Abstract
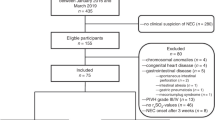
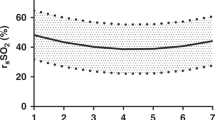
Infants with critical congenital heart disease, especially patients with a single-ventricle (SV) physiology, are at increased risk for the development of necrotizing enterocolitis (NEC). Decreased splanchnic oxygen delivery may contribute to the development of NEC and may be detected by regional oximetry (rSO2) via splanchnic near-infrared spectroscopy (NIRS). This prospective study enrolled 64 neonates undergoing biventricular (BV) repair or SV palliation for CHD and monitored postoperative splanchnic rSO2 before and during initiation of enteral feedings to determine whether changes in rSO2 are associated with risk of NEC. Suspected or proven NEC was observed in 32 % (11/34) of the SV subjects and 0 % (0/30) of the BV subjects (p = 0.001). Compared with the BV subjects, the SV palliated subjects had significantly lower splanchnic rSO2 before and during initiation of enteral feedings, but the groups showed no difference after correction for lower pulse oximetry (SpO2) in the SV group. The clinical parameters were similar among the SV subjects with and without NEC except for cardiopulmonary bypass times, which were longer for the patients who experienced NEC (126 vs 85 min; p = 0.03). No difference was observed in splanchnic rSO2 or in the SpO2–rSO2 difference between the SV subjects with and without NEC. Compared with the patients who had suspected or no NEC, the subjects with proven NEC had a lower average splanchnic rSO2 (32.6 vs 47.0 %; p = 0.05), more time with rSO2 less than 30 % (48.8 vs 6.7 %; p = 0.04) at one-fourth-volume feeds, and more time with SpO2–rSO2 exceeding 50 % (33.3 vs 0 %; p = 0.03) before feeds were initiated. These data suggest that splanchnic NIRS may be a useful tool for assessing risk of NEC, especially in patients with an SV physiology.


Similar content being viewed by others

References
Bhalala US, Nishisaki A, McQueen D, Bird GL, Morrison WE, Nadkarni VM, Nathan M, Starr JP (2012) Change in regional (somatic) near-infrared spectroscopy is not a useful indicator of clinically detectable low cardiac output in children after surgery for congenital heart defects. Pediatr Crit Care Med 13:529–534. doi:10.1097/PCC.0b013e3182389531
Carlo WF, Kimball TR, Michelfelder EC, Border WL (2007) Persistent diastolic flow reversal in abdominal aortic Doppler-flow profiles is associated with an increased risk of necrotizing enterocolitis in term infants with congenital heart disease. Pediatrics 119:330–335. doi:10.1542/peds.2006-2640
Cortez J, Gupta M, Amaram A, Pizzino J, Sawhney M, Sood BG (2011) Noninvasive evaluation of splanchnic tissue oxygenation using near-infrared spectroscopy in preterm neonates. J Matern Fetal Neonatal Med 24:574–582. doi:10.3109/14767058.2010.511335
Cozzi C, Aldrink J, Nicol K, Nicholson L, Cua C (2013) Intestinal location of necrotizing enterocolitis among infants with congenital heart disease. J Perinatol. doi:10.1038/jp.2013.49
Davies RR, Carver SW, Schmidt R, Keskeny H, Hoch J, Pizarro C (2013) Gastrointestinal complications after stage I Norwood versus hybrid procedures. Ann Thorac Surg 95:189–195. doi:10.1016/j.athoracsur.2012.05.130 discussion 195–186
Fortune PM, Wagstaff M, Petros AJ (2001) Cerebro-splanchnic oxygenation ratio (CSOR) using near-infrared spectroscopy may be able to predict splanchnic ischaemia in neonates. Intensiv Care Med 27:1401–1407
Gaies M, Gurney J, Yen A, Napoili M, Gajarski R, Ohye R, Charpie J, Hirsch J (2010) Vasoactive–inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11:234–238
Harrison AM, Davis S, Reid JR, Morrison SC, Arrigain S, Connor JT, Temple ME (2005) Neonates with hypoplastic left heart syndrome have ultrasound evidence of abnormal superior mesenteric artery perfusion before and after modified Norwood procedure. Pediatr Crit Care Med 6:445–447. doi:10.1097/01.pcc.0000163674.53466.ca
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI (2002) Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 123:110–118
Kaufman J, Almodovar MC, Zuk J, Friesen RH (2008) Correlation of abdominal site near-infrared spectroscopy with gastric tonometry in infants following surgery for congenital heart disease. Pediatr Crit Care Med 9:62–68. doi:10.1097/01.pcc.0000298640.47574.da
Kim JW, Shin WJ, Park I, Chung IS, Gwak M, Hwang GS (2013) Splanchnic oxygen saturation immediately after weaning from cardiopulmonary bypass can predict early postoperative outcomes in children undergoing congenital heart surgery. Pediatr Cardiol. doi:10.1007/s00246-013-0824-z
Li J, Van Arsdell GS, Zhang G, Cai S, Humpl T, Caldarone CA, Holtby H, Redington AN (2006) Assessment of the relationship between cerebral and splanchnic oxygen saturations measured by near-infrared spectroscopy and direct measurements of systemic haemodynamic variables and oxygen transport after the Norwood procedure. Heart 92:1678–1685. doi:10.1136/hrt.2005.087270
Malagon I, Onkenhout W, Klok G, van der Poel PF, Bovill JG, Hazekamp MG (2005) Gut permeability in paediatric cardiac surgery. Br J Anaesth 94:181–185. doi:10.1093/bja/aei014
Malagon I, Onkenhout W, Klok M, van der Poel PF, Bovill JG, Hazekamp MG (2005) Gut permeability in neonates after a stage 1 Norwood procedure. Pediatr Crit Care Med 6:547–549
Mallick IH, Yang W, Winslet MC, Seifalian AM (2004) Ischemia-reperfusion injury of the intestine and protective strategies against injury. Dig Dis Sci 49:1359–1377
Matcher SJ, Cooper CE (1994) Absolute quantification of deoxyhemoglobin concentration in tissue near-infrared spectroscopy. Phys Med Biol 39:1295–1312
McElhinney DB, Hedrick HL, Bush DM, Pereira GR, Stafford PW, Gaynor JW, Spray TL, Wernovsky G (2000) Necrotizing enterocolitis in neonates with congenital heart disease: risk factors and outcomes. Pediatrics 106:1080–1087
Mukherjee D, Zhang Y, Chang DC, Vricella LA, Brenner JI, Abdullah F (2010) Outcomes analysis of necrotizing enterocolitis within 11,958 neonates undergoing cardiac surgical procedures. Arch Surg 145:389–392. doi:10.1001/archsurg.2010.39
Schulz G, Weiss M, Bauersfeld U, Teller J, Haensse D, Bucher HU, Baenziger O (2002) Liver tissue oxygenation as measured by near-infrared spectroscopy in the critically ill child in correlation with central venous oxygen saturation. Intensive Care Med 28:184–189. doi:10.1007/s00134-001-1182-5
Silane MF, Symchych PS (1977) Necrotizing enterocolitis after cardiac surgery: a local ischemic lesion? Am J Surg 133:373–376
Stapleton GE, Eble BK, Dickerson HA, Andropoulos DB, Chang AC (2007) Mesenteric oxygen desaturation in an infant with congenital heart disease and necrotizing enterocolitis. Tex Heart Inst J 34:442–444
Acknowledgments
Support for this study included the Amendt-Heller Award for Newborn Research from the Department of Pediatrics at the University of Michigan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DeWitt, A.G., Charpie, J.R., Donohue, J.E. et al. Splanchnic Near-Infrared Spectroscopy and Risk of Necrotizing Enterocolitis After Neonatal Heart Surgery. Pediatr Cardiol 35, 1286–1294 (2014). https://doi.org/10.1007/s00246-014-0931-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-014-0931-5