Abstract
In pediatric patients with acute refractory cardiogenic shock (CS), extracorporeal membrane oxygenation (ECMO) remains an established procedure to maintain adequate organ perfusion. In this context, ECMO can be used as a bridging procedure to recovery, VAD or transplantation. While being supported by ECMO, most centers tend to keep their patients well sedated and supported by invasive ventilation. This may be associated with an increased risk of therapy-related morbidity and mortality. In order to optimize clinical management in pediatric patients with ECMO therapy, we report our strategy of veno-arterial ECMO (VA-ECMO) in extubated awake and conscious patients. We therefore present data of six of our patients with CS, who were treated by ECMO being awake without continuous analgosedation and invasive ventilation. Of these six patients, four were <1 year and two >14 years of age. Median time on ECMO was 17.4 days (range 6.9–94.2 days). Median time extubated, while receiving ECMO support was 9.5 days. Mean time extubated was 78 % of the total time on ECMO. Three patients reached full recovery of cardiac function on “Awake-VA-ECMO,” whereas the other three were successfully bridged to destination therapy (VAD, heart transplantation, withdrawal). Four out of our six patients are still alive. Complications related to ECMO therapy (i.e., severe bleeding, site infection or dislocation of cannulas) were not observed. We conclude that “Awake-VA-ECMO” in extubated, spontaneously breathing conscious pediatric patients is feasible and safe for the treatment of acute CS and can be used as a “bridging therapy” to recovery, VAD implantation or transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extracorporeal membrane oxygenation (ECMO) has evolved into a standard-of-care procedure in pediatric patients with acute refractory cardiogenic shock [2, 8, 10, 15, 20]. Due to the outstanding evolution in the field of extracorporeal life support (ECLS) (i.e., technical devices, cannulation technique, specialized ECMO Teams), ECMO has developed to a familiar and safe tool in pediatric tertiary centers. Within this evolution, pediatric as well as adult patients can be maintained on ECMO for weeks or even month in order to bridge them to recovery, LVAD implantation or transplantation [6, 9, 11].
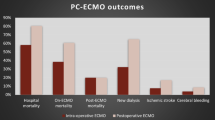
Although a myriad of new therapeutic approaches in the management of critical ill patients have been introduced in critical care medicine (e.g., small tidal volume ventilation, early initiation of renal replacement therapy, broad-spectrum antibiotics and antimycotics), the outcome of patients suffering from acute cardiogenic shock remains disproportionately poor (overall survival approximately 40 %), indicating the need to optimize their clinical management to achieve a more favorable outcome [3, 8, 23].
Although experiences regarding the concept of being awake and extubated on VA-ECMO as well as VV-ECMO have recently been published from our own adult ECMO patients (Hannover Group), there is still a lack of data in critically ill pediatric patients [5, 14, 17, 21]. We therefore previously described our first experiences in awake veno-venous ECMO (VV-ECMO) as a bridging concept to a further lung transplantation (LuTx) in pediatric patients, suggesting that patients being conscious and breathing spontaneously on ECMO prior to transplantation might have a better outcome compared to those who remained on the ventilator [16]. Anton-Martin et al. recently published their single-center data from sixteen patients being extubated for at least 24 h during their ECMO course. They were able to demonstrate that extubation and discontinuation of mechanical ventilation appear to be feasible in pediatric patients on long-term ECMO support without major complications [1].
Nevertheless, “Awake-VA-ECMO” in conscious extubated pediatric patients with acute cardiogenic shock has not been described so far.
In order to evaluate the feasibility and safety of “Awake-VA-ECMO” as a bridging strategy to recovery, diagnosis, VAD implantation or transplantation in pediatric patients, we have retrospectively reviewed our pediatric ECMO patients between 2009 and early 2015 at our institution and present the clinical data of six patients treated according to this “Awake-VA-ECMO-concept.”
Patients and Methods
Records of our pediatric patients supported on VA-ECMO due to acute cardiogenic shock at the Medical School Hannover, Germany, between 2009 and January 2015 were reviewed. The year 2009 was chosen as we started to introduce the concept of “Awake-ECMO” in our clinical practice. First starting with our pediatric patients on VV-ECMO awaiting lung transplantation, we transferred these experiences to our VA-ECMO patients.
In this retrospective analysis, a detailed review of each pediatric patient with acute cardiogenic shock who underwent “Awake-VA-ECMO” in the context of bridge to recovery, decision-making, transplantation or a further long-term device implantation was made. In each patient who met the inclusion criteria, demographic data, underlying disease, VA-ECMO device settings, clinical parameters, ECMO duration, extubation time on ECMO support, complications and interventions while on ECMO support and outcomes were collected (Table 1).
ECMO Devices and Settings
For extracorporeal life support (ECLS), a centrifugal pump (Deltastream DP 3, Medos, Medizintechnik AG, Germany, for patients < 1 year or the Maquet Rotaflow RF 32, MAQUET Cardiovascular, Fairfield, NJ, USA) was used in combination with a membrane oxygenator (Hilite 800 LT, Medos Medizintechnik AG, Germany, for patients < 1 year or the Quadrox PLS System, MAQUET Cardiovascular, Fairfield, NJ, USA). All patient-linked tubing systems were heparin-coated (Table 2).
Cannulas used on the arterial and venous side were selected according to the patient’s body size. Cannulation in all of our selected patients was performed peripherally by cut-down technique (neck cannulation in patients < 1 year) or percutaneously via Seldinger technique under sonographic control (groin cannulation in patients > 14 years). To guarantee sufficient perfusion of the cannulated leg, distal limb perfusion catheter was established under sonographic control using a 6- to 8-Fr sheath (Cordis Bridgewater). To allow physiotherapy while being awake on VA-ECMO in our older patients, both cannulas were implanted into one groin.
Anticoagulation was conducted with intravenous heparin in accordance with ELSO recommendations to maintain an activated clotting time goal of either 180–220 s (patients < 1 year) or 160–180 s (patients > 14 years). Antithrombin was substituted once antithrombin III level was subnormal (<70 %). To avoid bleeding complications, an initial threshold for platelet count >100,000 cells/mm3 was defined.
In all patients, pump flow was regulated to achieve adequate circulatory support and was monitored on the basis of systemic perfusion, oxygenation and mixed venous saturation (Table 3). Once clinical stabilization was achieved, inotropic pharmacological support was weaned as tolerated. Blood gas analyses were performed routinely from the right radial artery and from the ECMO oxygenator to ensure sufficient oxygen supply and carbon dioxide gas exchange.
In our two older patients with peripheral cannulation of the groin and distal leg perfusion, we continuously used near-infrared spectroscopy (NIRS) using the INVOS™, 5100 C, Covidien, Mansfield, USA, to monitor sufficient distal perfusion. In both patients, tissue oxygen saturation was >60 % without signs of ischemia or compartment [12].
Routine echocardiography was used to evaluate ventricular function and to assess filling of the ventricles as a measure of load removal in order to achieve ventricular recovery. In persistent ventricular compression, interventional cardiac catheterization was performed under VA-ECMO therapy (Table 4).
“AWAKE-ECMO” Setting, Cannula Fixation, Physiotherapy
Starting 2009, we introduced a special ECMO team (including pediatric intensivist, PICU/NICU nurse, physiotherapist and respiratory therapist) to evaluate our patients being on ECMO whether they are feasible “Awake-ECMO-Candidates.” Two indispensible presuppositions had to be fulfilled to stop sedation and consider extubation:
-
1.
A stable cardiopulmonary situation under ECMO support including sufficient oxygenation (SVO2 > 60–65 % and SAO2 > 95 %) with negative lactate, acceptable ventilator settings (e.g., PiP < 20 cm H2O, Peep < 6 cm H2O, FiO2 < 0.5 in patients < 1 year and PiP < 25 cm H2O, Peep < 8 cm H2O, FiO2 < 0.5 in our older patients) and chest X-ray without signs of major congestion.
-
2.
Due to the life-threatening complication of cannula dislocation (especially in conscious ECMO patients), we optimized our cannula fixation (Figs. 1, 2). Therefore, only in patients in whom cannula fixation was felt to be safe (sonographic and X-ray control of the cannula position) and no further interventions on the cannula site were planed (e.g., surgical re-fixation, surgical interventions due to bleeding reasons), sedation was reduced and patients were allowed to wake up and to be extubated.
Fig. 1 Exemplary VA-ECMO cannula fixation in our adolescent patient with cannulation of the left groin. 1 All cannulas are fixed surgically with sutures at the entrance site while continuous inspection of the cannula entrance area is possible using a Chlorhexidine drape (Tegaderm™ CHG, 3M Health Care, Germany); 2 Distal perfusion bypass, fixed with sutures; 3 Additional sutures fixating the arterial cannula distally from the entrance site; 4 Main-Lock fixation plaster (German Medical Products GmbH, Germany) fixating the arterial and venous cannula; 5 Additional fixation plate for venous cannula distal from the entrance site
Fig. 2 Exemplary VA-ECMO cannula fixation in our infant patients with neck cannulation. 1 Surgical sutures at the entrance site; 2 Main-Lock adhesive bandage/plaster (German Medical Products GmbH&Co.KG); 3 Endotracheal tube holder bandage or Elastomull® Cohesive Elastic fixation bandage (see Figs. 3, 4); 4 Chlorhexidine Dressing (Tegaderm™, 3M Health Care)
Caregivers were informed, and upcoming questions were answered. Within given permission, sedation was reduced and patients were extubated.
Although sedation was initially stopped/reduced for waking up our intubated patients, we used second-line agents (i.e., clonidine, lorazepam, phenobarbital, chloral hydrate) to allow a better patient comfort on ECMO if necessary. Therefore, once extubated, continuous infusion of clonidine (0.5–1.5 mic/kg/h) and intermittent administration of either phenobarbital or chloral hydrate (patients <1 year) or clonidine and lorazepam (>14 years) were allowed (Table 4). Unfortunately, comfort behavioral (comfort B) and Richmond Agitation–Sedation Scale (RASS) are not available in our retrospective analysis.
While being awake and extubated on VA-ECMO, all patients were included in daily active and passive physiotherapy programs to maintain muscular conditions. Parents were involved in clinical routine and therefore able to care for their children (e.g., feeding, washing, snuggling).
Patients Case Series
Case 1
This patient is a 2.5-month-old boy (Table 1) with severe signs of cardiac failure. Two weeks before, he showed signs of a viral infection. On admission, echocardiography showed a severe impaired left ventricular function [left ventricular end-diastolic diameter (LVEDD) 4.1 cm; fractional shortening (FS) 14 %] (Table 3). Despite inotropic support, the patient’s conditions worsened and VA-ECMO was started with the aim to bridge him to recovery under suspicion of viral myocarditis. He was intubated and underwent standard neck cannulation. Once on ECMO, our standardized ECMO protocol (see above) was applied regarding pump flow, anticoagulation and inotropic support including daily echocardiography in order to achieve ventricular recovery. In case of persistent left ventricular distension, cardiac catheterization with atrioseptostomy was performed without any complications (Table 4). Cardiac muscle biopsy showed signs of virus-associated myocarditis (cytomegalovirus). Twenty-four hours after cardiac catheterization, he could be extubated. During the following weeks, he remained extubated and was fully conscious (Fig. 3) while his parents were involved in clinical routine. No other organ system (kidney, liver, heart) showed signs of impaired function. On day 34 on ECMO, he developed signs of minor cerebral infarction, which caused reversible palsy of the right arm. While being fully awake, he could take part on immediately initiated physiotherapy programs and totally recovered from this minor cerebral infarction. He was listed for high-urgency heart transplantation. After 42 days (1007 h) on VA-ECMO support, a suitable donor organ became available, and he underwent successful heart transplantation. Forty-eight months following transplant, he is alive and doing well without any neurological problems (Table 4).
Case 2
This 5.5-month-old boy (Table 1), previously well, clinically presented with a life-threatening episode. Clinical evaluation showed dilatative cardiomyopathy of unknown origin with LVEDD = 5.1 cm and reduced FS of 13 % (Table 3). After 5 weeks of conventional anticongestive treatment (including inotropic support, milrinone, diuretics, ACE inhibitors), he developed signs of cardiac decompensation (Table 3). VA-ECMO was initiated and performed in accordance with our ECMO guidelines (see above). While on ECMO, echocardiography showed persistent left ventricular congestion. Therefore, cardiac catheterization was performed with atrial septostomy leading to ventricular decompression (Table 3). Biopsy demonstrated signs of inflammation without proven pathogen. Forty-eight hours after catheterization, and 5.5 days after cannulation, the patient was extubated. From then on, his parents were involved in clinical routine and were able to care for their son (e.g., feeding, washing, snuggling). While awake, the patient suffered from one episode of cannula dislocation requiring surgical intervention under local anesthesia. No severe bleeding events occurred under long-term ECMO run. However, this patient also developed a minor cerebral infarction with intermittent incomplete palsy of the right arm that recovered fully within one month. During the following weeks, the patient did not show any sign of recovery of his cardiac function and was therefore switched to permanent LVAD (Jarvik Heart, Inc, New York, NY) after 94 days on ECMO. Unfortunately, he died on day 18 after LVAD implantation (Table 1).
Case 3
This patient is an 18-year-old boy (Table 1) with congenital heart defect (corrected tetralogy of Fallot) who was admitted to PICU for acute cardiac shock secondary to severe sepsis caused by enterococcal endocarditis of his Contegra pulmonary-valved conduit (Table 3). Therefore, VA-ECMO was established via percutaneous femoral cannulation and performed in accordance with our ECMO guidelines (see above). Broad-spectrum antibiotics were started within 1 h of admission and were adapted to blood culture results. Twelve hours after cannulation, sedation was stopped, and he was extubated after 48 h on ECMO. He was fully awake and involved in clinical routine, including respiratory training and physiotherapy. Echocardiography revealed significant stenosis of the infected pulmonary conduit, preventing ventricular recovery. After right heart catheter with stent implantation into the right ventricular outflow tract, right ventricular function slowly recovered, and the patient could successfully be weaned from ECMO after a total of 20.5 days.
Case 4
This patient is a 4-week-old male (Table 1) with critical aortic stenosis and associated cardiac decompensation. He was admitted to our ward for interventional heart catheter. During catheterization, he developed refractory cardiogenic shock requiring VA-ECMO via cervical cannulation. Then on, ECMO was performed in accordance with our ECMO guidelines (see above). Due to prolonged resuscitation, the patient was cooled for 24 h. Forty-eight hours after cannulation, sedation was stopped, and on day 4 on ECMO, the boy was extubated without showing any sign of neurological impairment (Table 3). Apart from mild bleeding from the arterial cannula, successfully treated by mild compression, the patient did not suffer from any complication while on ECMO (Fig. 4). After 7 days, cardiac function has recovered, and he could successfully be weaned from ECMO.
Patient No. 2, 96 h after initiation of VA-ECMO. He is awake, breathing spontaneously receiving little airway support via nasal cannula. Cannula fixation was performed surgically at the entrance site as well as with steril drape and cohestive elastic fixation bandage (Elastomull®). 1 Cannulas are fixed surgically with sutures at the entrance site; in this case, a steril drape is used above the entrance site because the Chlorhexidine drape (Tegaderm™ CHG, 3M Health Care, Germany) can only be used in patients >2 month of age; 2 cohestive elastic fixation bandage (Elastomull®) around the head
Case 5
This patient is a 16-year-old boy (Table 1) with congenital heart defect (corrected tetralogy of Fallot in the first year of life). He was admitted to PICU with clinical signs of systemic infection (no pathogen could be isolated) and progressive cardiac failure. Initial echocardiography showed severe impaired biventricular function as wells as secondary pulmonary hypertension. Additionally, echocardiography showed a previously unknown relevant stenosis of the pulmonary trunk and the left pulmonary artery (Table 3). Although the patient was started immediately on inotropes and broad-spectrum antibiotics, his clinical situation deteriorated rapidly developing sings of acute cardiac failure (arrhythmias, rising lactate, decreased level of consciousness) (Table 3). While the patient was intubated, bedside femoral cannulation for VA-ECMO was performed and ECMO was commenced in accordance with our ECMO guidelines (see above). However, cardiac function did not recover despite full decompression of both ventricles, most likely because of persistent right outflow tract stenosis. We therefore decided to perform right heart catheterization with stent implantation into the pulmonary trunk and the left pulmonary artery. Following right heart catheterization, his cardiac function slowly recovered. Twenty-four hours after catheter intervention, sedation was stopped and he was extubated after 7 days on ECMO. From then on, he was fully awake, took part in daily physiotherapy programs as well as in respiratory care and daily bedside school lessons. After a total of 11.5 days, he was successfully weaned from ECMO.
Case 6
This 2-day old female term newborn was admitted to our ward with severe signs of acute cardiac failure. On admission, her echocardiography showed normal heart anatomy with severe impaired biventricular function (fractional shortening (FS) 12 %) and signs of persistent pulmonary hypertension (Table 3). Despite inotropic support, the patient’s conditions worsened and VA-ECMO was started as a bridge to decision-making. She was intubated and underwent standard neck cannulation. Once on ECMO, our standardized ECMO protocol (see above) was applied. Due to persistent left ventricular overfilling, Rashkind’s procedure was performed without any complications (Table 4) while cardiac muscle biopsy showed signs of cardiomyopathy. She was successfully extubated after 8 days on VA-ECMO support. During the following days, she remained extubated while her parents were involved in clinical routine. Within the diagnosis of neonatal cardiomyopathy, heart transplantation was offered and was refused by her parents. Therapy was withdrawn and she deceased in the arms of her parents.
Discussion
Within the ongoing advances in the field of ECLS, long-term ECMO use in acute cardiogenic shock is now safe and feasible. Nevertheless, the outcome of patients suffering from acute cardiac failure remains disproportionately poor [4, 8]. The concept of being awake on ECMO might avoid complications associated with mechanical ventilation, long-term sedation and immobilization and therefore help to accelerate recovery and achieve a favorable outcome in this critically ill patient group. Recently published data have shown that this strategy can be used as a bridge to recovery or transplantation concept in adult patients suffering from acute cardiopulmonary failure [13, 17, 21]. Even so, Anton-Martin et al. [1] demonstrated in their single-center experience that extubation during pediatric ECMO is feasible in VV and VA ECMO, and there is still a lack of data regarding the use of an “Awake-VA-ECMO-concept” in pediatric patients.
One of the reasons why concepts of “Awake-ECMO” have not yet been applied in pediatric patients so far might be the concern of potentially life-threatening complications (i.e., cannula dislocation, site bleedings or even accidental decannulation). Sedation and sedation-associated mechanical ventilation have therefore been seen as an essential part in this patient group [10]. However, in recent years, it has become more and more evident that sedation and sedation-associated problems—such as tolerance, physical dependency and withdrawal—are themselves complicating and prolonging clinical recovery, especially in patients suffering from circulatory failure. One of the hallmarks of intensive care in the past has therefore been the aim to reduce sedation and ventilation times as much as possible [18, 19]. Despite a plenty of data in adult patients, controlled trials in the pediatric population are lacking. Gupta et al. recently demonstrated in PICU patients that length of mechanical ventilation, length of stay in the PICU and the average calculated cost of therapy were significantly reduced in the group of patients receiving interrupted sedation compared to the group receiving continuous sedation [7]. While transferring the concept of daily interruption of sedation in critically ill pediatric patients on ECMO, Wildschut et al. [22] were the first to show that sedation interruption is feasible and safe in neonates on ECMO without increased risks of complications. Compared to Wildschut et al., we even went further extubating our VA-ECMO patients, once clinical stabilization has been achieved and presuppositions had been fulfilled (see above). Within the data from our adult ECMO patients demonstrating that the concept of “Awake-ECMO” is feasible for patients on VV-ECMO as well as on VA-ECMO as a bridge to recovery or transplantation concept without major complications [5, 14, 17], we transferred these valuable experiences to our pediatric VA-ECMO patients.
Here we present data of six of our pediatric patients suffering from acute, potentially reversible cardiogenic shock, who were supported on VA-ECMO while being conscious and spontaneously breathing. Three patients were suffering from Myocarditis/DCM, one patient presented with acute left ventricular failure associated with ballon valvuloplasty for critical aortic stenosis, and two patients had acute right ventricular failure associated with pulmonary valve endocarditis. In these patients, cannulation was performed via peripheral vascular access. Regarding the subgroup of patients, which will be cannulated centrally via thoracotomy [e.g., post-cardiotomy or under extracorporeal cardiopulmonary resuscitation (ECPR)], we decided to exclude them, because they were felt to be at a higher risk of site bleeding and cannula dislocation compared to our peripherally cannulated patients. Nevertheless, in adolescent post-cardiotomy patients in whom longer period of ECMO support is required, we would try to switch to a peripheral cannulation once the patient is hemodynamically stable and without major bleeding. If peripheral cannulated, we would not hesitate to further pursue on our “Awake-ECMO-concept.”
In our case series, no life-threatening ECMO-related complications occurred. Similar to other ECMO studies, the complications we observed were related to cannula site bleeding [13]. In accordance with these reports, our therapeutic concept to allow full consciousness and spontaneous breathing on ECMO in critically ill children did not lead to more frequent or more severe complications. Only one patient required surgical intervention on the cannulation site, which could be performed in local anesthesia. Bleeding complications were neither more frequent nor more severe compared to previous times when patients were fully sedated. Only one life-threatening complication occurred in the patient who was switched from conventional ECMO to LVAD and was LVAD-associated (hemolysis and system failure).
Although distal limb perfusion was routinely measured with NIRS, additional verbal pain assessment in our two adolescents helps to confirm that there were no problems regarding leg perfusion. Being awake on ECMO therefore might not only help to reduce complications associated with mechanical ventilation, sedation and immobilization but also help to assess complications much earlier throughout communication to their caregivers helping to perform safer and longer ECMO runs before switching to long-term LVAD. In addition, “Awake-VA-ECMO” allows the patient to participate in daily activities and physiotherapy, potentially improves their general physical condition and prevents long periods of withdrawal, thus shortening rehabilitation times once ECMO therapy can be stopped.
Mechanical cardiopulmonary support promotes clinical stabilization within minutes after ECMO cannulation in acute cardiogenic shock. To provide adequate further therapy, it is vital to identify patients with irreversible neurological injury. Therefore, neurological assessment on ECMO is essential. Although ultrasound cerebral scans, cranial computed tomography as well as electroencephalograms could be performed, a conclusive predication often is impossible. Within waking up our patients on ECMO, early and detailed examination of neurological behavior is possible and might help to decide whether withdrawal of support due to irreversible neurological injury is necessary. Especially in patient 4 in whom ECMO was started in context to reanimation, we had been able to assess adequate neurological status 72 h after starting ECMO allowing us to continue extracorporeal support.
Limitations
The number of pediatric patients from this single-center report is too small to allow any major conclusions, and analysis was performed retrospectively without any comparable control group. It also has to be kept in mind that results will be greatly influenced by the individual hospital policies itself, so pediatric Awake-VA-ECMO might not be feasible for every tertiary hospital and ECMO center.
Conclusion
VA-ECMO in extubated, fully conscious and spontaneously breathing pediatric patients could be an appropriate therapeutic approach even for children with cardiogenic shock requiring mechanical support for longer periods of time. This strategy might help to reduce long-term sedation and immobilization while assessing neurologic status of each patient more precisely. We demonstrated that the concept of “Awake-VA-ECMO” is feasible and safe in pediatric patients presenting with acute cardiogenic shock.
References
Anton-Martin P, Thompson MT, Sheeran PD, Fischer AC, Taylor D, Thomas JA (2014) Extubation during pediatric extracorporeal membrane oxygenation: a single-center experience. Pediatr Critic Care Med 15(9):861–869. doi:10.1097/PCC.0000000000000235
Cooper DS, Jacobs JP, Moore L et al (2007) Cardiac extracorporeal life support: state of the art in 2007. Cardiol Young 17(S2). doi:10.1017/S1047951107001217
Dalton HJ (2011) Extracorporeal life support: moving at the speed of light. Respir Care 56(9):1445–1453 (discussion 1453–1456). doi:10.4187/respcare.01369
Extracorporeal Life Support Organization, Ann Arbor, MI. ECLS Registry Report, International Summary, January 2015. www.elso.org/Registry/Statistics/InternationalSummary.aspx
Fuehner T, Kuehn C, Hadem J et al (2012) Extracorporeal membrane oxygenation in awake patients as bridge to lung transplantation. Am J Respir Crit Care Med 185(7):763–768. doi:10.1164/rccm.201109-1599OC
Gupta P, McDonald R, Chipman CW et al (2012) 20-year experience of prolonged extracorporeal membrane oxygenation in critically ill children with cardiac or pulmonary failure. Ann Thorac Surg 93(5):1584–1590. doi:10.1016/j.athoracsur.2012.01.008
Gupta K, Gupta VK, Jayashree M, Muralindharan J, Singhi S (2012) Randomized controlled trial of interrupted versus continuous sedative infusions in ventilated children. Pediatr Crit Care Med 13(2):131–135. doi:10.1097/PCC.0b013e31820aba48
Joffe AR, Lequier L, Robertson CMT (2012) Pediatric outcomes after extracorporeal membrane oxygenation for cardiac disease and for cardiac arrest. ASAIO J 58(4):297–310. doi:10.1097/MAT.0b013e31825a21ff
Kirshbom PM, Bridges ND, Myung RJ, Gaynor JW, Clark BJ, Spray TL (2002) Use of extracorporeal membrane oxygenation in pediatric thoracic organ transplantation. J Thorac Cardiovasc Surg 123(1):130–136. doi:10.1067/mtc.2002.118504
Lequier L (2004) Extracorporeal life support in pediatric and neonatal critical care: a review. J Intensive Care Med 19(5):243–258. doi:10.1177/0885066604267650
Levi D, Marelli D, Plunkett M et al (2002) Use of assist devices and ECMO to bridge pediatric patients with cardiomyopathy to transplantation. J Heart Lung Transpl 21(7):760–770
Md RJS, Md SS, Md BA et al (2014) Using near-infrared spectroscopy to monitor lower extremities in patients on venoarterial extracorporeal membrane oxygenation. Ann Thorac Surg 98(5):1853–1854. doi:10.1016/j.athoracsur.2014.04.057
Mohite P, Sabashnikov A, Reed A et al (2015) Extracorporeal life support in “Awake” patients as a bridge to lung transplant. Thorac Cardiovasc Surg 1–7. doi:10.1055/s-0035-1546429
Olsson KM, Simon A, Strueber M et al (2010) Extracorporeal membrane oxygenation in nonintubated patients as bridge to lung transplantation. Am J Transpl 10(9):2173–2178. doi:10.1111/j.1600-6143.2010.03192.x
Rajagopal SK, Almond CS, Laussen PC, Rycus PT, Wypij D, Thiagarajan RR (2010) Extracorporeal membrane oxygenation for the support of infants, children, and young adults with acute myocarditis: a review of the Extracorporeal Life Support Organization registry*. Crit Care Med 38(2):382–387. doi:10.1097/CCM.0b013e3181bc8293
Schmidt F, Sasse M, Boehne M et al (2012) Concept of “awake venovenous extracorporeal membrane oxygenation” in pediatric patients awaiting lung transplantation. Pediatr Transpl 17(3):224–230. doi:10.1111/petr.12001
Sommer W, Marsch G, Kaufeld T et al (2015) Cardiac awake extracorporeal life support-bridge to decision? Artif Organs n/a–n/a. doi:10.1111/aor.12396
Strøm T, Toft P (2011) Time to wake up the patients in the ICU: a crazy idea or common sense? Minerva Anestesiol 77(1):59–63
Strøm T, Martinussen T, Toft P (2010) A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet 375(9713):475–480. doi:10.1016/S0140-6736(09)62072-9
Thourani VH, Kirshbom PM, Kanter KR et al (2006) Venoarterial extracorporeal membrane oxygenation (VA-ECMO) in pediatric cardiac support. Ann Thoracic Surg 82(1):138–145. doi:10.1016/j.athoracsur.2006.02.011
Tudorache I, Sommer W, Kühn C et al (2015) Lung transplantation for severe pulmonary hypertension—awake extracorporeal membrane oxygenation for postoperative left ventricular remodelling. Transplantation 99(2):451–458. doi:10.1097/TP.0000000000000348
Wildschut ED, Hanekamp MN, Vet NJ et al (2010) Feasibility of sedation and analgesia interruption following cannulation in neonates on extracorporeal membrane oxygenation. Intensive Care Med 36(9):1587–1591. doi:10.1007/s00134-010-1931-4
Wolf MJ, Kanter KR, Kirshbom PM, Kogon BE, Wagoner SF (2012) Extracorporeal cardiopulmonary resuscitation for pediatric cardiac patients. Ann Thorac Surg 94(3):874–879 (discussion 879–80). doi:10.1016/j.athoracsur.2012.04.040
Acknowledgments
We thank Sebastian Tiedge and Joerg Optenhoeffel for their technical ECMO support.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmidt, F., Jack, T., Sasse, M. et al. “Awake Veno-arterial Extracorporeal Membrane Oxygenation” in Pediatric Cardiogenic Shock: A Single-Center Experience. Pediatr Cardiol 36, 1647–1656 (2015). https://doi.org/10.1007/s00246-015-1211-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1211-8