Abstract
Background
Veno-arterial extracorporeal membrane oxygenation (VA-ECMO) can be initiated during cardiac surgery or later in ICU according to the hemodynamic profile and organ perfusion. Our aim was to study the appropriate timing of post-cardiotomy ECMO (PC-ECMO) initiation. We retrospectively analyzed 152 adult patients supported with PC-ECMO in our cardiac center between 2016 and 2022. The patients were divided into two groups: the intra-operative ECMO and the postoperative ECMO groups. The primary outcome was all-and-on-ECMO hospital mortality. The secondary outcomes included ECMO duration, new need for dialysis, cerebrovascular stroke, and length of ICU stay.
Results
Our cohort analysis revealed that 81(53.3%) patients were intra-operatively supported with VA-ECMO while 71(46.7%) patients were postoperatively supported in ICU. The postoperative ECMO group had significantly lesser SAVE score (p = 0.001), higher SAVE risk classes (p < 0.001), and higher SOFA score (p = 0.008) compared to the intra-operative ECMO group. The postoperative ECMO group had significantly more frequent hospital mortality (p = 0.003), on-ECMO mortality (p = 0.006), cerebrovascular stroke (p = 0.034), acute renal failure requiring dialysis (p < 0.001), and lesser lactate clearance at 12 h (p = 0.016) and at 24 h (p = 0.023) compared to the intra-operative group. There were statistically insignificant differences between the two groups regarding post-ECMO hospital mortality, cerebral bleeding, limb ischemia, ECMO, and ICU duration. Postponed postoperative ECMO insertion was associated with an increased risk of death (HR 1.628, 95%CI 1.102–2.403, p =0.014) with cox-proportional hazard regression. Logistic multivariable regression showed that atrial fibrillation (OR 6.2, 95% CI 2.71–61.84, p = 0.002), initial SOFA score (OR 1.46, 95% CI 1.041–3.83, p = 0.001), and postoperative ECMO insertion (OR 1.93, 95% CI 1.04–8.73, p = 0.031) were the predictors of hospital mortality.
Conclusions
Postponed ECMO insertion in critically sick patients was associated with increased mortality after cardiac surgery. Early intra-operative initiation of PC-ECMO may have the potential to improve outcomes after cardiac surgeries.
Similar content being viewed by others
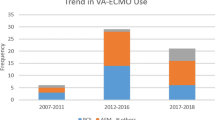
Background
The use of veno-arterial extracorporeal membrane oxygenation (VA-ECMO) with cardiac surgery is common but its application depends on the cardiac surgeons and each center ̕s policy and experience [1, 2]. Being an invasive procedure, resource-consuming, and associated with many morbidities, the decision to initiate post-cardiotomy VA-ECMO (PC-ECMO) is challenging to the surgeons to avoid unnecessary early mechanical support hoping that the clinical condition will improve by maximizing medical therapy [2,3,4,5]. To minimize the worse outcomes, ECMO should be initiated before the irreversible impaired tissue perfusion and multi-organ injury [6]. The complexity of patients undergoing cardiac surgery due to pre-operative risk profile, systematic effects of cardiopulmonary circulation, and operative complications makes the time to initiate VA-ECMO challenging. The decision to early start ECMO or wait longer with maximizing medical therapy is challenging with each patient developing post-cardiotomy shock. The objective of this study was to review all patients who underwent PC-ECMO in our center and whether the timing of ECMO (intra-operatively vs. postoperatively) affected the outcomes.
Methods
Study design and population
This was a retrospective single-center cohort study that enrolled all adult patients who were supported with VA-ECMO after cardiac surgery. The study was conducted in King Faisal Specialist Hospital and Research Center (KFSHRC) and was approved by the Institutional Review Board and given the reference number (2191042). All patients studied were ≥ 18 years old and received cardiac surgeries in KFSHRC and managed in the cardiac surgical intensive care unit between 2016 and 2022. We excluded all patients who had ECMO for non-surgical reasons and those who were referred on-ECMO from other centers.
ECMO initiation and scores
ECMO insertion was done by the cardiac surgeons in all patients either in the operation room or later in the ICU with refractory cardiogenic shock. We used the Survival after Veno-arterial ECMO (SAVE) and Sequential Organ Failure Assessment (SOFA) scores to evaluate our patients. The SAVE score was created in 2015 specifically to assess the patients before VA-ECMO initiation with a score range (– 35 to 17) and 5 risk classes [7]. The SAVE score consists of many variables (age and body weight of the patients, presence of renal, liver, and neurological dysfunctions, etiology of cardiogenic shock, peak inspiratory pressure, duration of invasive ventilation before ECMO, pre-ECMO arterial diastolic and pulse pressures, and occurrence of cardiac arrest). The SOFA score is a general score for critically ill patients and was tested in many patient groups including patients on VA-ECMO [8, 9]. The SOFA score consists of 6 variables (mean arterial blood pressure, serum bilirubin, platelet count, serum creatinine, PaO2/FiO2, Glasgow Coma Scale) and each one varies from – 4 to 4. It can be repeated every 48 h to assess organ function improvement or deterioration. We calculated SOFA score at 3 points; before ECMO initiation and then on the third and fifth days. The change of SOFA was calculated as the differences between the 3rd or 5th day and the initial score.
The studied variables and outcomes
The primary outcome was all-and-on-ECMO hospital mortality. The secondary outcomes included ECMO duration, a new need for dialysis, cerebrovascular stroke, and length of ICU stay. The pre-operative variables collected included age, diabetes mellitus, renal impairment, coronary and cerebrovascular diseases, underlying heart disease, and previous cardiotomy. The underlying heart diseases included ischemic cardiomyopathy due to coronary artery disease, adult congenital heart disease, rheumatic heart disease, and idiopathic dilated, restrictive, or hypertrophic cardiomyopathy. The operative variables included the type of surgery, cardiopulmonary bypass (CPB) time, aortic cross-clamping time, intra-aortic balloon pump (IABP) use. Most of the patients studied had isolated valves or combined valve and CABG surgeries. The laboratory variables included pre-operative hemoglobin, platelet count, serum creatinine, bilirubin, and liver enzymes. Blood lactate was measured at 4 points: at ECMO initiation (L0), 12 h (L12) and 24 (L24) h later and the peak value. Lactate clearance was calculated at 2 points: 12 and 24 h after ECMO initiation [10]:
Statistical analysis
Data were summarized as frequency (with percentage) for categorical data and median (with interquartile range Q1–Q3) in quantitative data due to skewed data distribution. The Mann-Whitney test was used for comparing quantitative variables. Chi-square (χ2) test was used for comparing categorical data. Two-sided p values ˂ 0.05 were considered significant. The Kaplan-Meier method was used to get the survival curves of the intra-operative and postoperative ECMO groups. The log-rank test was used for comparison between the survival curves. Cox-proportional hazard analysis and logistic multivariable regression were done for hospital mortality. The statistical package for the Social Sciences (SPSS) version 28 was used for statistical analysis (IBM Corp., Armonk, NY, USA).
Results
The pre-ECMO patients characteristics
After reviewing 195 VA-ECMO-supported adult patients, 152 adult post-cardiotomy patients supported with VA-ECMO were enrolled after the exclusion of non-cardiotomy patients. The intra-operative ECMO group included 81(53.3%) while the postoperative (ICU) ECMO group included 71(46.7%) patients. There were no significant differences between both groups regarding pre-operative demographic, clinical, operative or ECMO cannulation variables. The postoperative ECMO group had significantly lesser median SAVE score (p = 0.001), higher SAVE risk classes (p < 0.001), and higher median SOFA score (p = 0.008) compared to the intra-operative ECMO group (Table 1).
Laboratory data of the patients studied
The postoperative ECMO group had significantly higher blood lactate levels at ECMO initiation(p = 0.04), 12 h later (p=0.032), and 24 h later(p = 0.041) with lesser lactate clearance at 12 h (p = 0.016) and 24 h (p = 0.023) after ECMO support compared to the intra-operative ECMO group. The postoperative ECMO group had significantly lesser median hemoglobin level (p < 0.001), platelet count (p = 0.01), and GFR (p = 0.004) compared to the intra-operative ECMO group (Table 2).
Outcomes of the patients studied
The postoperative ECMO group had significantly higher hospital mortality (p = 0.003), on-ECMO mortality (p = 0.006), cerebrovascular stroke (p = 0.034), and acute renal failure requiring dialysis (p < 0.001) compared to the intra-operative group. There were statistically insignificant differences between the two groups regarding post-ECMO hospital mortality, cerebral bleeding, limb ischemia, ECMO duration, and ICU stay (Table 3, Fig. 1).
Cox-proportional hazard analysis showed that postponed postoperative ECMO insertion was associated with an increased risk of death (HR 1.628, 95% CI 1.102–2.403, p =0.014). Univariable analysis of mortality and logistic multivariable regression showed that atrial fibrillation (OR 6.2, 95% CI 2.71–61.84, p = 0.002), initial SOFA score (OR 1.46, 95%CI 1.041–3.83, p = 0.001), and postoperative insertion (OR 1.93, 95% CI 1.04–8.73, p = 0.031) were the predictors of hospital mortality (Tables 4 and 5).
The logistic regression model had a goodness-of-fit by Hosmer-Lemeshow test (Pearson chi2 = 26.81, p value = 1) and the mean variance inflation factor (VIF) was 1.13. The univariate analysis showed significant differences between the study survivors and non-survivors regarding CKD, previous cardiotomy SAVE score, and cardiopulmonary bypass time. However, these variables were not independent predictors of mortality in the logistic multivariable regression. Lactate clearance was not included in the logistic model due to multicollinearity with postoperative ECMO variable as evidenced by high VIF. Kaplan-Meier curves showed a decreased survival with postoperative ECMO initiation compared to intra-operative ECMO with log-rank p = 0.012 (Fig. 2).
Discussion
The main finding of this observational study was that early intra-operative initiation of PC-ECMO was associated with decreased hospital mortality after cardiac surgeries. The postoperative ECMO group had significantly higher hospital mortality (p = 0.003), on-ECMO mortality (p = 0.006), acute cerebrovascular stroke (p = 0.034), and acute renal failure requiring dialysis (p < 0.001) compared to the intra-operative group.
PC-ECMO is required for refractory post-cardiotomy cardiogenic shock (PCS) that occurs in about 0.3–3.6% of total cardiotomies according to the different reports due to variations in study populations, surgery types and complications, cardiac centers experiences, and policies [2, 3, 6]. Our cohort analysis revealed that the total hospital mortality was 68.4% and of them 74 (48.7%) patients died on ECMO. Our results were similar to the reports from large multicenter studies of PC-ECMO [11,12,13]. Mariani et al. studied 2003 patients with PC-ECMO from 34 centers and reported 60% mortality [11]. Biancari et al. studied 781 patients with PE-ECMO from 19 centers and reported a total mortality of 64.4% and subgroup analysis showed a mortality of 76.1% in patients aged > 70 years [12]. Biancari et al. [13] studied 1269 patients with PC-ECMO and reported hospital mortality of 70.7% (vs. 63.7%) in the central and peripheral cannulation groups respectively. There were no significant differences in the cannulation approaches in our cohort analysis. Most mortality reports described the variables associated with mortality but there is little data about the importance of timing of PC-ECMO.
In our cohort, we found that postoperative ECMO insertion was associated with a 22% higher hospital mortality compared to the intra-operative ECMO insertion and the patients of both groups did not have significant differences regarding the pre-operative clinical variables or the surgical details. Moreover, postoperative ECMO was associated with an increased hazard ratio in the Cox-proportional regression and was an independent predictor of mortality in the logistic multivariable regression. Mariani et al. reported that the post-operative ECMO group had a 7% higher mortality despite having lesser pre-operative and intra-operative risk profiles [11].
We found that the pre-ECMO laboratory variables were statistically worse in the postoperative ECMO group including anemia, thrombocytopenia, and lactic acidosis. Ideally, ECMO should be considered before anaerobic metabolism (indicated with hyperlactatemia) and multi-organ injury [6]. Hyperlactatemia was linked to different worse outcomes during VA-ECMO support with different cut-off values for differentiating hospital mortality [14, 15]. The postoperative ECMO insertion was associated with significant hyperlactatemia at ECMO initiation and delayed clearance at the 12th and 24th hours. Lactate clearance was a strong independent predictor of hospital mortality in patients with cardiogenic shock [10].
Mariani et al. [11] reported that 22.8% of patients with postoperative ECMO had cardiac arrest compared to 11.2% in the intra-operative ECMO group which may be due to long waiting to take a decision for ECMO initiation. In our relatively small cohort, we did not have a large number of cardiac arrests and ECPR. Hemodynamic deterioration despite maximizing medical therapy requires an early consideration of mechanical circulatory support before developing cardiac arrest [16, 17].
Regarding the cerebral and renal outcomes, the postoperative ECMO group had significantly higher frequencies of acute cerebrovascular strokes, acute kidney injury, and new need for dialysis compared to the intra-operative ECMO group. Mariani et al. [11] reported a significant increase in multi-organ failure in the postoperative ECMO group. We used the SOFA and SAVE scores for the risk assessment of the patients studied. The postoperative ECMO group had a higher initial SOFA score and an increased trend over the next few days indicating the clinical severity and occurrence of multiorgan affection compared to the intra-operative ECMO group. The increased trend of SOFA score in the postoperative group together with the delayed lactate clearance indicates the delayed ECMO support and occurrence of multi-organ injury. Increased SOFA trend was linked to mortality in patients with VA-ECMO [4, 9]. Initial SOFA score was an independent predictor of hospital mortality with PC-ECMO in our cohort analysis. Atrial fibrillation was an independent predictor of mortality with PC-ECMO in our cohort. This finding is consistent with Saxena et al. [18] who reported the association between pre-operative atrial fibrillation and hospital mortality with PC-ECMO [18]. Mariani et al. [19] recently analyzed 2058 patients with PC-ECMO from 34 centers and reported that atrial fibrillation was an independent predictor of mortality during follow-up.
The postoperative ECMO group had a significantly lower median SAVE score with increased frequencies of the higher-risk classes. The SAVE score was initiated for predicting survival with VA-ECMO with a good discrimination but its validity for PC-ECMO is still controversial [7]. Despite the non-survivors having significantly lower SAVE scores compared to the survivors in our study, it was an insignificant predictor in the logistic multivariable regression.
The surgeons usually initiate the intra-operative ECMO for patients with high pre-operative risk and with failed weaning off cardiopulmonary bypass. The patients with pre-operative low-risk profiles and borderline hemodynamics, the surgeons usually postpone ECMO insertion hoping that the patients will improve with medical therapy and avoid the risks of ECMO. However, this may result in deterioration of hemodynamics, multi-organ injury, and increased risks of cardiac arrest, morbidities, and hospital mortality.
Conclusions
Postponed ECMO insertion in critically sick patients was associated with increased mortality after cardiac surgery. Early intra-operative initiation of PC-ECMO may have the potential to improve outcomes after cardiac surgeries.
Limitations
The study is a single-center experience with a retrospective observational analysis. We could not get detailed data about the hemodynamic profile and vasopressors during and postoperatively to calculate the vasopressor score. However, we calculated the SAVE and SOFA scores to assess the clinical severity of the patients studied. We could not get the criteria of ECMO weaning especially the aortic velocity time integral (VTI) and lateral mitral annulus peak systolic velocity (TDSa).
Availability of data and materials
The data of the study is available with the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- CABG:
-
Coronary artery bypass graft
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CRRT:
-
Continuous renal replacement therapy
- ECMO:
-
Extracorporeal membrane oxygenation
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- GFR:
-
Glomerular filtration rate
- OR:
-
Odds ratio
- IABP:
-
Intra-aortic balloon pump
- SAVE:
-
Survival after veno-arterial ECMO
- SOFA:
-
Sequential organ failure assessment
- LC:
-
Lactate clearance
- LVAD:
-
Left ventricular assist device
References
Kowalewski M, Raffa GM, Zielinski K, Alanazi M, Gilbers M, Heuts S et al (2020) The impact of Centre’s heart transplant status and volume on in-hospital outcomes following extracorporeal membrane oxygenation for refractory postcardiotomy cardiogenic shock: a meta-analysis. BMC Cardiovasc Disord 20:10
Kowalewski M, Zielinski K, Brodie D, MacLaren G, Whitman G, Raffa GM et al (2021) Venoarterial extracorporeal membrane oxygenation for postcardiotomy shock-analysis of the extracorporeal life support organization registry. Crit Care Med 49:1107–1117
Lorusso R, Raffa GM, Alenizy K, Sluijpers N, Makhoul M, Brodie D et al (2019) Structured review of post-cardiotomy extracorporeal membrane oxygenation: part 1— adult patients. J Heart Lung Transplant 38:1125–1143
Laimoud M, Alanazi M, Qureshi R (2021) Hospital outcomes after emergent peripheral veno-arterial extracorporeal membrane oxygenation in adult patients presenting with cardiogenic shock. Signa Vitae 17(5):103–109
Rao P, Khalpey Z, Smith R, Burkhoff D, Kociol RD (2018) Venoarterial extracorporeal membrane oxygenation for cardiogenic shock and cardiac arrest: cardinal considerations for initiation and management. Circulation. Heart Failure 11(9):e004905
Lorusso R, Whitman G, Milojevic M, Raffa G, McMullan DM, Boeken U et al (2021) 2020 EACTS/ELSO/STS/AATS expert consensus on post-cardiotomy extracorporeal life support in adult patients. J Thorac Cardiovasc Surg 161:1287–1331
Schmidt M, Burrell A, Roberts L et al (2015) Predicting survival after ECMO for refractory cardiogenic shock: the survival after veno-arterial-ECMO (SAVE)-score. Eur Heart J 36:2246–2256
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. Jama 286(14):1754–1758
Laimoud M, Alanazi M (2020) The validity of SOFA score to predict mortality in adult patients with cardiogenic shock on venoarterial extracorporeal membrane oxygenation. Crit Care Res Pract 2020:3129864
Marbach JA, Di Santo P, Kapur NK, Thayer KL, Simard T, Jung RG, Parlow S, Abdel-Razek O, Fernando SM, Labinaz M, Froeschl M (2022) Lactate clearance as a surrogate for mortality in cardiogenic shock: insights from the DOREMI trial. J Am Heart Assoc 11(6):e023322
Mariani S, Wang IW, van Bussel BC, Heuts S, Wiedemann D, Saeed D, van der Horst IC, Pozzi M, Loforte A, Boeken U, Samalavicius R (2023) The importance of timing in postcardiotomy venoarterial extracorporeal membrane oxygenation: A descriptive multicenter observational study. J Thorac Cardiovasc Surg 166
Biancari F, Dalén M, Fiore A, Ruggieri VG, Saeed D, Jónsson K, Gatti G, Zipfel S, Perrotti A, Bounader K, Loforte A (2020) Multicenter study on postcardiotomy venoarterial extracorporeal membrane oxygenation. J Thorac Cardiovasc Surg 159(5):1844–1854
Biancari F, Kaserer A, Perrotti A, Ruggieri VG, Cho SM, Kang JK, Dalén M, Welp H, Jónsson K, Ragnarsson S, Hernández Pérez FJ (2022) Central versus peripheral postcardiotomy veno-arterial extracorporeal membrane oxygenation: systematic review and individual patient data meta-analysis. J Clin Med 11(24):7406
Laimoud M, Alanazi M (2020) The clinical significance of blood lactate levels in evaluation of adult patients with veno-arterial extracorporeal membrane oxygenation. Egypt Heart J 72(1):74. https://doi.org/10.1186/s43044-020-00108-7. (PMID: 33108534; PMCID: PMC7588953)
Biancari F, Kaserer A, Perrotti A, Ruggieri VG, Cho SM, Kang JK, Dalén M, Welp H, Jónsson K, Ragnarsson S, Hernández Pérez FJ (2023) Hyperlactatemia and poor outcome after postcardiotomy veno-arterial extracorporeal membrane oxygenation: an individual patient data meta-analysis. Perfusion 02676591231170978
Naidu SS, Baran DA, Jentzer JC, Hollenberg SM, van Diepen S, Basir MB et al (2022) SCAI SHOCK stage classification expert consensus update: a review and incorporation of validation studies: this statement was endorsed by the American College of Cardiology (ACC), American College of Emergency Physicians (ACEP), American Heart Association (AHA), European Society of Cardiology (ESC) Association for Acute Cardiovascular Care (ACVC), International Society for Heart and Lung Transplantation (ISHLT), Society of Critical Care Medicine (SCCM), and Society of Thoracic Surgeons (STS) in December 2021. J Am Coll Cardiol 79:933–946
Masud F, Gheewala G, Giesecke M, Suarez EE, Ratnani I (2020) Cardiogenic shock in perioperative and intraoperative settings: a team approach. Methodist Debakey Cardiovasc J 16:e1–e7
Saxena P, Neal J, Joyce LD, Greason KL, Schaff HV, Guru P, Shi WY, Burkhart H, Li Z, Oliver WC, Pike RB, Haile DT, Schears GJ (2015) Extracorporeal membrane oxygenation support in postcardiotomy elderly patients: the mayo clinic experience. Ann Thorac Surg 99(6):2053–2060. https://doi.org/10.1016/j.athoracsur.2014.11.075. (Epub 2015 Apr 10. PMID: 25865760)
Mariani S, Heuts S, BCT v B, Di Mauro M, Wiedemann D, Saeed D, Pozzi M, Loforte A, Boeken U, Samalavicius R, Bounader K, Hou X, JJH B, Buscher H, Salazar L, Meyns B, Herr D, MLS M, Sponga S, MacLaren G, Russo C, Formica F, Sakiyalak P, Fiore A, Camboni D, Raffa GM, Diaz R, Wang IW, Jung JS, Belohlavek J, Pellegrino V, Bianchi G, Pettinari M, Barbone A, Garcia JP, Shekar K, GJR W, Lorusso R, PELS-1 Investigators * (2023) Patient and management variables associated with survival after postcardiotomy extracorporeal membrane oxygenation in adults: the PELS-1 multicenter cohort study. J Am Heart Assoc 12(14):e029609. https://doi.org/10.1161/JAHA.123.029609. (Epub 2023 Jul 8. PMID: 37421269; PMCID: PMC10382118)
Acknowledgements
Not applicable.
Funding
The authors did not receive any funds for the study or publication.
Author information
Authors and Affiliations
Contributions
ML participated in study design, data collection, statistical analysis, and manuscript writing. EH, PM, MGL, and MJM participated in data collection and interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethical committee of King Faisal Heart Center, was given a reference number (2191042) and waived from specific consent as there is no personally identifiable data or photos.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laimoud, M., Hakami, E., Machado, P. et al. Appropriate timing of veno-arterial extracorporeal membrane oxygenation initiation after cardiac surgery. Cardiothorac Surg 32, 2 (2024). https://doi.org/10.1186/s43057-023-00120-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43057-023-00120-y