysate, and mesenteric lymphocyte lysate from immunized mice showed neutralization efficiency to LT toxin when compared with that from control mice. b Serum, intestinal mucus, splenocyte lysate, and mesenteric lymphocyte lysate from immunized mice showed neutralization efficiency to STa toxin when compared with that from control mice. c Serum, intestinal mucus, splenocyte lysate, and mesenteric lymphocyte lysate from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice. The ratios on the figure were dilution gradient of toxins, the minimum inhibitory gradient of samples from the immunized mice leading ZYM-DIEC02 cells to death greater than that of control mice
Toxin-neutralizing activity in vivo by suckling mouse assay
For STa toxin, samples from the immunized mice showed neutralization efficiency when compared with that from control mice in serum (1:7.5 vs. 1:12.5), intestinal mucus (1:7.5 vs. 1:12.5), splenocyte lysate (1:10 vs. 1:15), and mesenteric lymphocyte lysate (1:7.5 vs. 1:12.5) (Fig. 7a–d). For STb toxin, samples from the immunized mice showed neutralization efficiency when compared with that from control mice in serum (1:7.5 vs. 1:12.5), intestinal mucus (1:5 vs. 1:12.5), splenocyte lysate (1:7.5 vs. 1:15), and mesenteric lymphocyte lysate (1:7.5 vs. 1:12.5) (Fig. 7e–h).
Neutralization of STa and STb activity in the suckling mice assay by samples from mice immunized with ER-A and ER-B simultaneously. The toxin–sample mixtures were made by mixing serially twofold diluted toxins in PBS with an equal volume of samples. a Serum from immunized mice showed neutralization efficiency to STa toxin when compared with that from control mice. b Intestinal mucus from immunized mice showed neutralization efficiency to STa toxin when compared with that from control mice. c Splenocyte lysate from immunized mice showed neutralization efficiency to STa toxin when compared with that from control mice. d Mesenteric lymphocyte lysate from immunized mice showed neutralization efficiency to STa toxin when compared with that from control mice. e: Serum from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice. f Intestinal mucus from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice. g: Splenocyte lysate from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice. h Mesenteric lymphocyte lysate from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice. Mean values are shown, and error bars represent standard deviations
Protection efficacy of the suckling mice after intaking milk of immunized mice
The suckling mice from the immunized pregnant mice were challenged with STa or STb toxin to test the protective efficacy of passive immunization with lac feminium. For STa toxin, G/C ratios from the immunized suckling mice had a negative value (G/C = 0.081 ± 0.002) after challenge with 1:15 diluted STa toxin, greater than that of control mice (1:25 diluted STa toxin; G/C = 0.088 ± 0.007) (Fig. 8a). Similarly, for STb toxin, G/C ratios from the immunized suckling mice also had a negative value (G/C = 0.083 ± 0.007) after challenge with 1:10 diluted STb toxin, greater than that of control mice (1:20 diluted STb toxin; G/C = 0.086 ± 0.004) (Fig. 8b).
In vivo neutralization assays on immunized suckling mice after challenge with STa and STb toxin. The suckling mice were fed STa or STb toxin in serial dilutions. a G/C ratios from the immunized suckling mice challenged with STa toxin had a negative value in 1:15 dilution, which is greater than that of control mice. b G/C ratios from the immunized suckling mice challenged with STb toxin had a positive value in 1:10 dilution, which is greater than that of control mice. Mean values are shown, and error bars represent standard deviations
Discussion
To the best of our knowledge, this is the first report of exploring a multivalent oral vaccine focusing on all the porcine ETEC enterotoxins simultaneously. The result from this study clearly demonstrated that the simultaneous oral strategy of ER-A and ER-B induce protective anti-LT, anti-STa, and anti-STb immunity simultaneously. This study constructed the oral vaccine based on an attenuated wild-type ETEC strain, which expresses the F41 fimbriae colonized at small intestinal cells of pigs (Morris et al. 1983), cattle (Morris et al. 1982), and dogs (Liu et al., unpublished data), making the oral vaccines ER-A and ER-B to overcome gastrointestinal motility mechanism and performing a more successful colonization. In addition, the delivery vehicle was E. coli, which itself may have natural adjuvant capabilities and may contribute to production of a highly immunogenic oral vaccine (Lourdault et al. 2014).
In this study, the chimeric LT192-STa13 and LT192-STb retained the native LT promoter, nucleotides coding two ribosome binding sites of LTA and LTB subunits. Thus, the chimeric antigens were expressed persistently without induction and stimulated the mucosal immune system of gastrointestinal tract for a longer time after oral administration in mice, which results in solid immune response. However, although it is possible to accurately determine the level of expressed antigen in the test tube, we cannot monitor precisely gene expression in the gastrointestinal tract. Therefore, it is necessary to update novel methods to analyze genes encoding antigens expressed in situ so as to control the efficiency and persistence of expression (Zhao et al. 2012).
In the present study, we evaluated protection and immune responses in mice model, which had been immunized with a third immunization in order to improve the efficacy of the experimental vaccine. This immune protocol was adapted from the procedure of a previous study (Challacombe 1983), which indicated that such pattern of immunization was effective consistently when particulate oral vaccines were used to immunize mice. The result clearly showed that this oral vaccine successfully elicited anti-LT, anti-STa, and anti-STb-specific immune responses after oral administration. Oral immunization is based on antigen delivery to the gastrointestinal tract, the largest mucosal surface, and the central site of IgA secretion. sIgA plays the most important role in the mucosal immune response against pathogen invasion, which mainly existed in local mucosa fluids (Liu et al. 2011). In this study, the simultaneous oral strategy induced high levels of anti-LTA, anti-LTB, anti-STa, anti-STb, and anti-F41 IgA antibodies. Statistically significant differences were observed on days 21, 21, 28, 21, and 14 for fecal samples. In addition, statistically significant differences were also observed for spleens, lac feminium, mesenteric lymph nodes, and intestinal mucus. Likewise, a similar result was observed with the detection of specific IgG. These results indicated that the oral vaccine ER-A was capable of inducing mucosal immune response producing sIgA and systemic immune response producing IgG. In addition, the SI ratio of splenocytes and mesenteric lymphocytes significantly increased after being stimulated by specific antigens (Fig. 5a–b; P < 0.05). These results demonstrated that the simultaneous oral immunization of ER-A and ER-B induced sufficient cellular immune response. Moreover, Th 1 (IFN-γ)/Th 2 (IL-4) ratio in mesenteric lymph node cells of immunized mice was obviously decreased as compared to controlled mice, which is in consistent with a previous study, indicating that LT-promoted cellular immune responses are more skewed toward Th 2 (Norton et al. 2012).
In vitro and in vivo neutralization assays were used for confirming the immune efficacy of the induced antibodies in inhibiting the enterotoxins. Results showed that serum, intestinal mucus, splenocyte lysate, and mesenteric lymphocyte lysate from immunized mice could inhibit the infection of LT, STa, and STb enterotoxins to ZYM-DIEC02 cells. In addition, these samples also showed obvious inhibition to STa and STb enterotoxins in suckling mice assay. After challenge with STa or STb toxins, lactivorous suckling mice from the immunized group showed obvious protective effect compared to that from the control group. These results indicated that this oral strategy elicited obvious neutralization antibodies against LT, STa, and STb enterotoxins. The ultimate goal for simultaneous oral immunization of ER-A and ER-B was to develop a broadly protective vaccine against ETEC infection. Due to limited resource, this study only tested the immunogenicity of the oral strategy in a mice model. However, experiments to test for protection of mice against LT, STa, and STb challenge are difficult; thus, testing the efficacy in a porcine vaccination and infection model is the next step in examining the efficacy of this vaccine formulation.
In summary, higher level of systemic and mucosal antibody immune responses was observed after immunization with ER-A and ER-B simultaneously. This study could be another step leading toward the development of multivalent vaccines against ETEC-associated porcine diarrhea, a disease caused by ETEC strains expressing multiple immunogenically distinctive virulence factors.
References
Challacombe SJ (1983) Salivary antibodies and systemic tolerance in mice after oral immunization with bacterial antigens. Ann N Y Acad Sci 409:177–193
Feng Y, Liu W, Shi D (2013) Effectiveness of egg yolk antibody against Shiga toxin II variant toxicity in vitro and in vivo. Curr Microbiol 67(4):448–453. doi:10.1007/s00284-013-0384-8
Hu S, Chen H, Ma J, Chen Q, Deng H, Gong F, Huang H, Shi C (2013) CpG7909 adjuvant enhanced immunogenicity efficacy in mice immunized with ESAT6-Ag85A fusion protein, but does not confer significant protection against Mycobacterium tuberculosis infection. J Appl Microbiol 115(5):1203–1211. doi:10.1111/jam.12315
Jiang X, Yu M, Qiao X, Liu M, Tang L, Jiang Y, Cui W, Li Y (2014) Up-regulation of MDP and tuftsin gene expression in Th1 and Th17 cells as an adjuvant for an oral Lactobacillus casei vaccine against anti-transmissible gastroenteritis virus. Appl Microbiol Biotechnol. doi:10.1007/s00253-014-5893-2
Kotton CN, Hohmann EL (2004) Enteric pathogens as vaccine vectors for foreign antigen delivery. Infect Immun 72(10):5535–5547. doi:10.1128/IAI. 72.10.5535-5547.2004
Liu D, Wang X, Ge J, Liu S, Li Y (2011) Comparison of the immune responses induced by oral immunization of mice with Lactobacillus casei-expressing porcine parvovirus VP2 and VP2 fused to Escherichia coli heat-labile enterotoxin B subunit protein. Comp Immunol Microbiol Infect Dis 34(1):73–81. doi:10.1016/j.cimid.2010.02.004
Liu W, Yuan C, Bao J, Guan W, Zhao Z, Li X, Tang J, Li D, Shi D (2014a) Generation of an attenuated strain oral vaccine candidate using a novel double selection platform in Escherichia coli. Appl Microbiol Biotechnol. doi:10.1007/s00253-014-6099-3
Liu W, Yuan C, Meng X, Du Y, Gao R, Tang J, Shi D (2014b) Frequency of virulence factors in Escherichia coli isolated from suckling pigs with diarrhoea in China. Vet J 199(2):286–289. doi:10.1016/j.tvjl.2013.11.019
Lourdault K, Wang LC, Vieira A, Matsunaga J, Melo R, Lewis MS, Haake DA, Gomes-Solecki M (2014) Oral immunization with Escherichia coli expressing a lipidated form of LigA protects hamsters against challenge with Leptospira interrogans serovar Copenhageni. Infect Immun 82(2):893–902. doi:10.1128/IAI. 01533-13
Morris JA, Thorns C, Scott AC, Sojka WJ, Wells GA (1982) Adhesion in vitro and in vivo associated with an adhesive antigen (F41) produced by a K99 mutant of the reference strain Escherichia coli B41. Infect Immun 36(3):1146–1153
Morris JA, Thorns CJ, Wells GA, Scott AC, Sojka WJ (1983) The production of F41 fimbriae by piglet strains of enterotoxigenic Escherichia coli that lack K88, K99 and 987P fimbriae. J Gen Microbiol 129(9):2753–2759
Norton EB, Lawson LB, Mahdi Z, Freytag LC, Clements JD (2012) The A subunit of Escherichia coli heat-labile enterotoxin functions as a mucosal adjuvant and promotes IgG2a, IgA, and Th17 responses to vaccine antigens. Infect Immun 80(7):2426–2435. doi:10.1128/IAI. 00181-12
Qiao X, Li G, Wang X, Li X, Liu M, Li Y (2009) Recombinant porcine rotavirus VP4 and VP4-LTB expressed in Lactobacillus casei induced mucosal and systemic antibody responses in mice. BMC Microbiol 9:249. doi:10.1186/1471-2180-9-249
Ruan X, Liu M, Casey TA, Zhang W (2011) A tripartite fusion, FaeG-FedF-LT(192)A2:B, of enterotoxigenic Escherichia coli (ETEC) elicits antibodies that neutralize cholera toxin, inhibit adherence of K88 (F4) and F18 fimbriae, and protect pigs against K88ac/heat-labile toxin infection. Clin Vaccine Immunol 18(10):1593–1599. doi:10.1128/CVI. 05120-11
You J, Xu Y, He M, McAllister TA, Thacker PA, Li X, Wang T, Jin L (2011) Protection of mice against enterotoxigenic E. coli by immunization with a polyvalent enterotoxin comprising a combination of LTB, STa, and STb. Appl Microbiol Biotechnol 89(6):1885–1893. doi:10.1007/s00253-010-2991-7
Zhao LL, Liu M, Ge JW, Qiao XY, Li YJ, Liu DQ (2012) Expression of infectious pancreatic necrosis virus (IPNV) VP2-VP3 fusion protein in Lactobacillus casei and immunogenicity in rainbow trouts. Vaccine 30(10):1823–1829. doi:10.1016/j.vaccine.2011.12.132
Acknowledgements
Financial support for this study was provided by grants from Synergetic Innovation Center of Food Safety and Nutrition, the National Science and Technology Support Project (2012BAD12B03-3, 2012BAD12B05-2), and the Science and Technology Planning Project of Heilongjiang Province (GC12B303). The authors thank Prof. Yijing Li for providing ZYM-DIEC02 cell lines.
Conflict of interest
None of the authors has any financial or personal relationships that could inappropriately influence or bias the content of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, W., Li, J., Bao, J. et al. Simultaneous oral immunization of mice with live attenuated Escherichia coli expressing LT192-STa13 and LT192-STb fusion immunogen, respectively, for polyvalent vaccine candidate. Appl Microbiol Biotechnol 99, 3981–3992 (2015). https://doi.org/10.1007/s00253-014-6302-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-014-6302-6